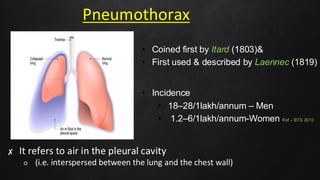
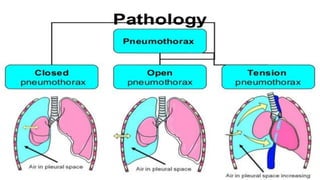
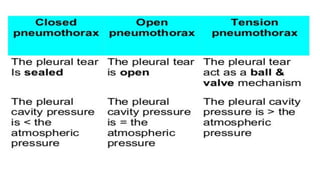
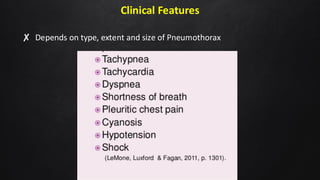
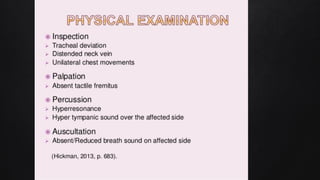
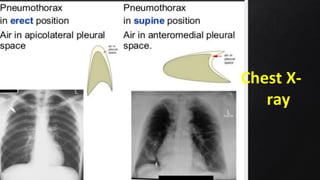
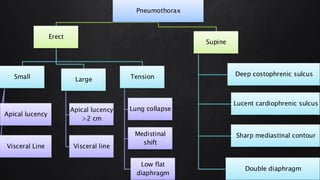
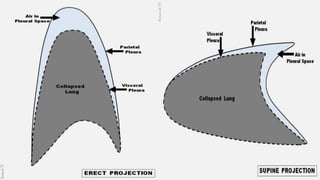
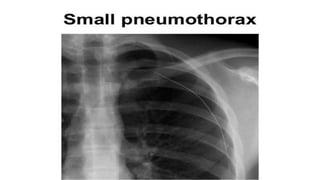
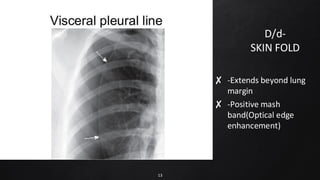
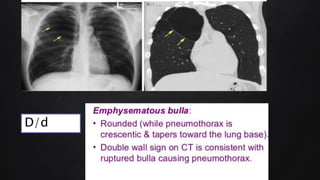
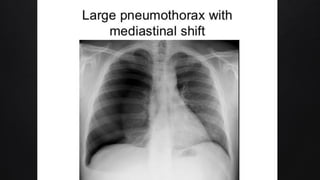
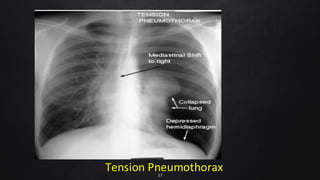
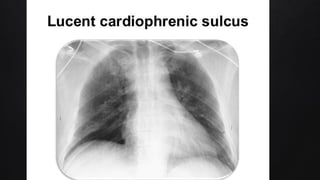
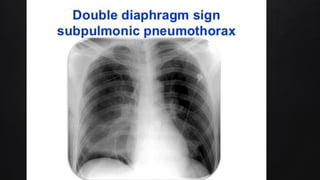
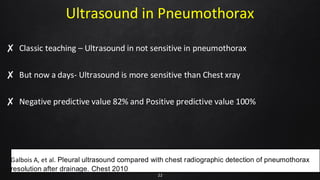
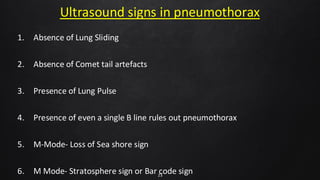
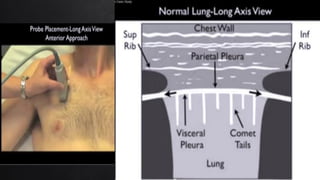
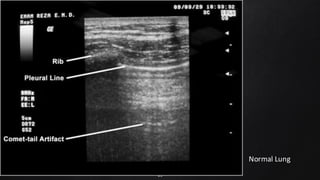
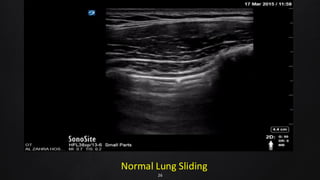
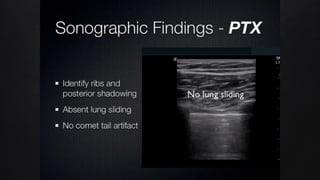
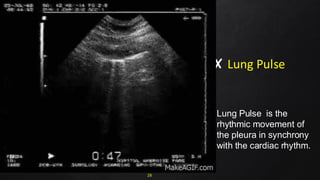
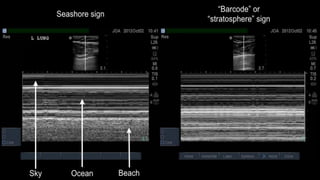
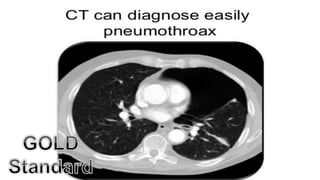
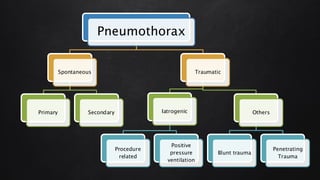
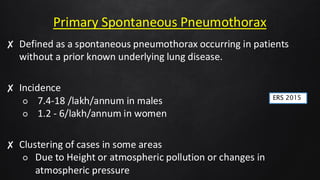
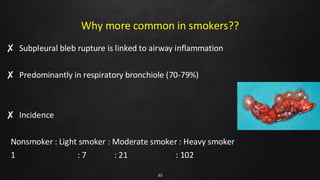
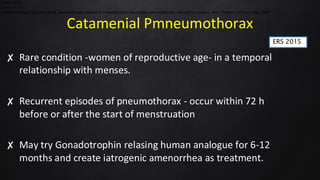
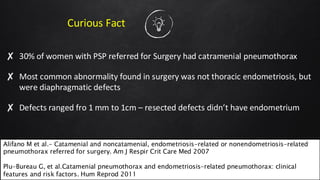
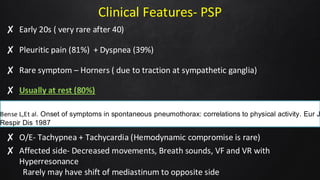
