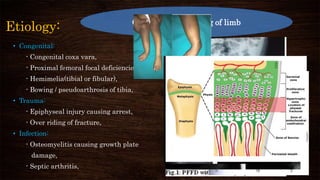
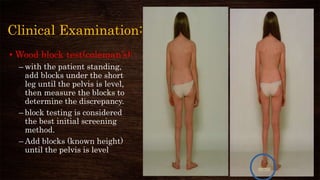
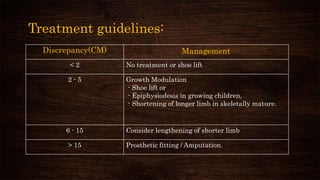
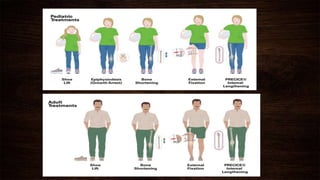
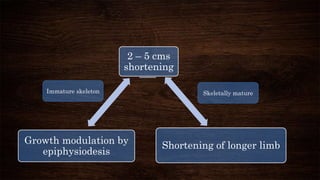
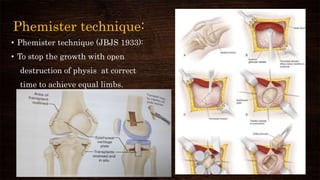
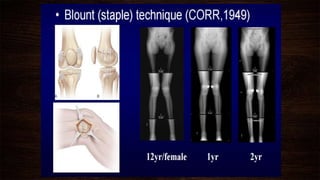
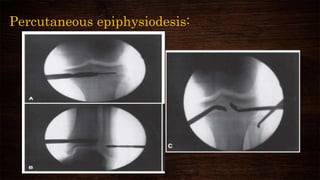
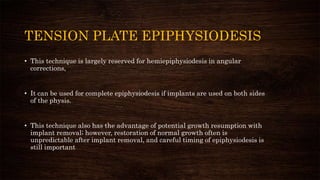
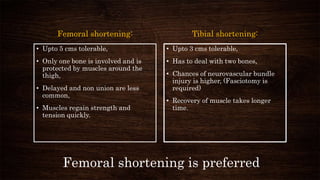
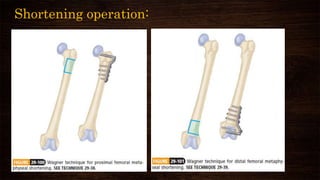
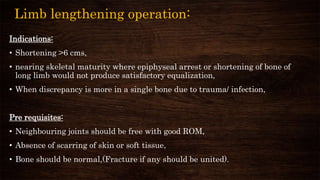
Limb length discrepancy can be structural or functional. For structural discrepancies between 2-5 cm in growing children, epiphysiodesis is commonly used to modulate growth. Epiphysiodesis involves arresting growth in the long limb's growth plate to allow the short limb time to catch up. It is a relatively simple procedure but risks include under or overcorrection and asymmetric growth arrest. For discrepancies over 5 cm or in skeletally mature individuals, shortening the long limb is preferred over lengthening the short limb.