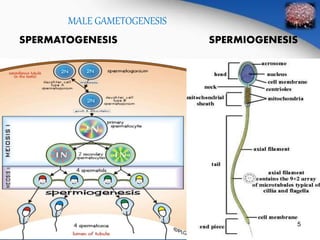
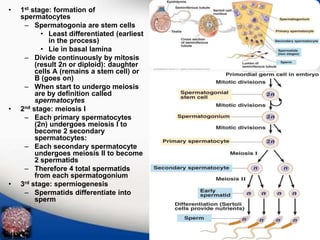
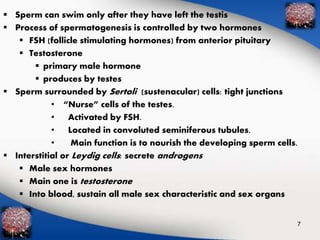
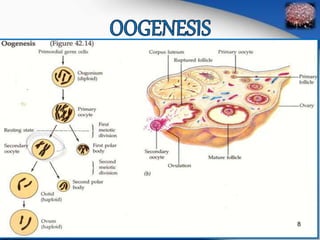
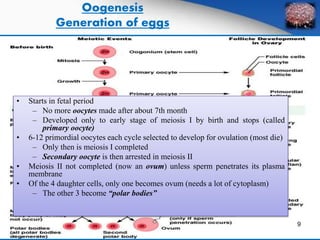
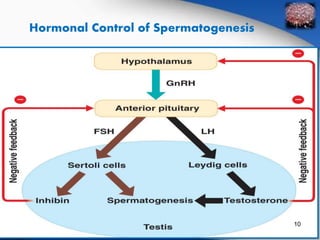
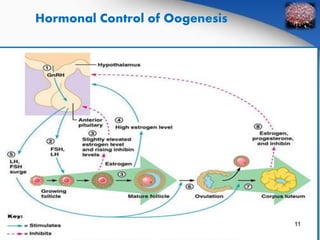
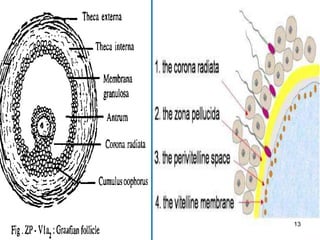
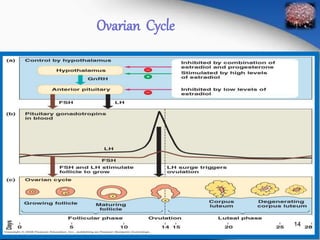
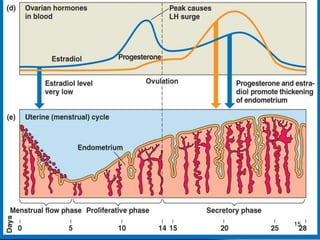
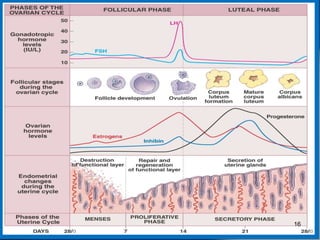
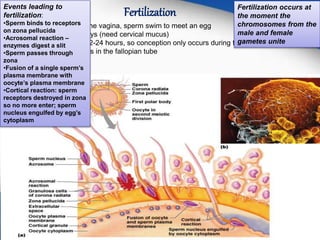
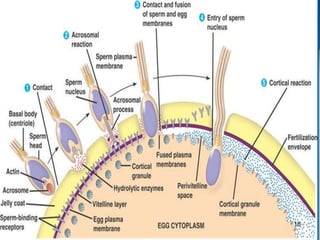
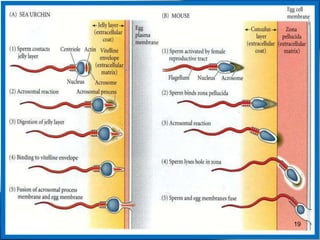
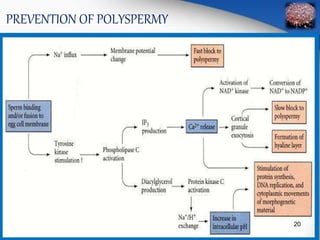
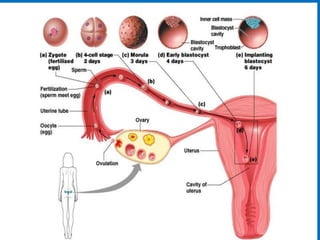
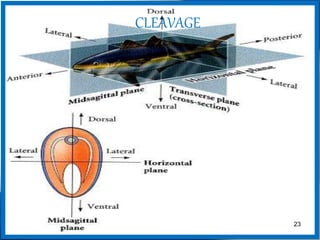
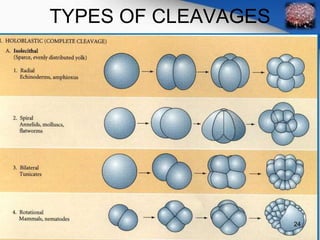
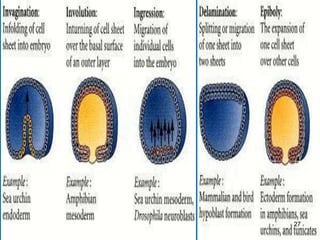
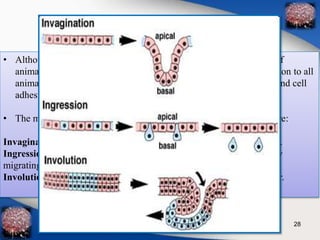
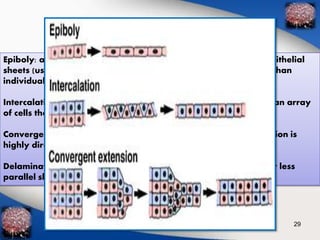
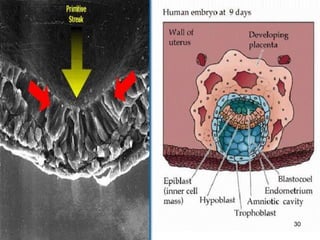
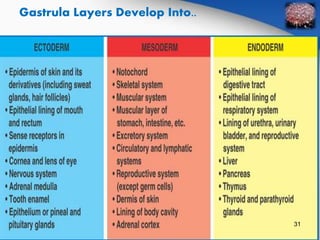
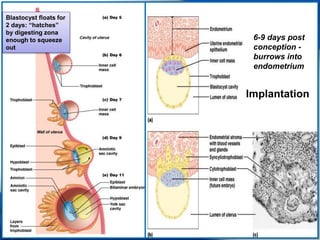
