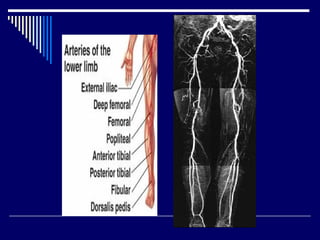
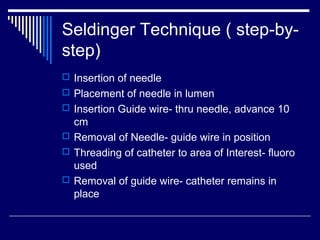
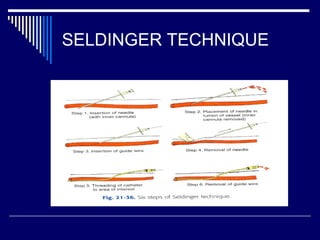
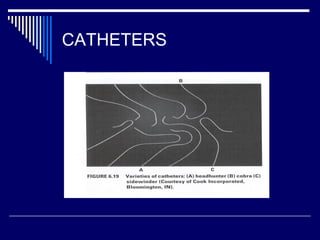
1. Angiography is performed by inserting a catheter into an artery or vein using the Seldinger technique, which involves inserting a needle and guidewire before threading the catheter.
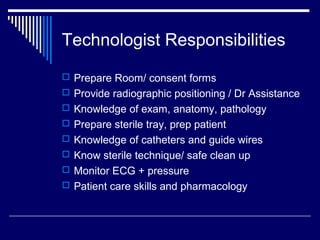
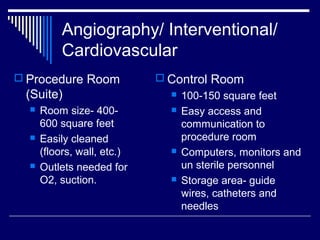
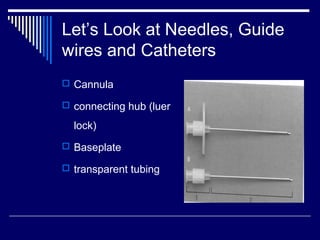
2. The angiography team includes a radiologist, nurse, and technologists who prepare equipment like catheters, guidewires, and injectors to visualize blood vessels and perform interventional procedures.
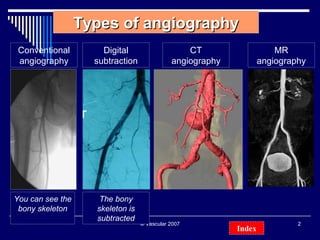
3. Digital subtraction angiography uses computer algorithms to subtract bone structures from images, clearly showing blood vessel anatomy for diagnostic and therapeutic purposes like angioplasty.