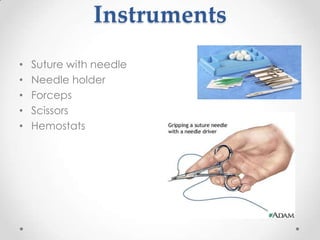
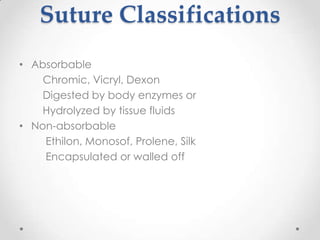
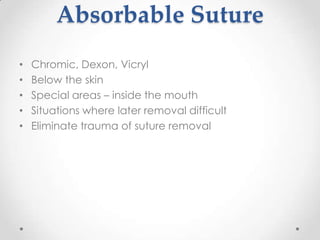
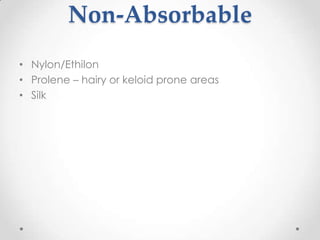
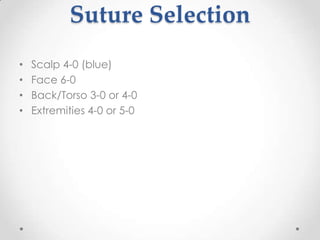
This document provides an overview and objectives for a basic suturing workshop for family practitioner students. It covers topics like wound evaluation and preparation, types of sutures and suturing techniques, wound cleansing and irrigation, and guidelines for using local anesthesia. The objectives are to discuss wound repair principles, explain local anesthesia concepts, and perform simple interrupted suture techniques. [/SUMMARY]