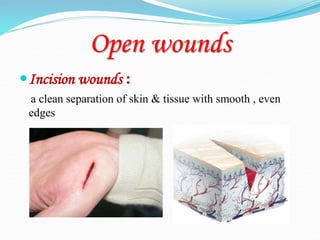
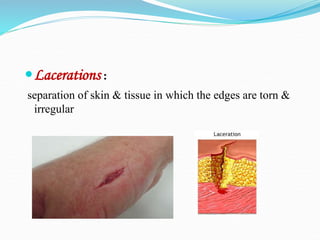
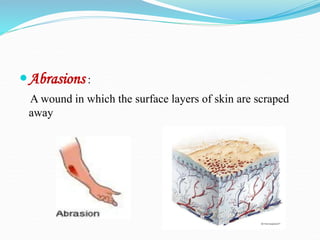
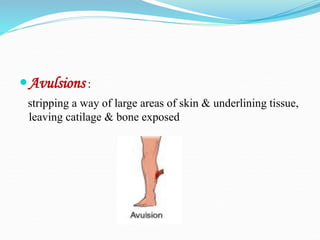
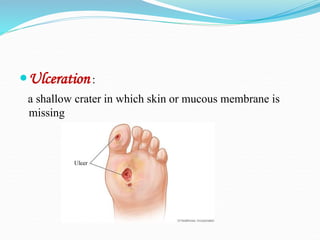
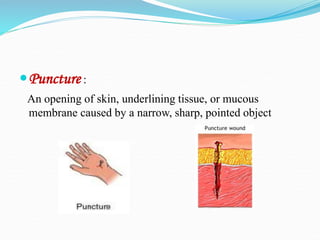
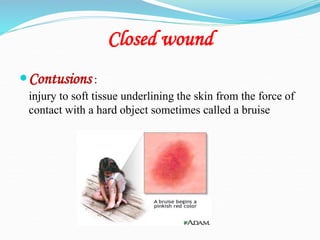
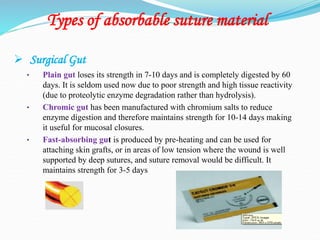
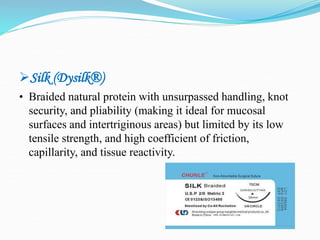
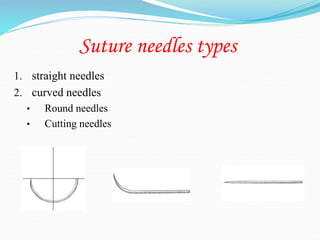
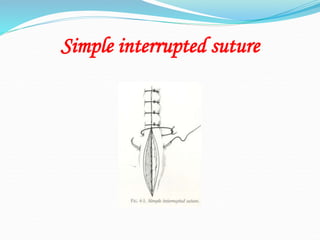
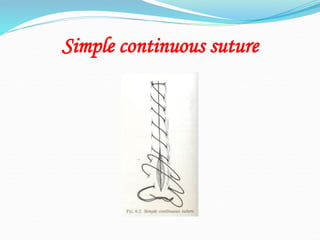
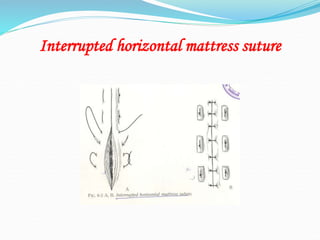
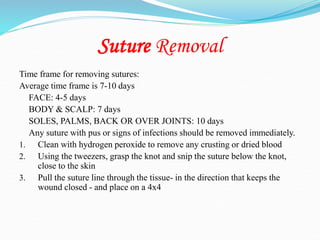
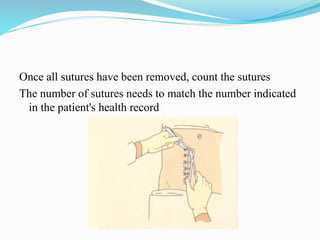
There are two basic types of wounds - open wounds where the skin is broken, and closed wounds where the skin is intact but the underlying tissue is damaged. Open wounds include incisions, lacerations, abrasions, avulsions, ulcers, and punctures. Closed wounds include contusions. Wound management involves techniques to promote healing such as dressings, drainage, bandages, sutures, and staples. Sutures are used to close wounds and come in absorbable and non-absorbable varieties made from materials like gut, polyglactin, and nylon. Selection depends on factors like tensile strength, tissue reactivity, and absorption time. Sutures are placed using techniques