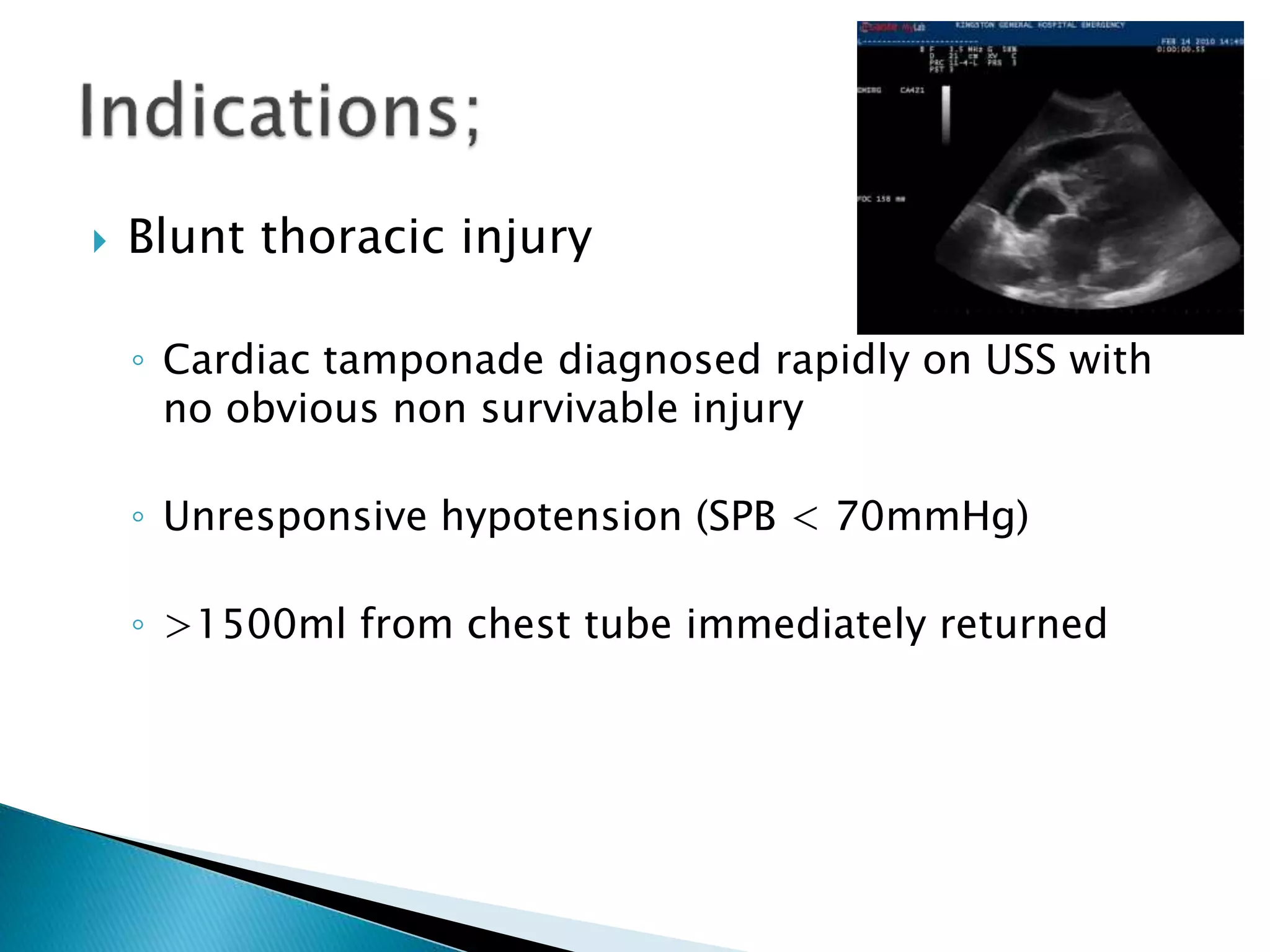
