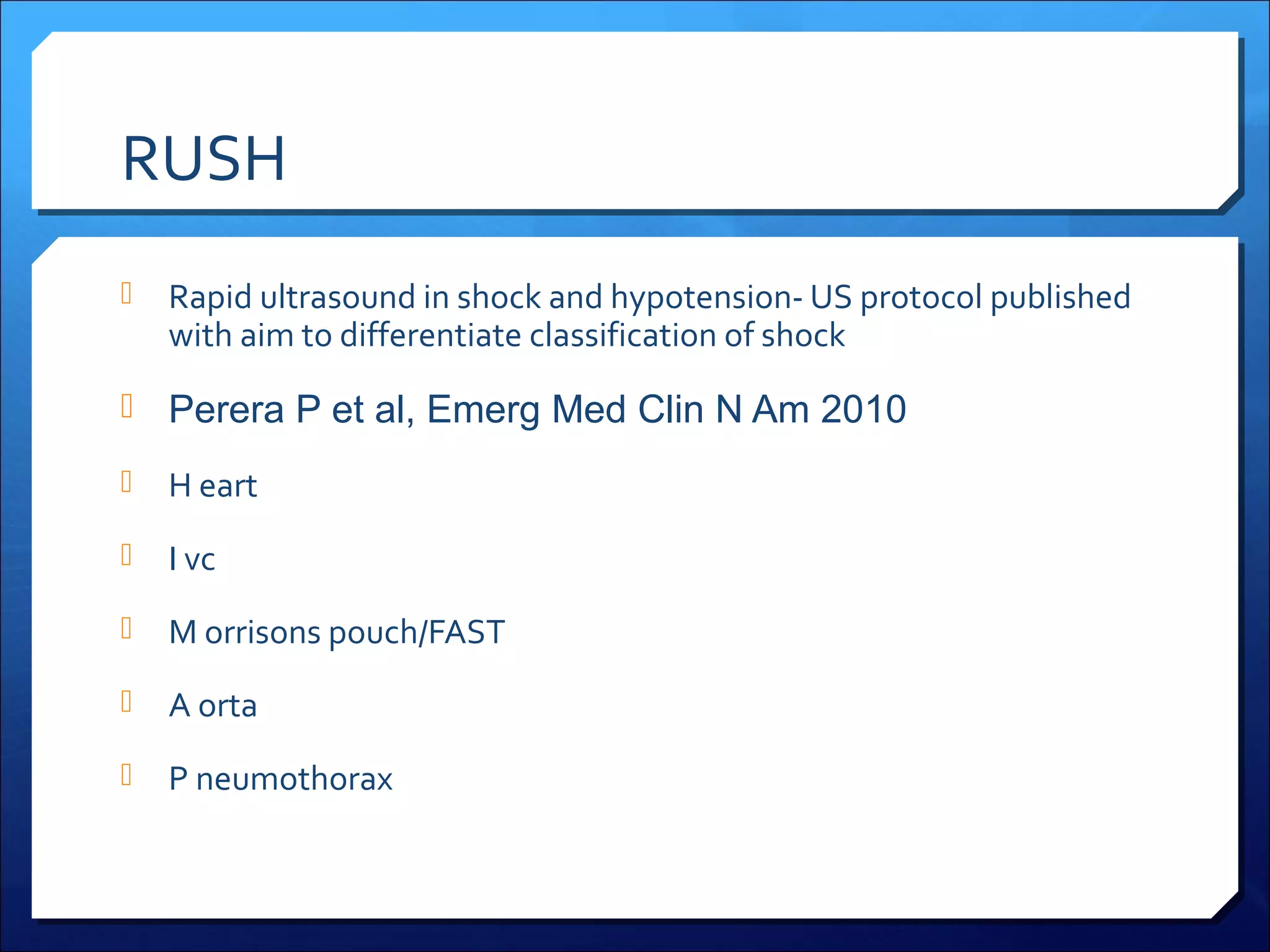
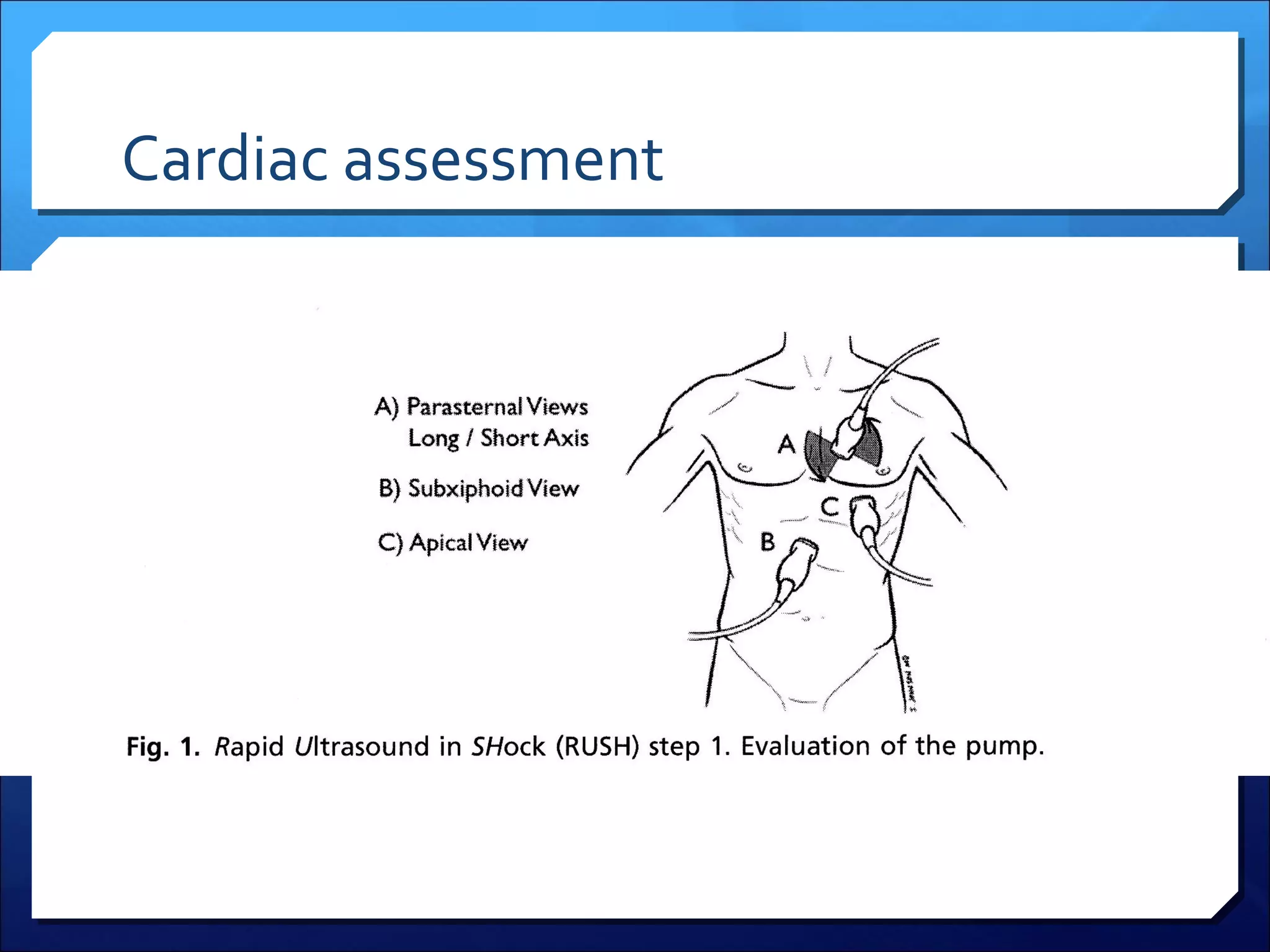
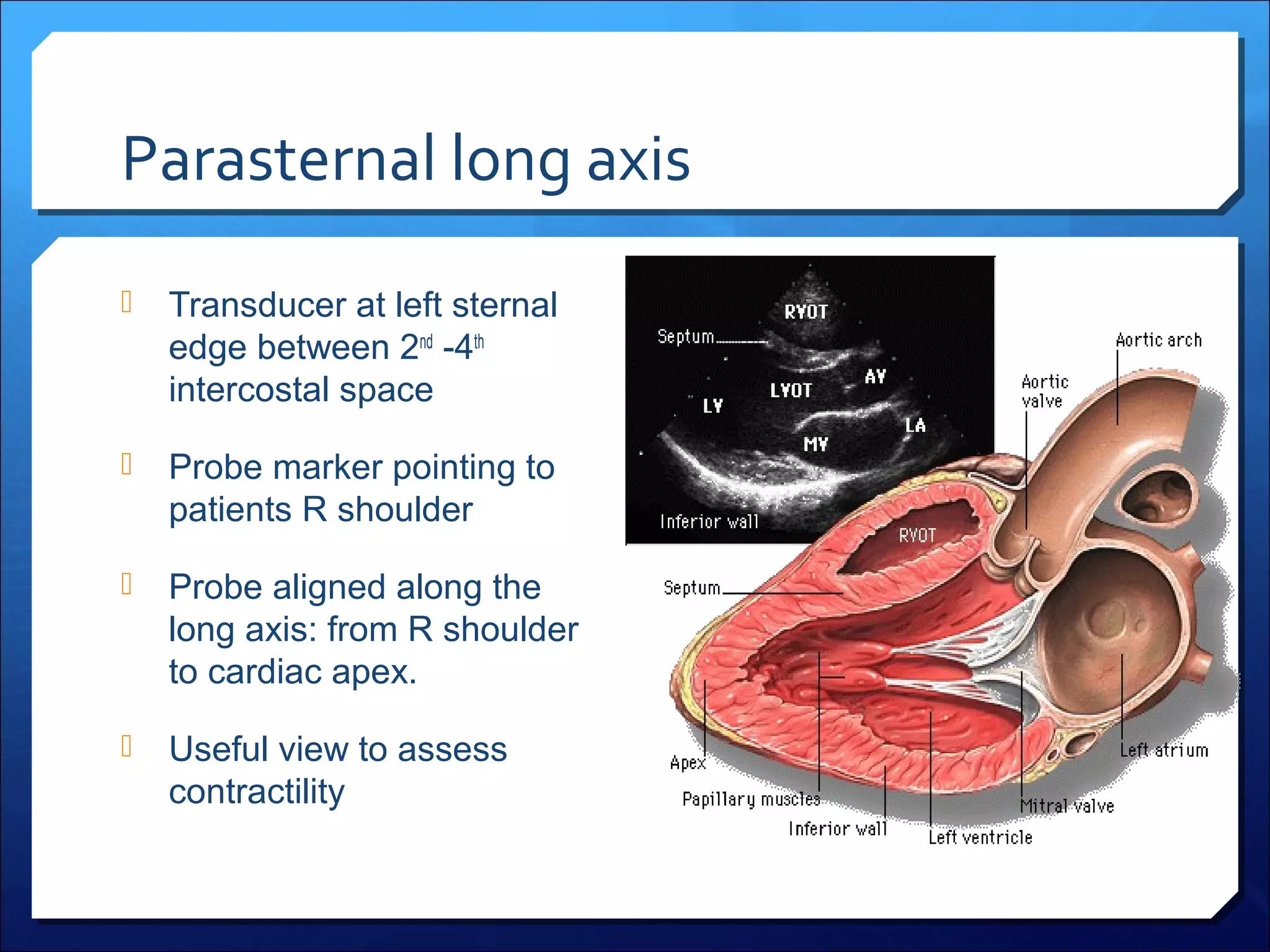
