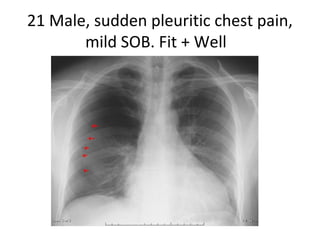
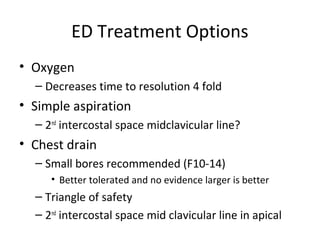
This document discusses the management of pneumothorax. Key factors in treatment include whether the pneumothorax is spontaneous or traumatic, primary or secondary, the patient's age and symptoms, and the size of the pneumothorax. Small pneumothoraces may be treated with oxygen or simple aspiration while larger ones often require a chest drain. Follow up is important to ensure complete resolution. Recurrent or bilateral pneumothoraces may require early specialist involvement. Treatment options range from observation to procedures like thoracotomy or pleurodesis.