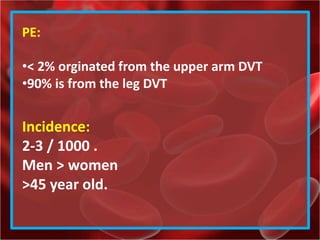
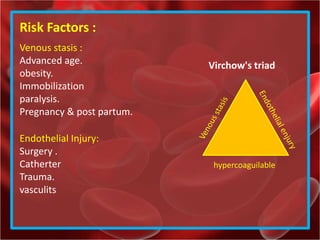
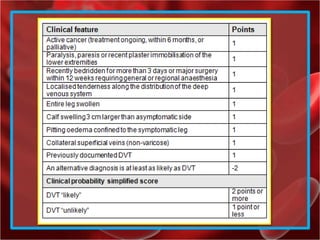
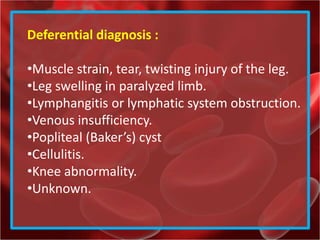
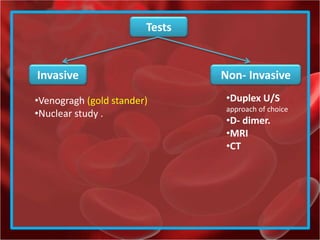
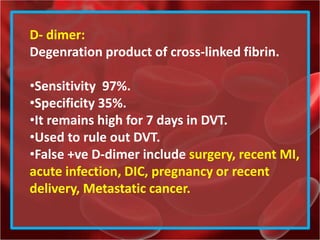
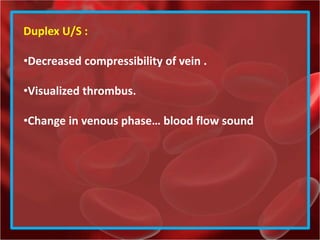
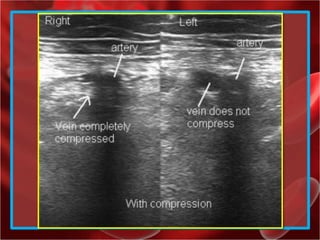
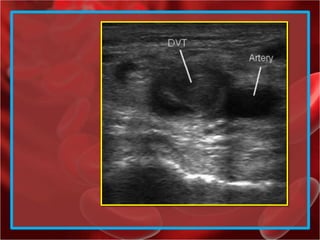
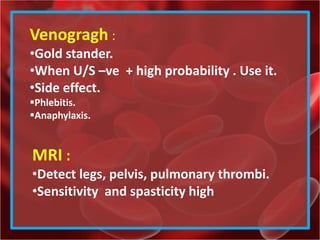
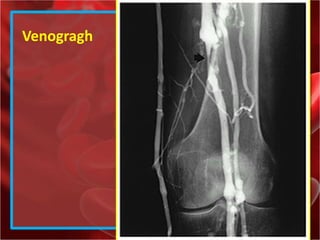
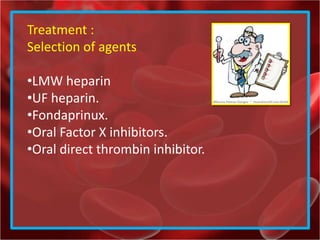
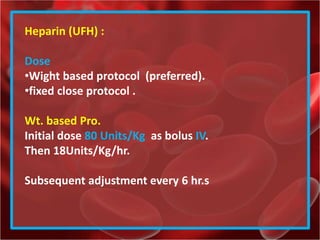
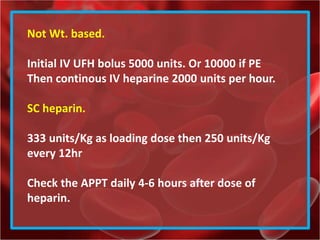
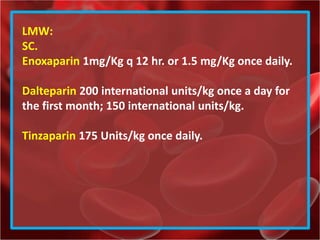
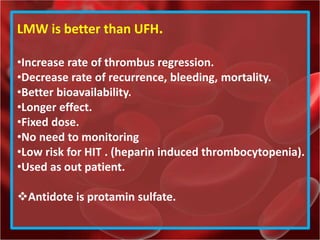
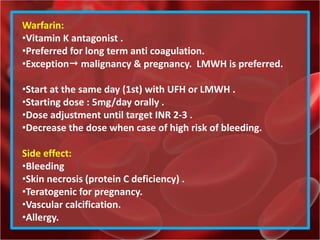
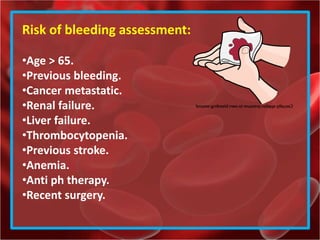
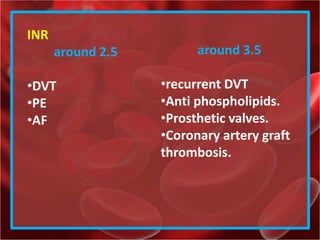
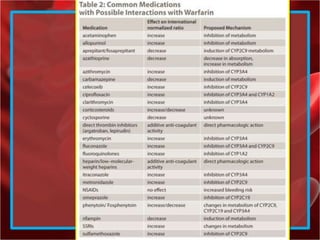
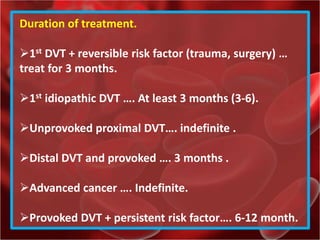
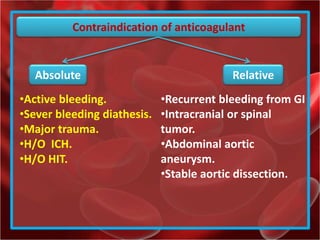
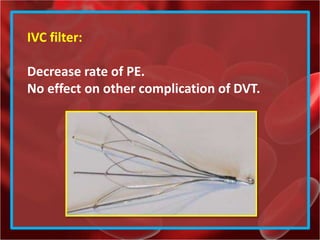
The document provides a comprehensive overview of deep vein thrombosis (DVT), including its definition, risk factors, symptoms, and diagnostic methods. It elaborates on the types of DVT, treatment options, and the importance of anticoagulation therapy, alongside mentioning possible complications and contraindications for anticoagulants. Furthermore, it describes the role of ultrasound and D-dimer tests in diagnosis, as well as the management strategies for various patient scenarios.