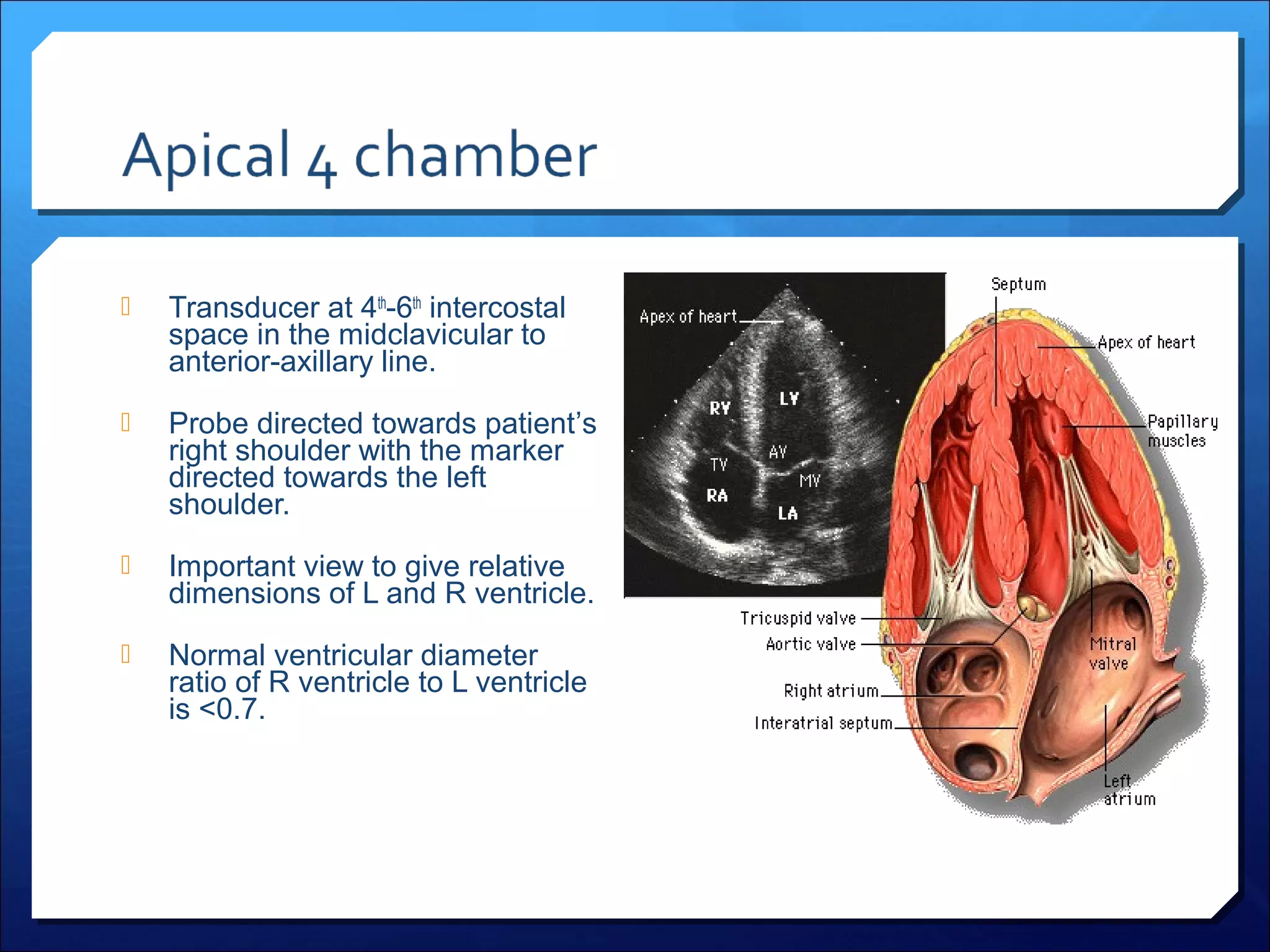
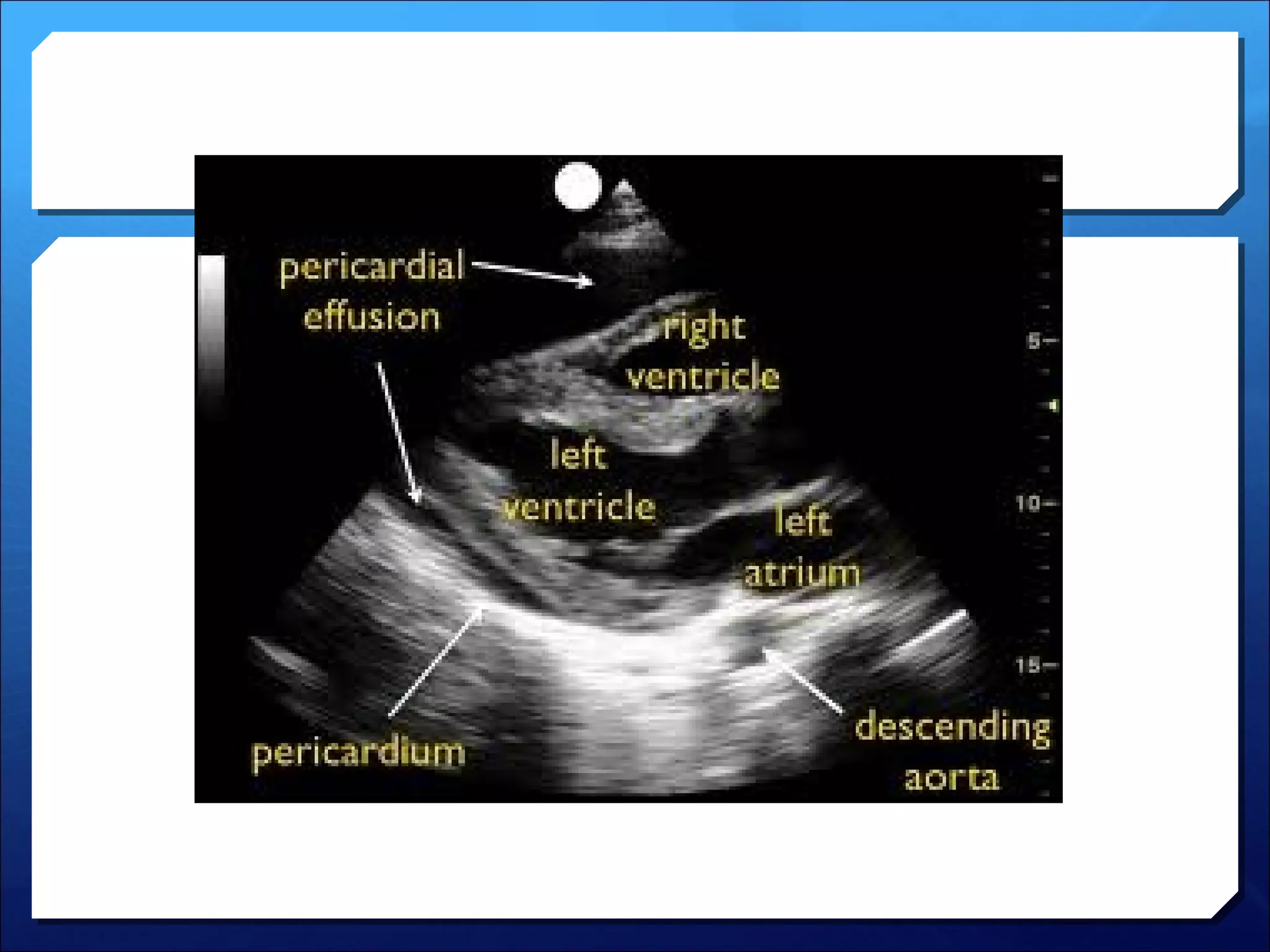
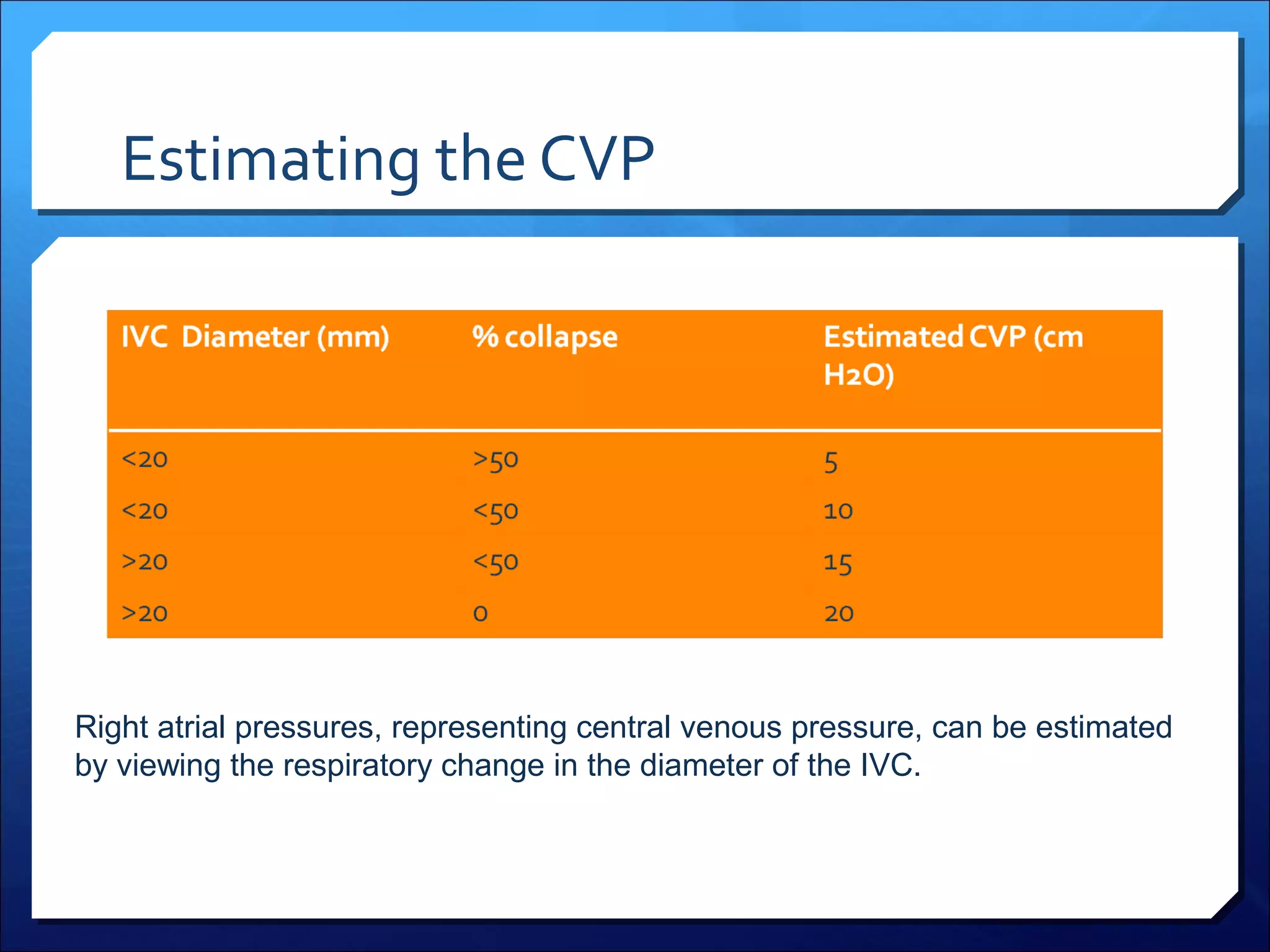
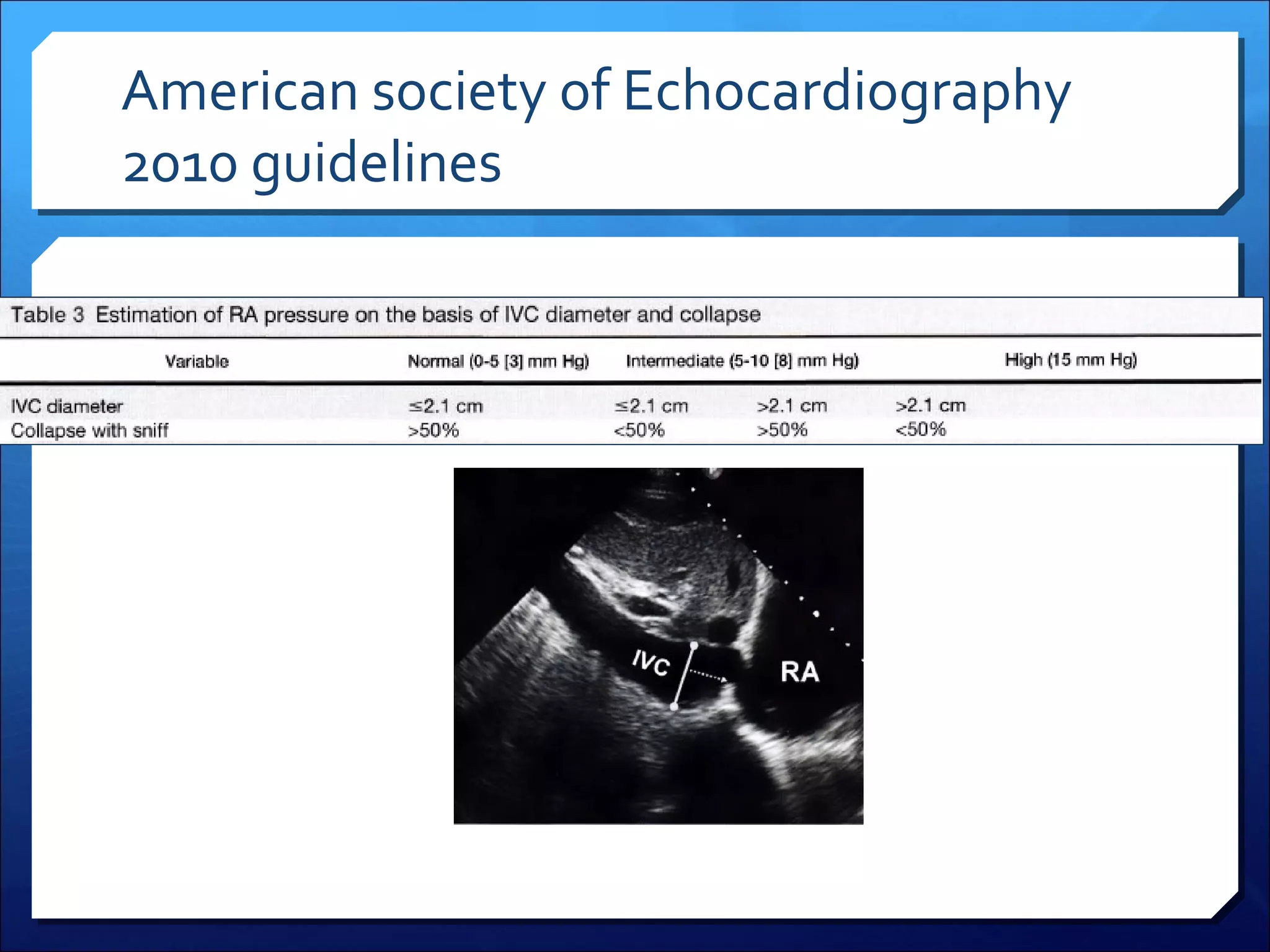
