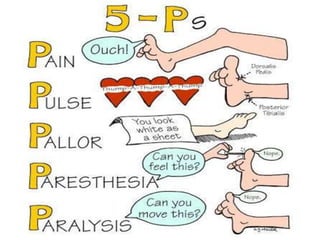
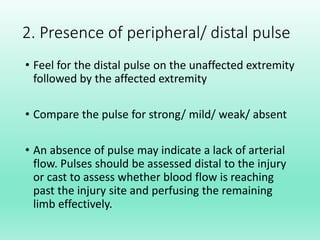
This document discusses the purpose and components of a neurovascular assessment. A neurovascular assessment is performed to assess nerve function and blood circulation in the body to detect potential complications such as compartment syndrome. The assessment involves evaluating pain, peripheral pulses, pallor, paresthesia, and paralysis. Compartment syndrome occurs when excessive pressure builds up within a compartment due to swelling or bleeding and can be identified by the 6 P's: pain, pulses, pallor, paresthesia, pressure, and paralysis. A neurovascular assessment is important for monitoring injuries and potential complications.