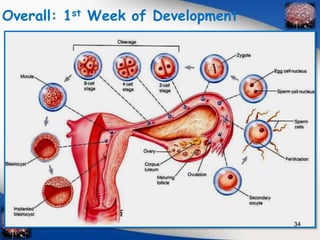
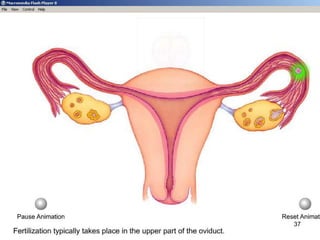
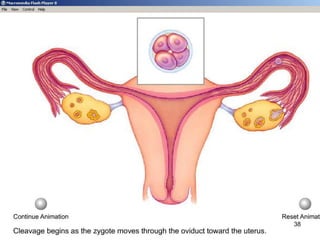
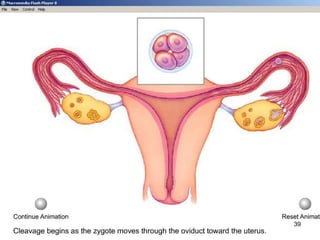
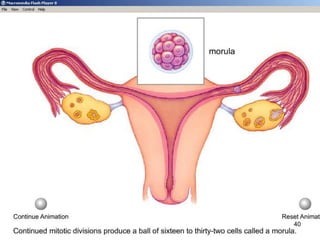
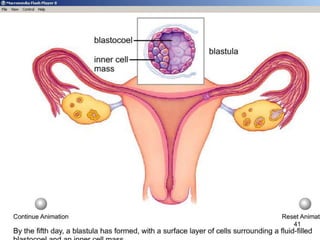
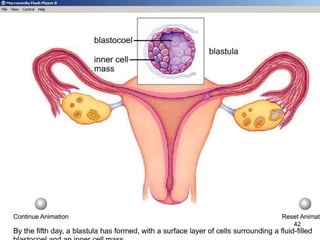
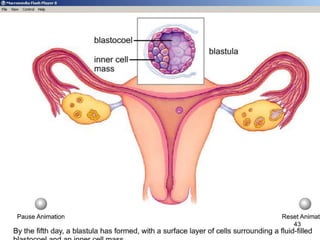
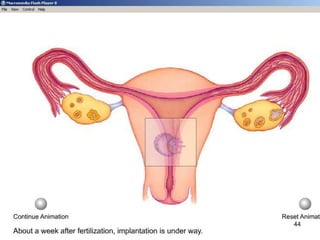
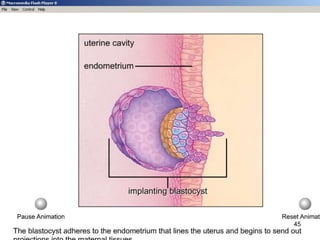
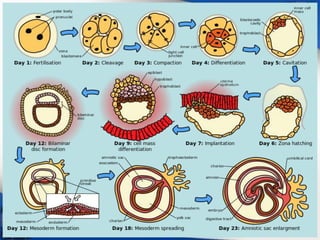
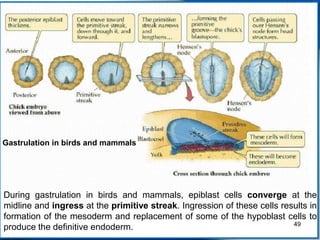
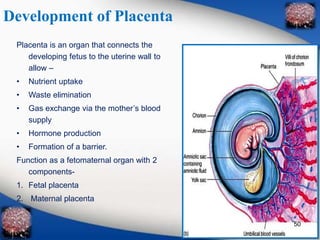
The document outlines gametogenesis, fertilization, and embryonic development in humans, discussing the processes of spermatogenesis and oogenesis, and their hormonal controls. It details fertilization events, early cleavage stages, gastrulation, and the subsequent formation of the embryo and placenta. Key differences between male and female gametogenesis, as well as the roles of various cellular movements and stages during development, are also presented.