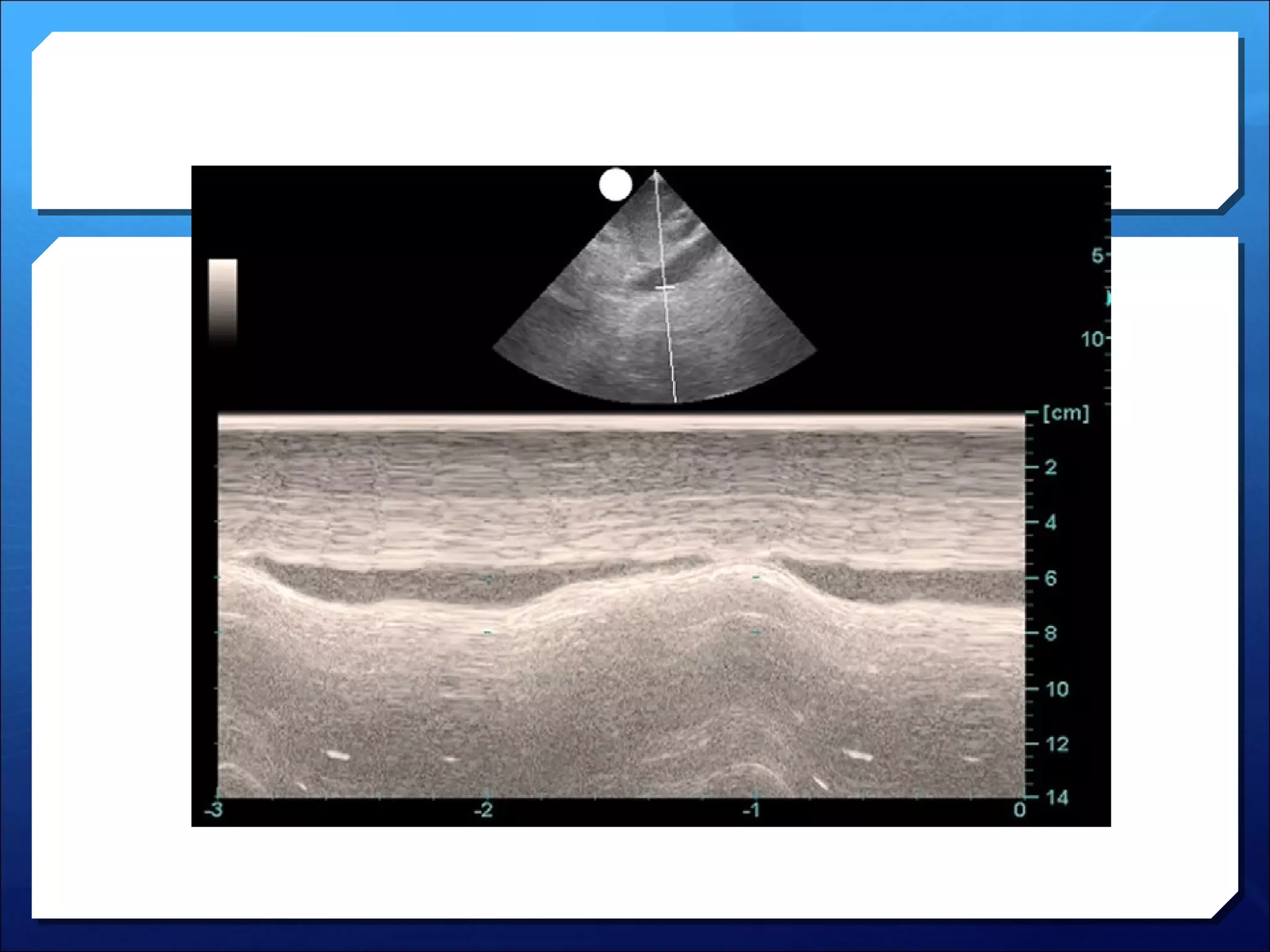
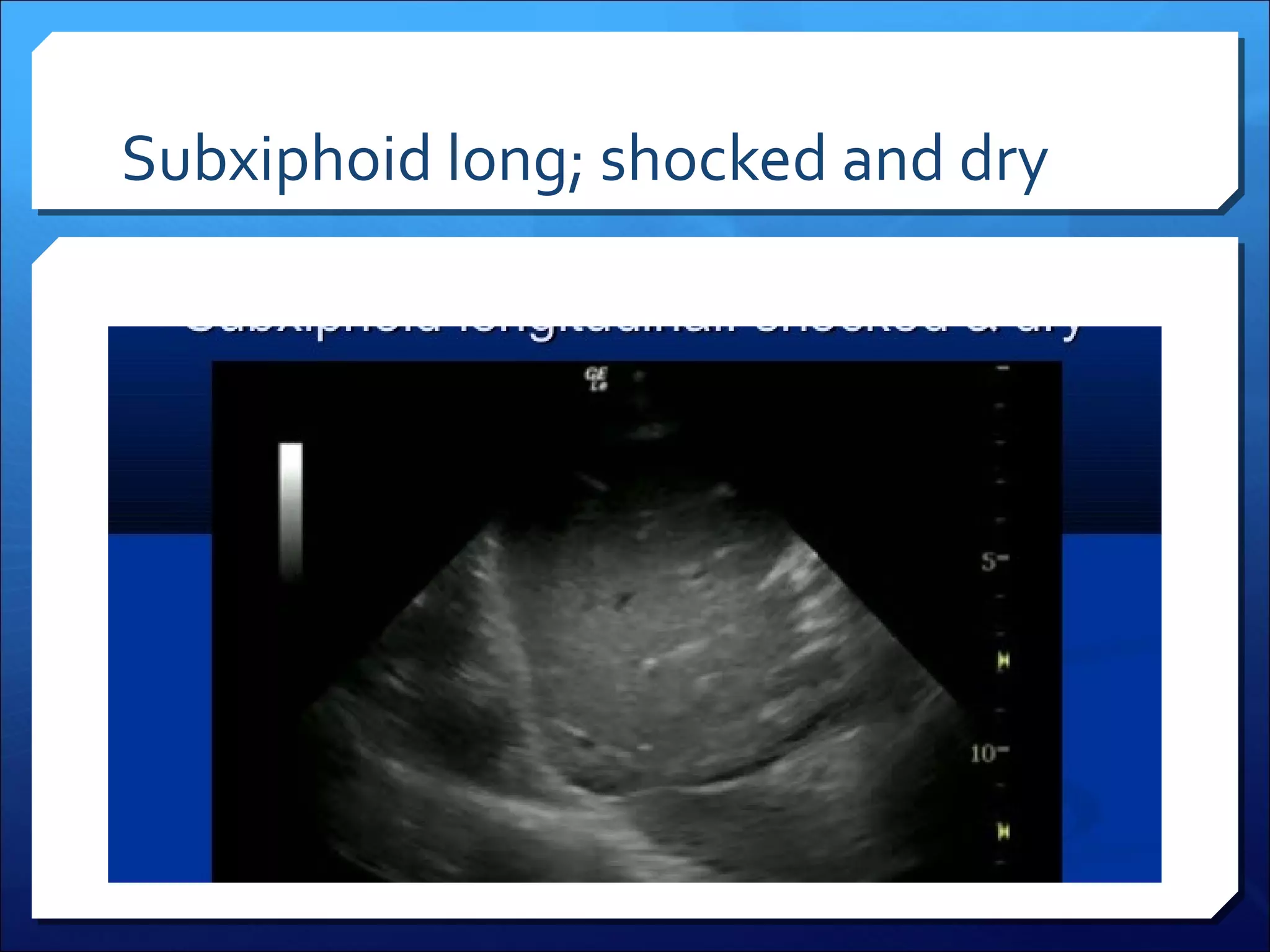
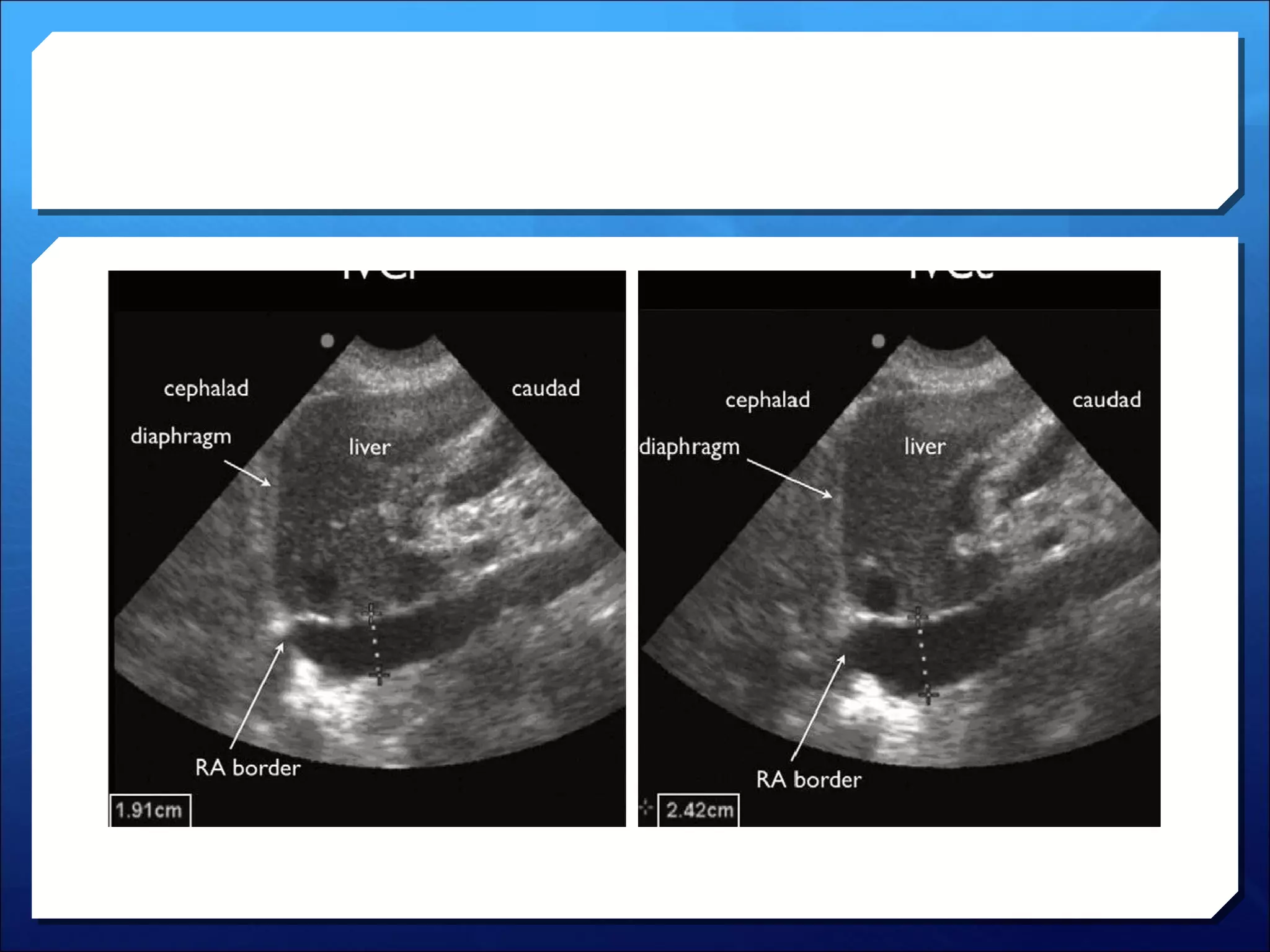
