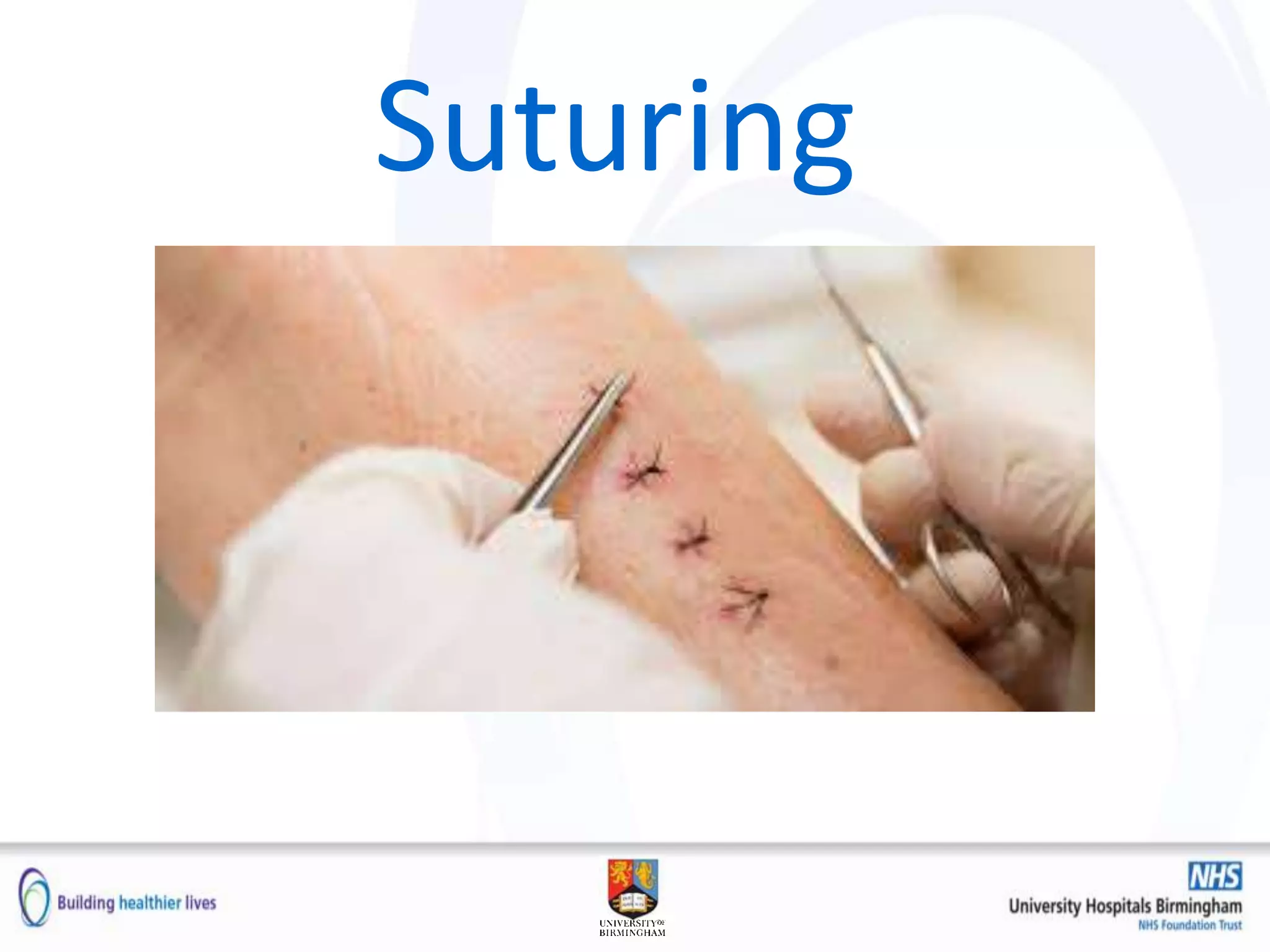
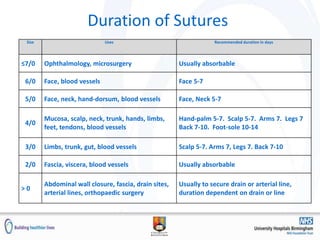
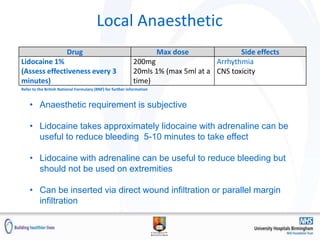
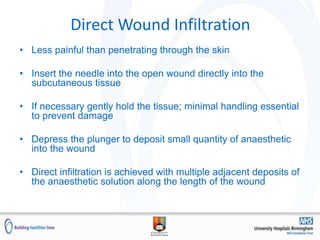
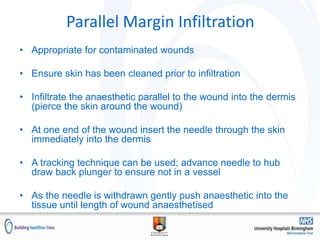
This document discusses suturing techniques and wound closure. It covers the stages of wound healing, indications and contraindications for suturing, types of suture materials, local anesthetic administration, and techniques for simple interrupted sutures and vertical mattress sutures. Alternative closure methods like steri strips and surgical glue are also reviewed. The goal of wound closure is healing without infection, scarring or deformity.