This document provides information on neurovascular assessments, including:
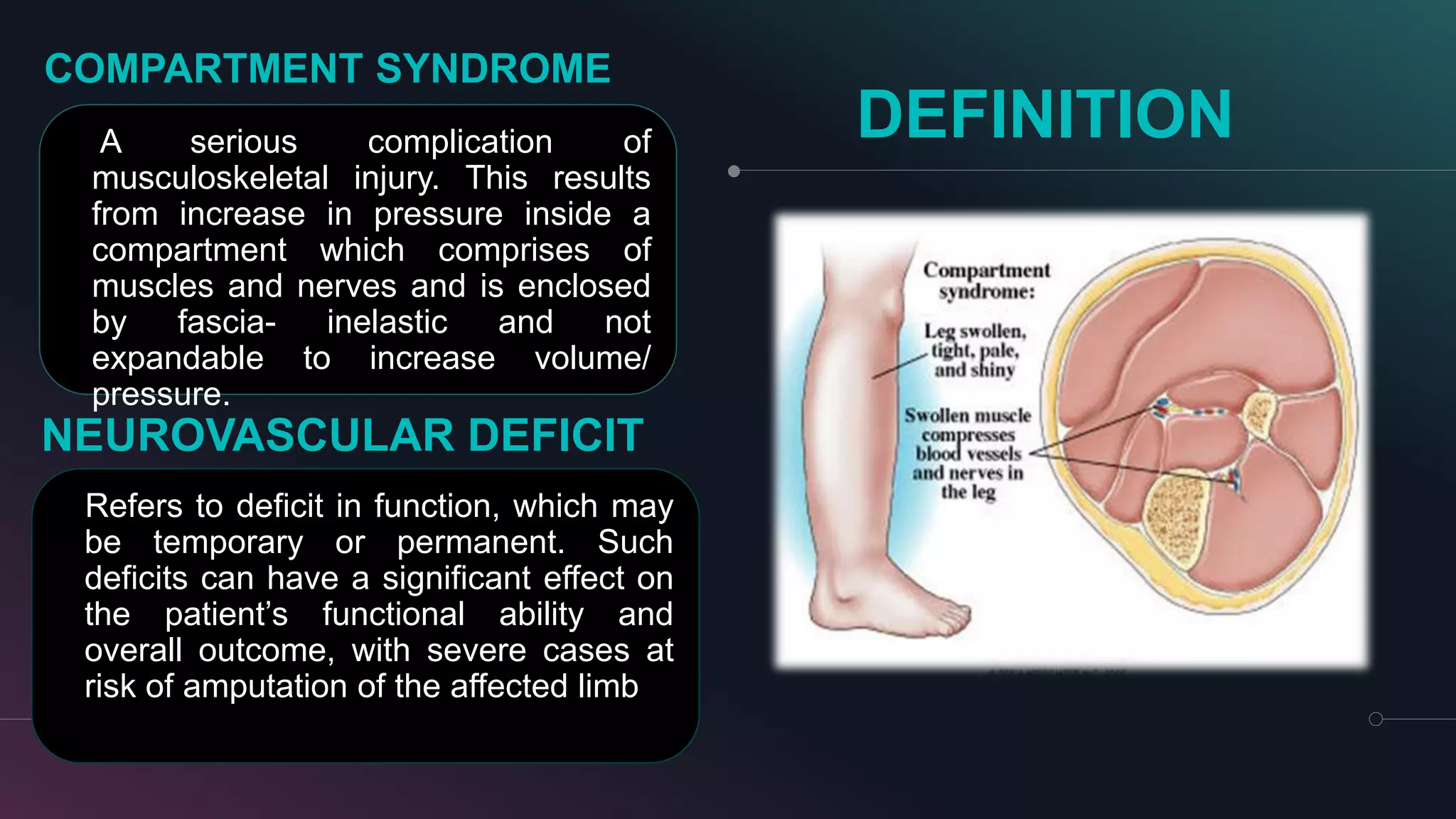
- The purpose is to assess nerve and blood circulation in the body to detect potential issues like compartment syndrome.
- Key terms are defined, like neurovascular, compartment syndrome, and neurovascular deficit.