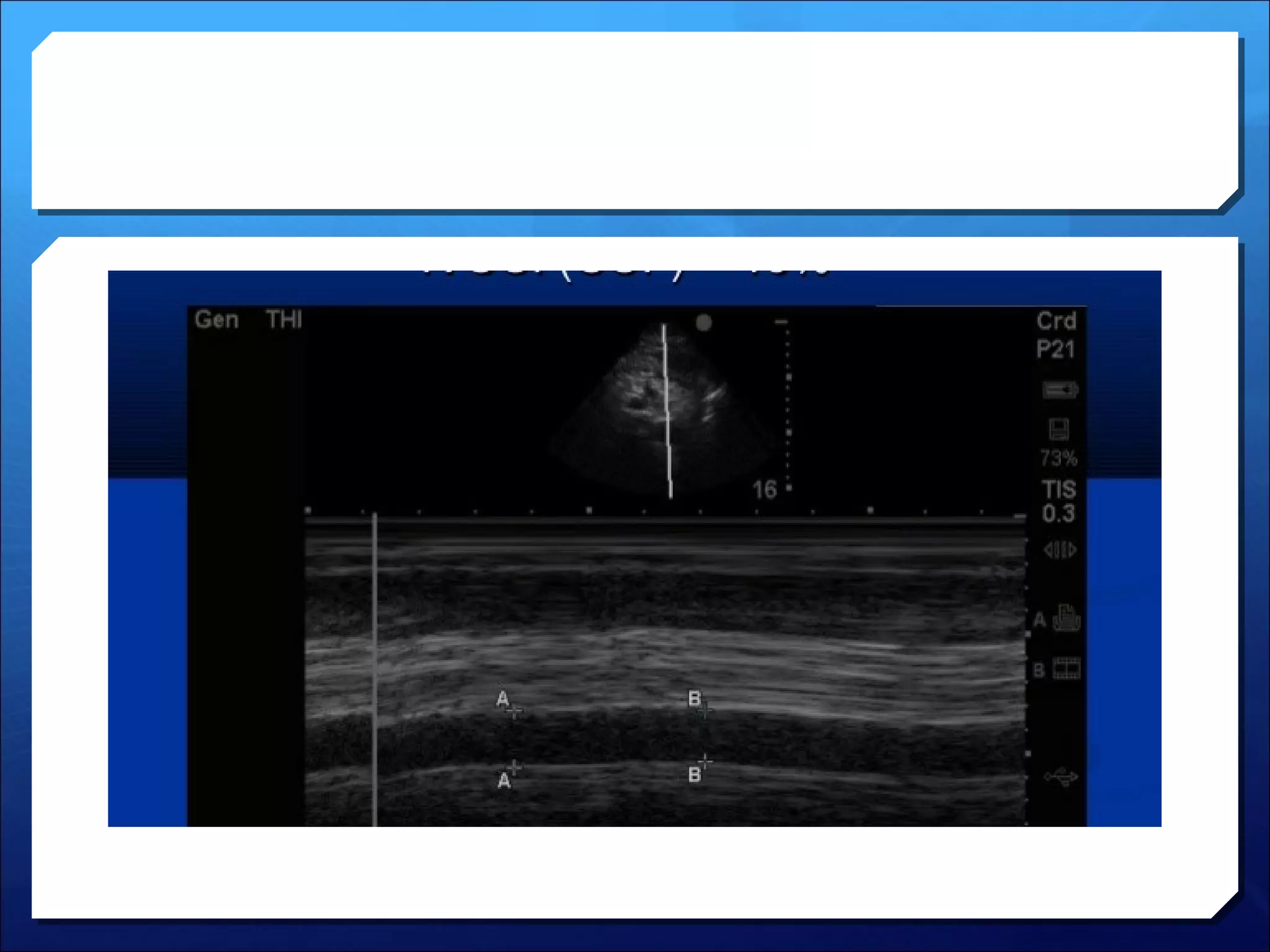
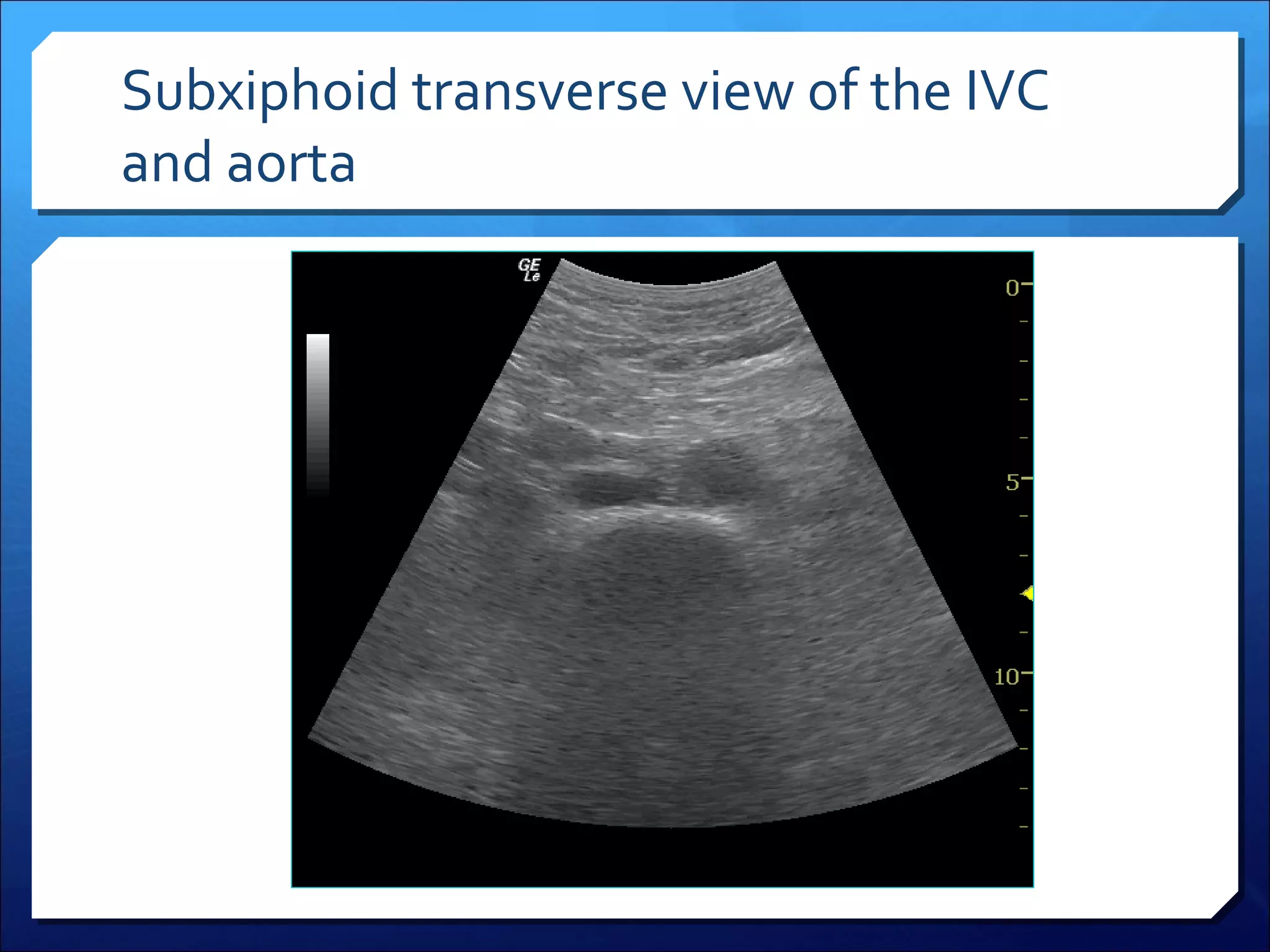
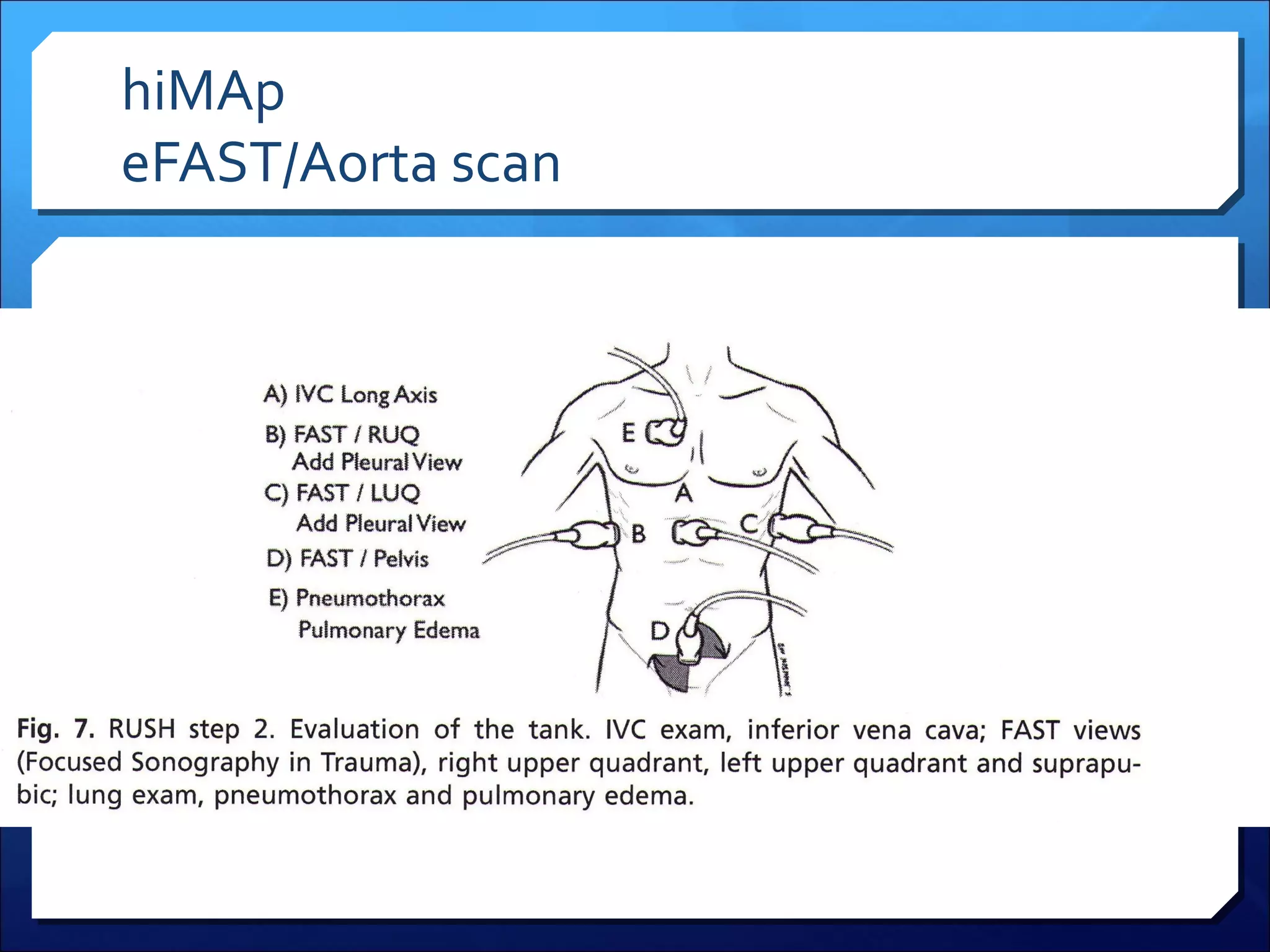
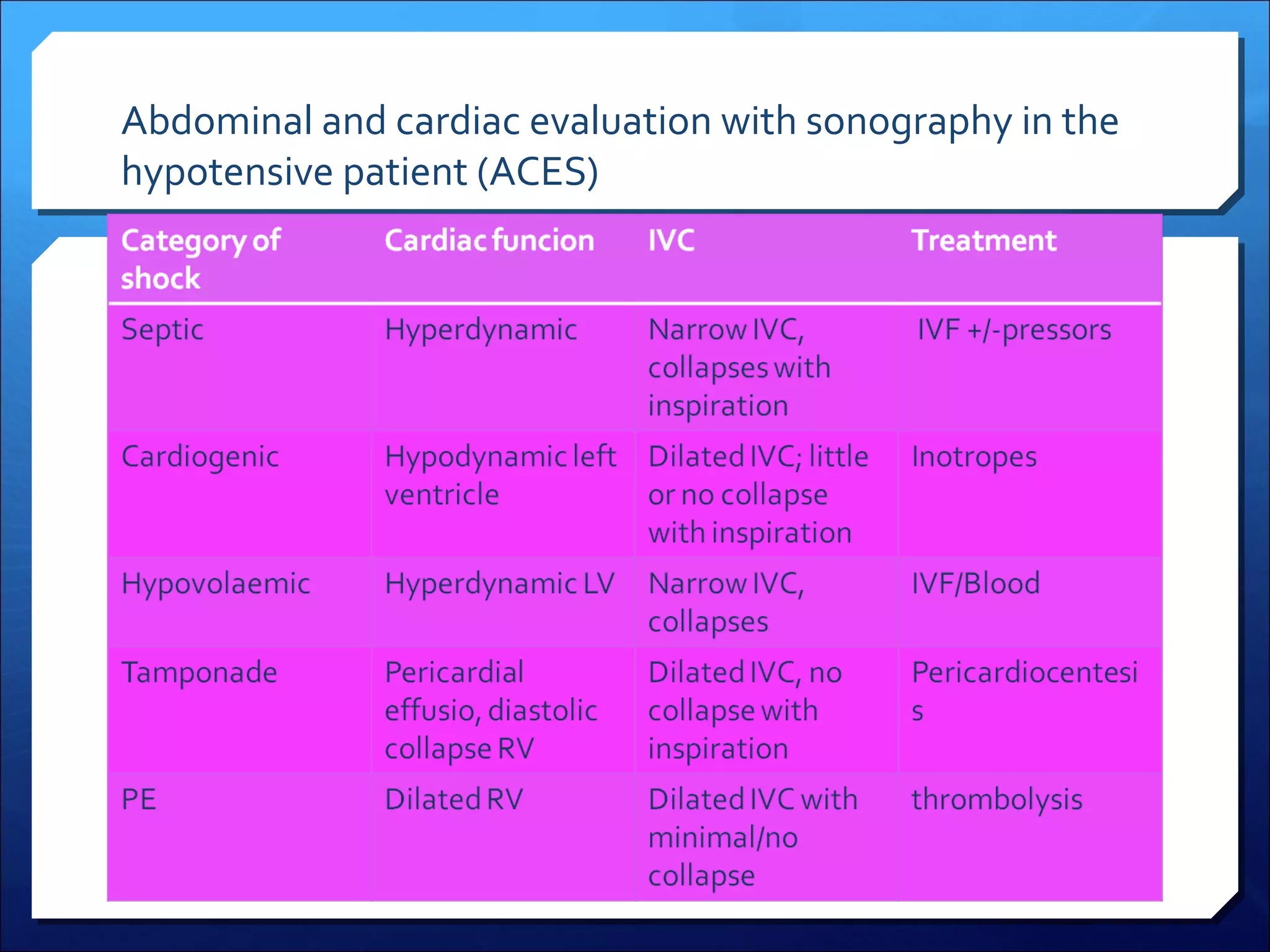