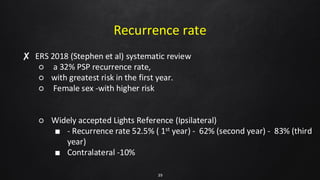
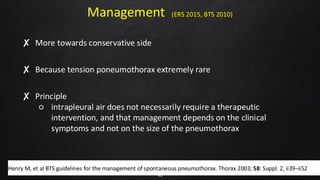
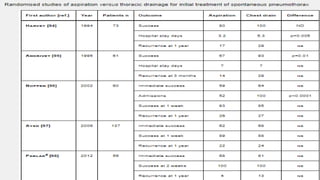
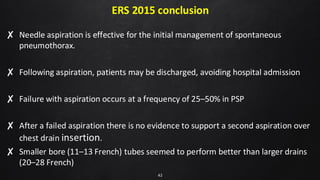
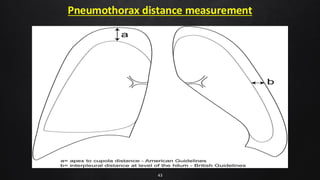
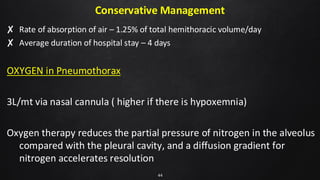
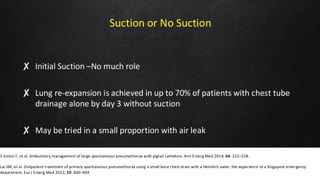
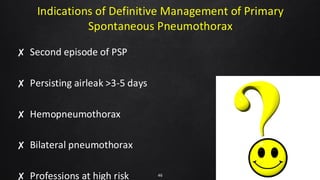
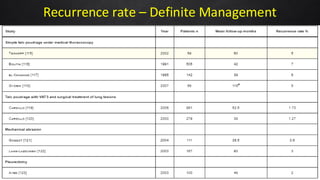
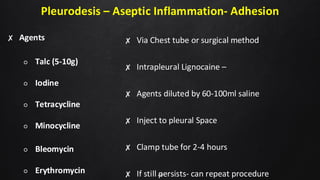
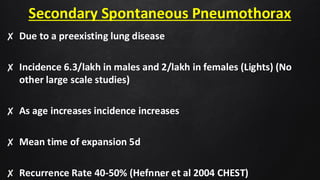
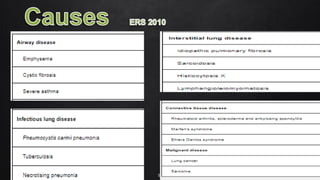
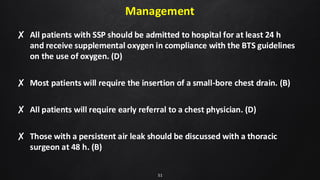
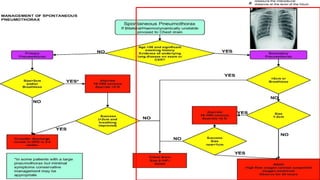
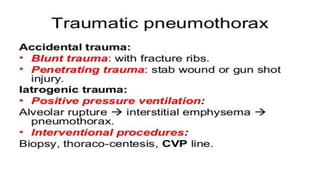
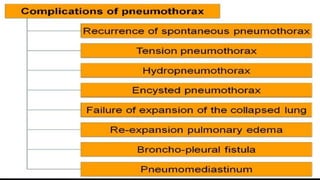
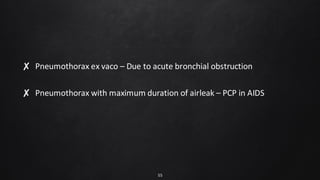
The document discusses pneumothorax, an accumulation of air in the pleural cavity, detailing its types, clinical features, incidence rates, and diagnostic methods such as chest X-ray and ultrasound. It highlights the management strategies, advocating for conservative treatment and describing interventions like needle aspiration and chest tube insertion. Key points include the recurrence rates for spontaneous pneumothorax and the characteristics of primary versus secondary spontaneous pneumothorax.