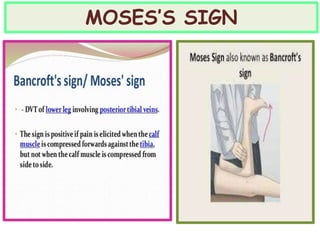
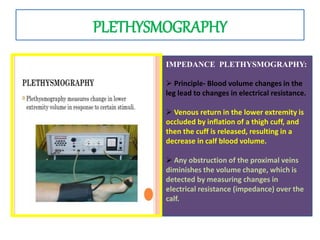
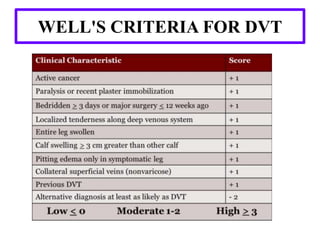
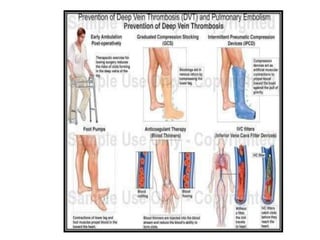
Deep vein thrombosis (DVT) formation in the legs is a common complication. Risk factors include immobility, surgery, cancer, and genetic conditions. Symptoms may include leg swelling, pain, and skin changes. Ultrasound is the primary diagnostic test. Treatment involves blood thinners like heparin, low molecular weight heparin, and warfarin to prevent clots from growing or breaking off. Compression stockings also help. Prevention focuses on early ambulation and mechanical or pharmacological prophylaxis for high risk patients. Complications include bleeding, thrombocytopenia, and post-thrombotic syndrome. Nursing care monitors for signs of clot progression or medication side effects while educating on prevention