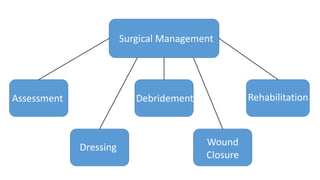
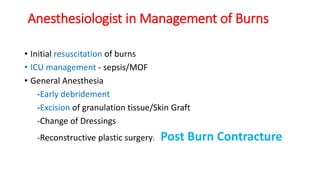
This document discusses the surgical management of burns. It covers assessment, dressing, debridement, wound closure, and rehabilitation. Key points include:
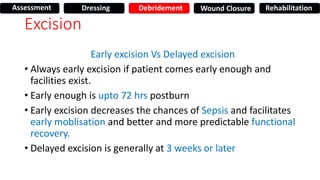
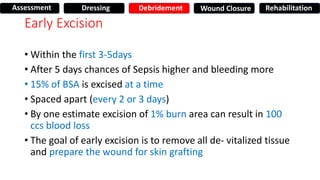
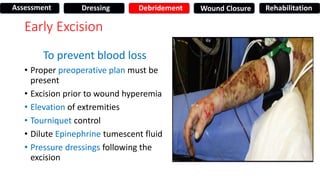
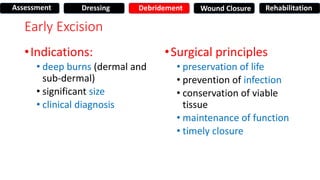
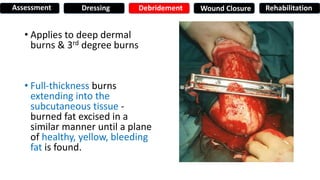
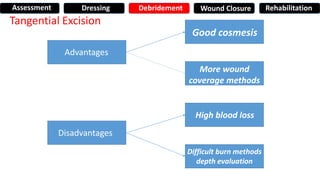
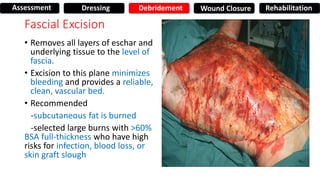
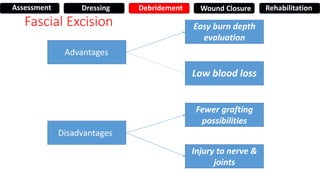
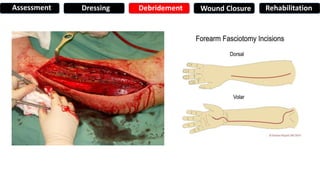
- Early excision within 72 hours is preferred to decrease risk of sepsis and facilitate healing. Excision can be done tangentially or down to the fascia.
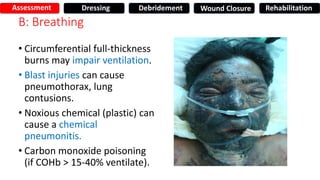
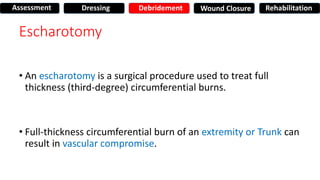
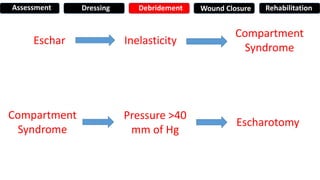
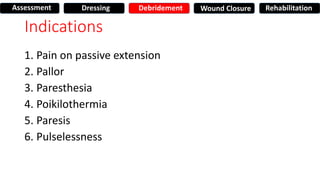
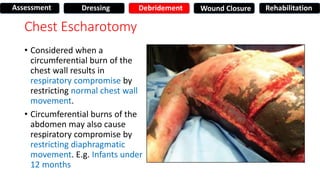
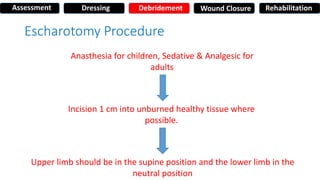
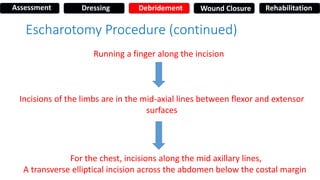
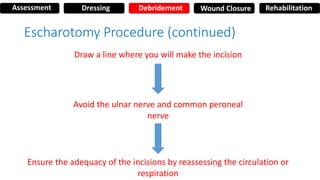
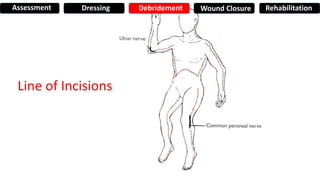
- Escharotomy may be needed for circumferential burns to relieve pressure.
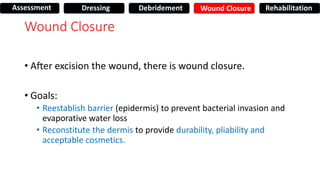
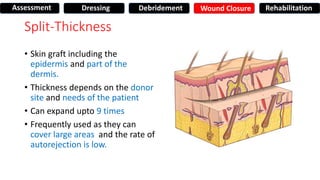
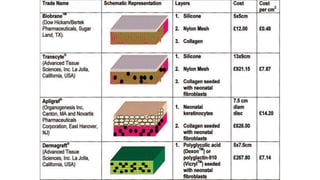
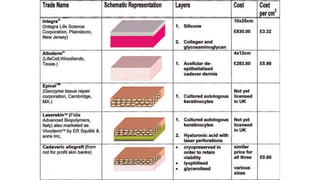
- Wounds are closed primarily with split-thickness skin grafts within 3-5 days of excision.
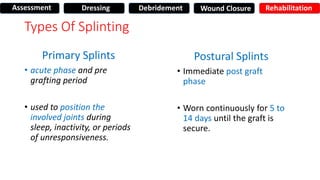
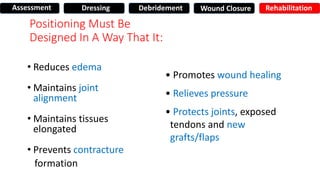
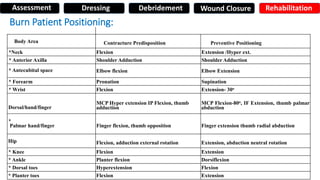
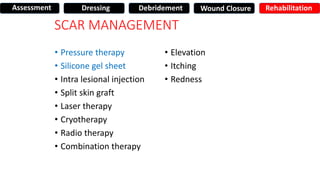
- Rehabilitation includes splinting to prevent contractures and scar management. Positioning is vital to optimize functional outcomes.
![Alhad Naragude
Final Year M.B.B.S [BJMC PUNE]
Guided By
Dr. Pawan Chumbale
M.S, MCh Plastic Surgery [SASSOON HOSPITAL, PUNE]
BURNS](https://image.slidesharecdn.com/7surgery-160810204332/75/BURNS-Surgical-Management-1-2048.jpg)