- The policy outlines when assessments should be done, like after injuries or procedures. It also lists the mandatory assessment parameters.
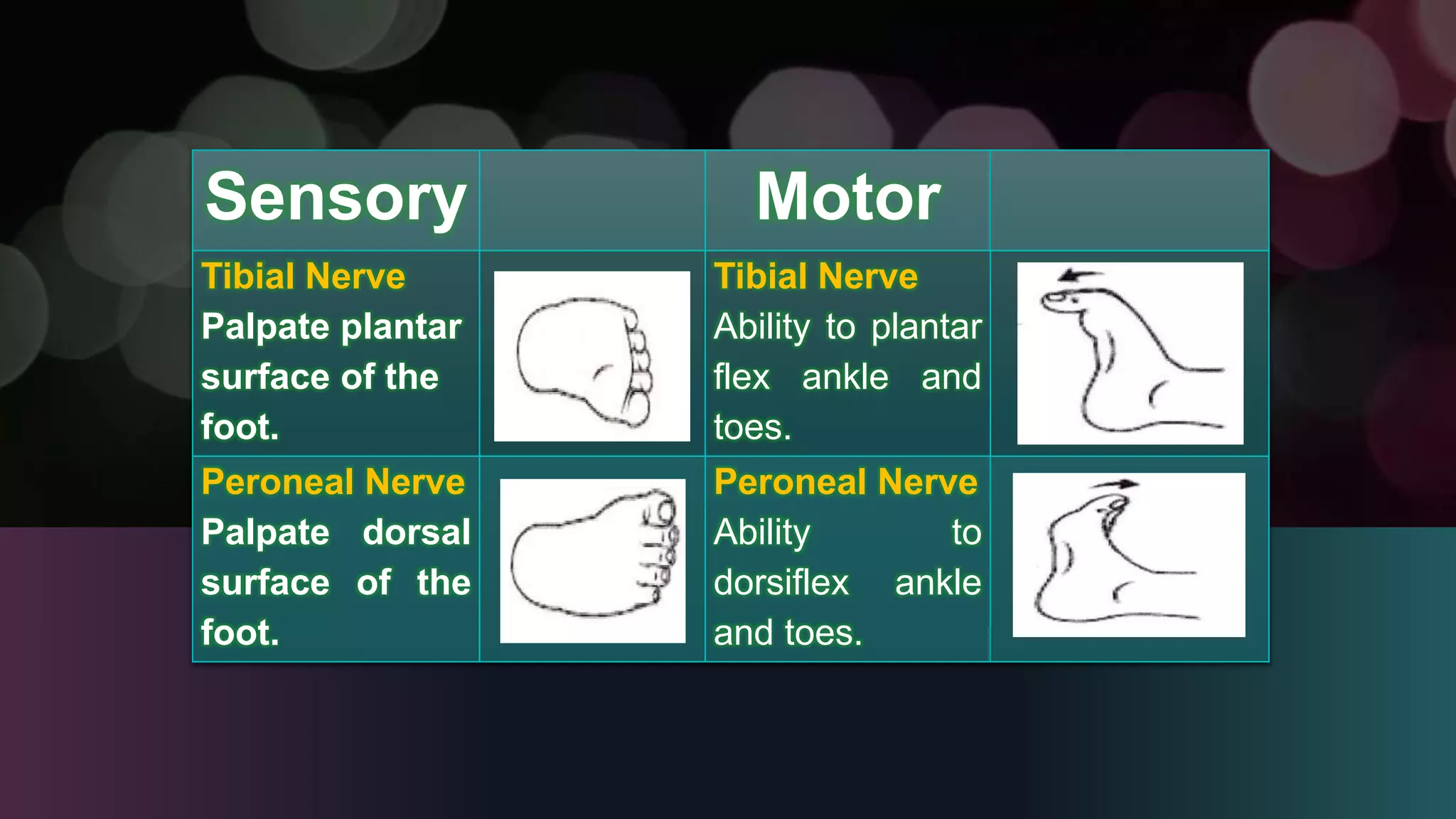
- The procedure explains how to conduct the assessment, including checking pulse, sensation, color, warmth, swelling, and range of motion. It also provides examples of assessing specific nerves.