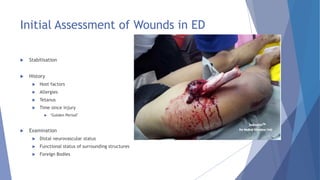
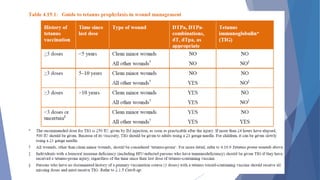
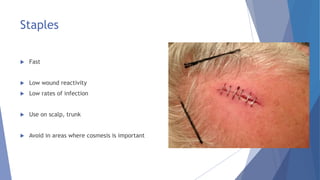
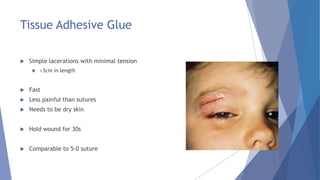
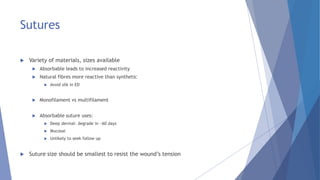
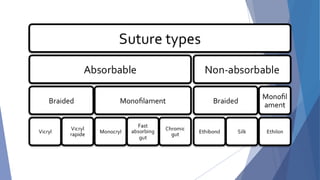
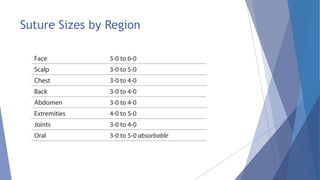
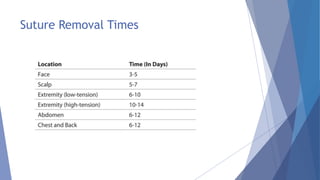
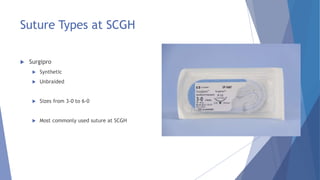
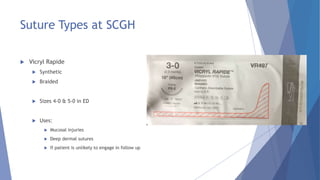
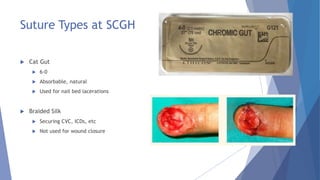
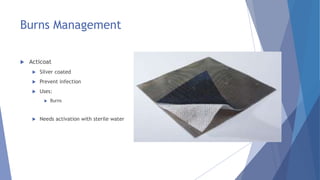
This document provides guidance on wound management and closure techniques in the emergency department. It discusses assessing wounds, types of closure like sutures, staples and glue. Suture techniques like simple interrupted and mattress styles are covered. Finally, it reviews wound dressings and their appropriate uses for situations like burns, bleeding, or to promote healing. The goal is to close wounds effectively while preventing infection and promoting good cosmetic and functional recovery.