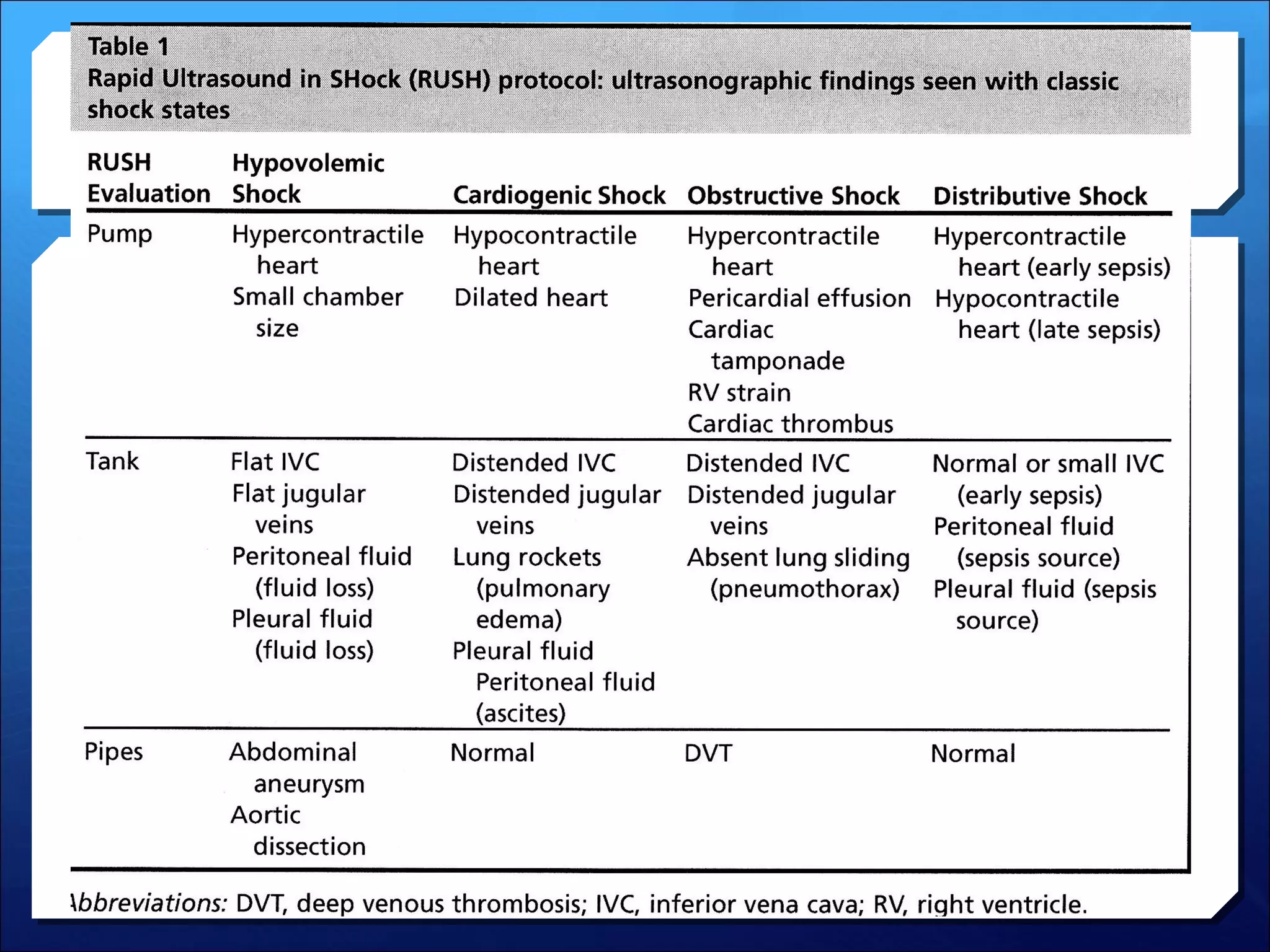
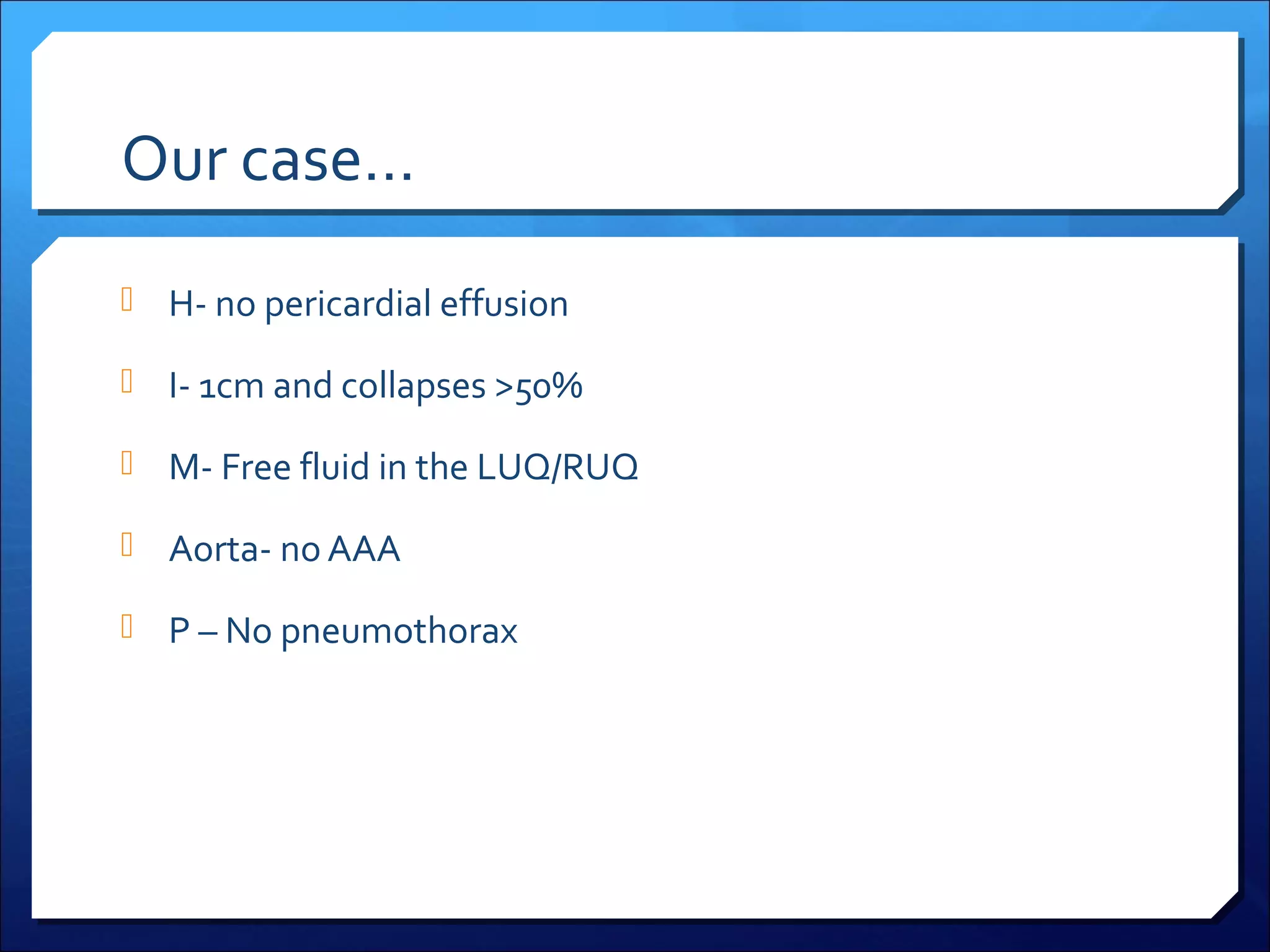
Ultrasound can be useful in the evaluation and diagnosis of patients presenting in shock. Integrating bedside ultrasound allows for a more accurate initial diagnosis and earlier treatment. The RUSH protocol assesses the heart, IVC, pericardial space and lungs to help classify the type of shock. Ultrasound findings of a dilated and collapsing IVC along with evidence of free fluid suggest the patient has hypovolemic shock likely due to internal bleeding.