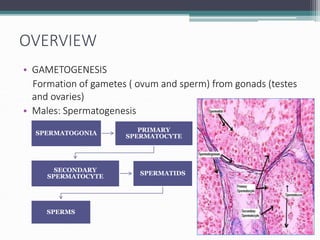
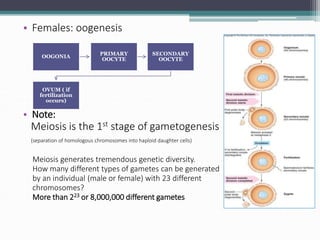
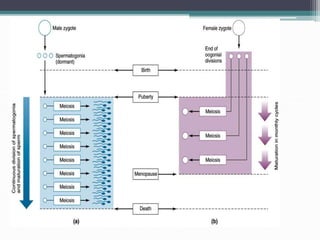
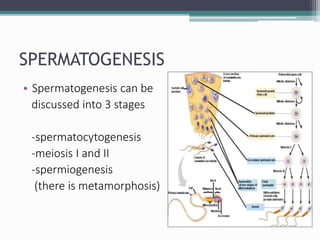
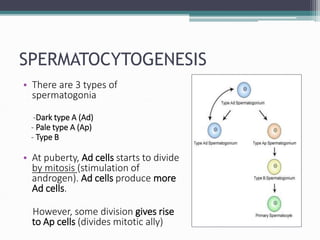
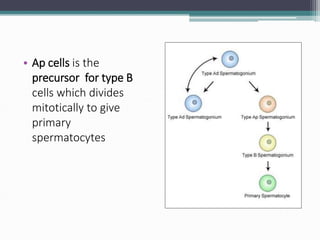
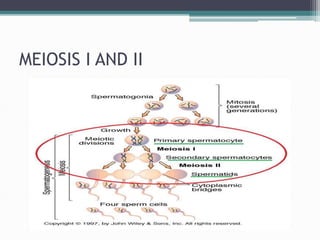
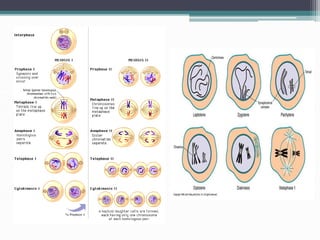
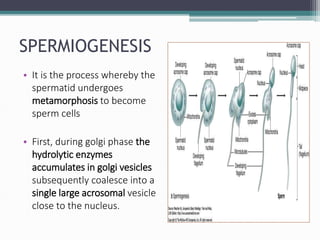
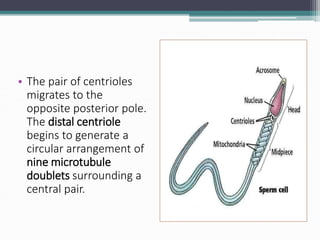
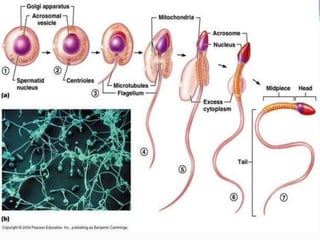
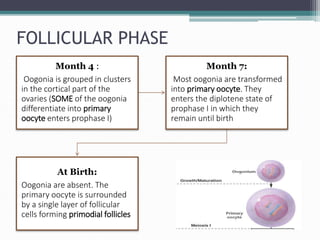
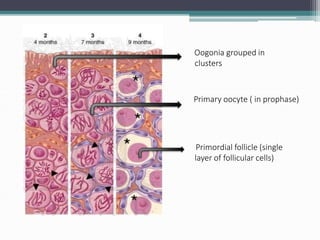
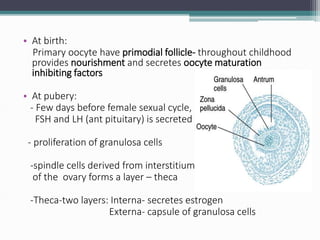
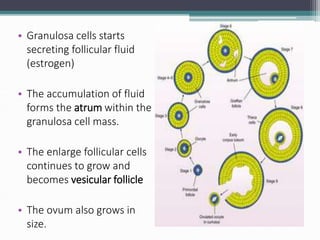
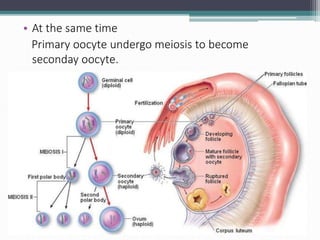
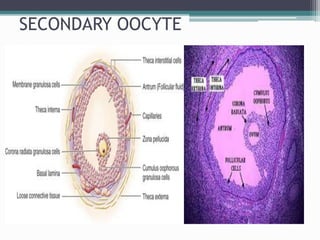
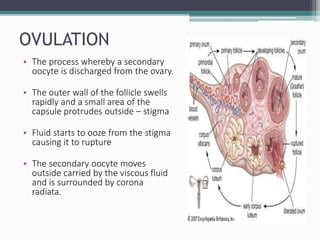
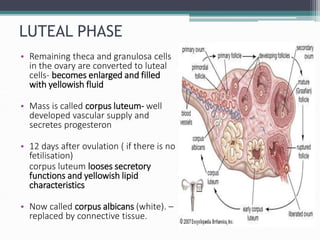
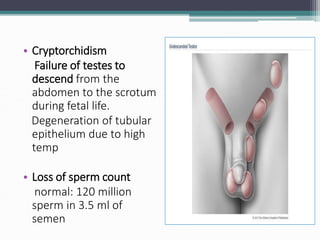
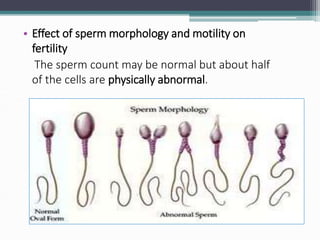
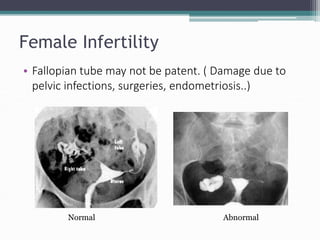
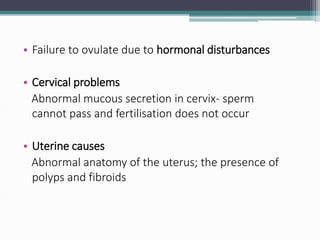
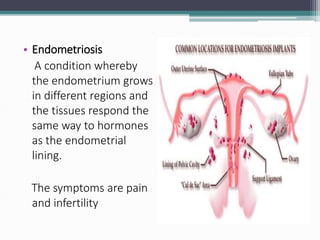
Gametogenesis is the process of forming gametes (eggs and sperm) from gonads through meiosis. In males, spermatogenesis occurs in the testes through spermatocytogenesis, meiosis I and II, and spermiogenesis. In females, oogenesis occurs in the ovaries through follicular development, ovulation, and the luteal phase. Infertility can result from problems with gametogenesis like inflammation of the testes or failure of the ovaries to ovulate, as well as issues with the fallopian tubes, cervix, or uterus.