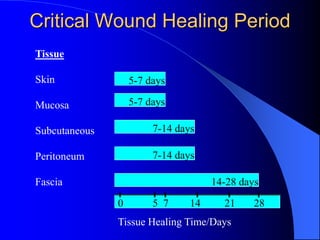
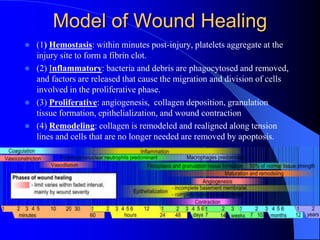
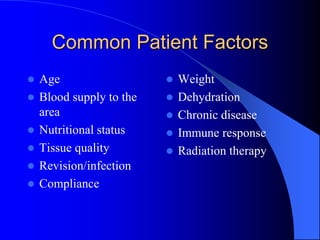
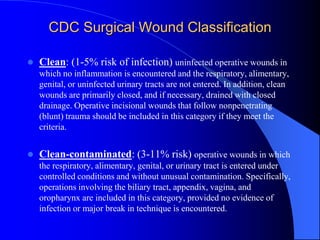
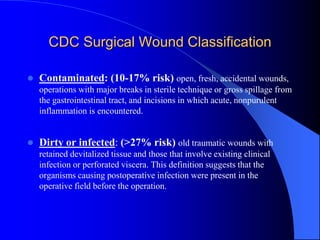
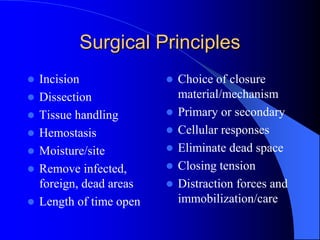
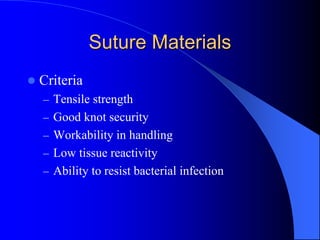
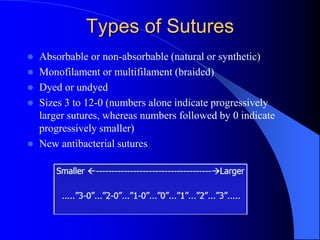
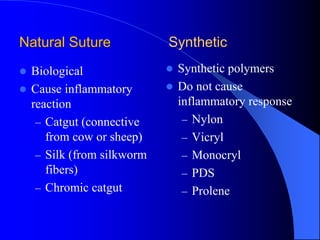
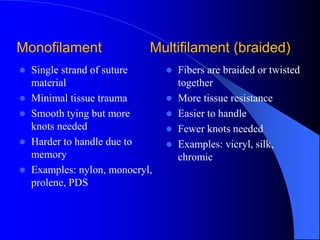
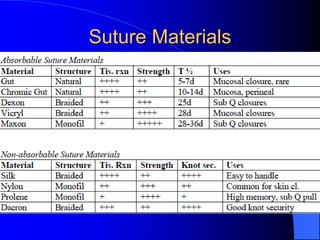
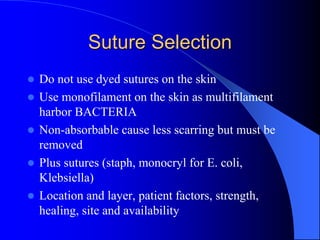
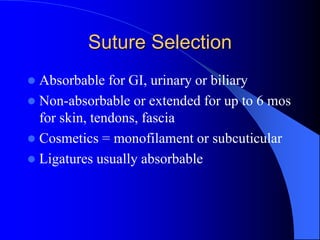
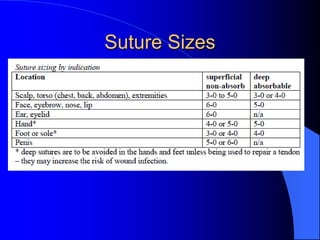
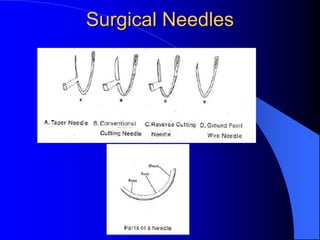
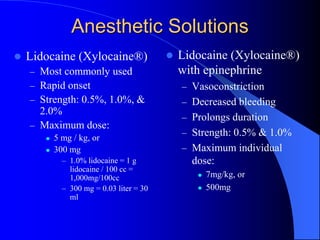
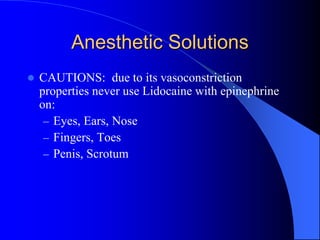
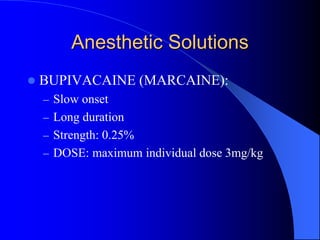
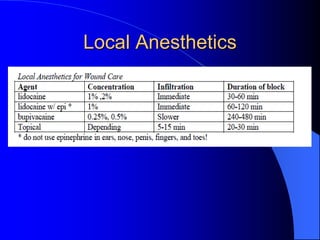
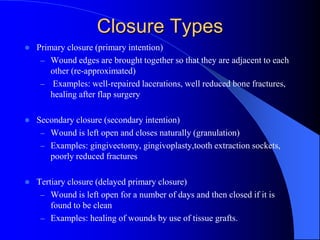
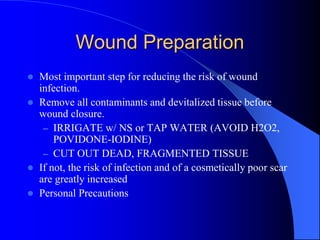
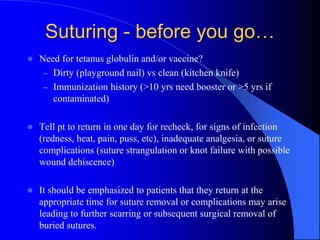
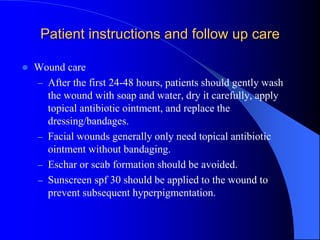
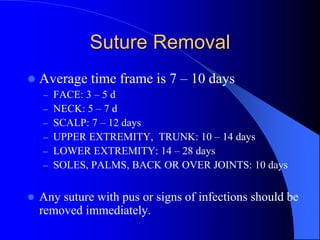
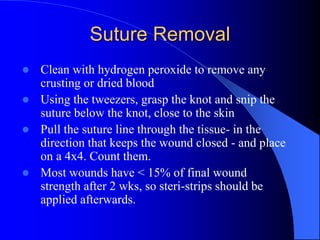
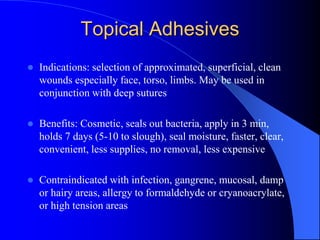
This document provides information on sutures and suturing for wound closure. It discusses wound healing timelines for different tissues, the four phases of wound healing, factors to consider for patients and wounds, wound classification, surgical principles, suture materials and types, needles, local anesthetics, wound evaluation and closure techniques. It also reviews guidelines for wound preparation, suturing techniques, patient instructions, and suture removal.