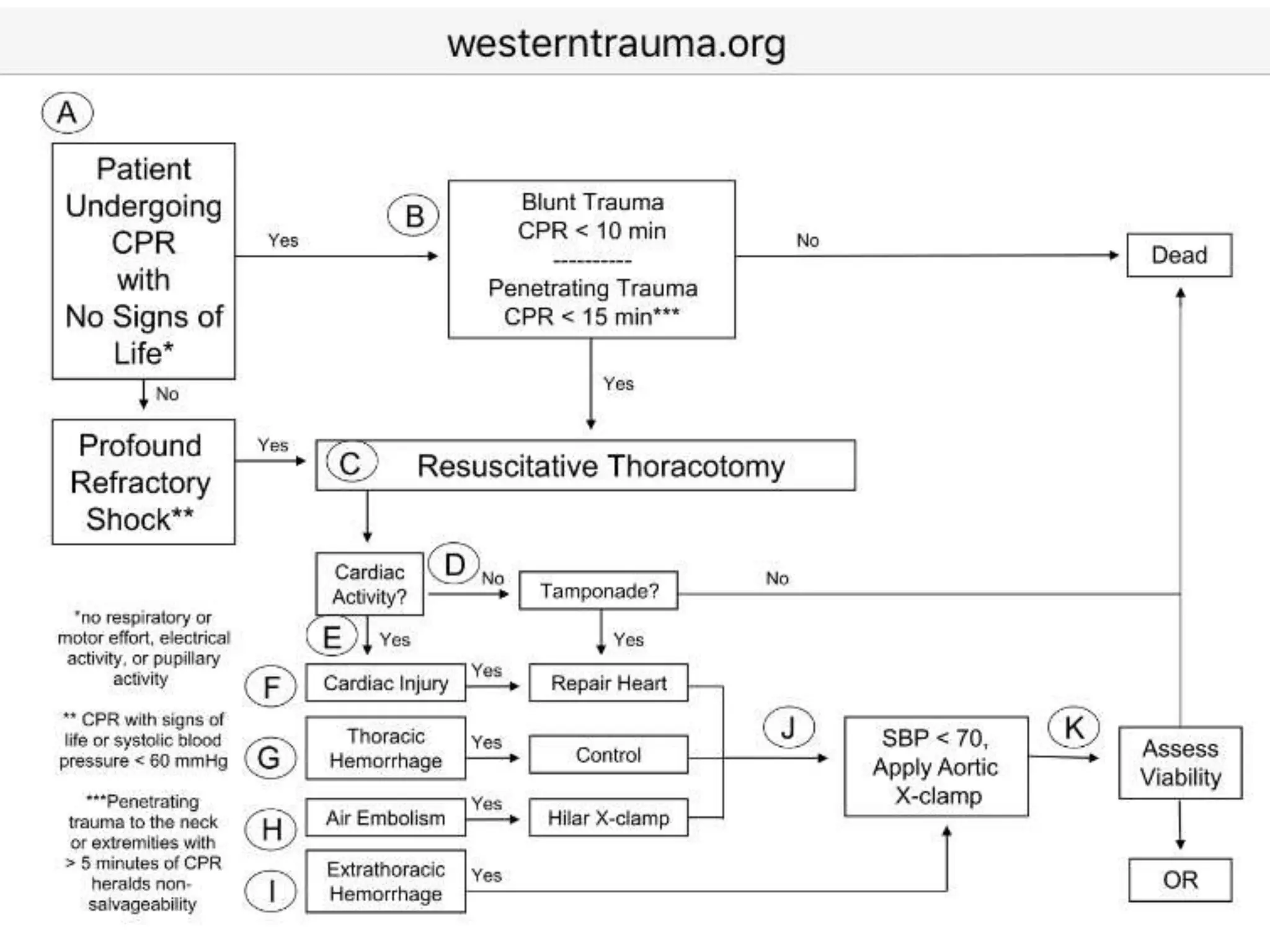
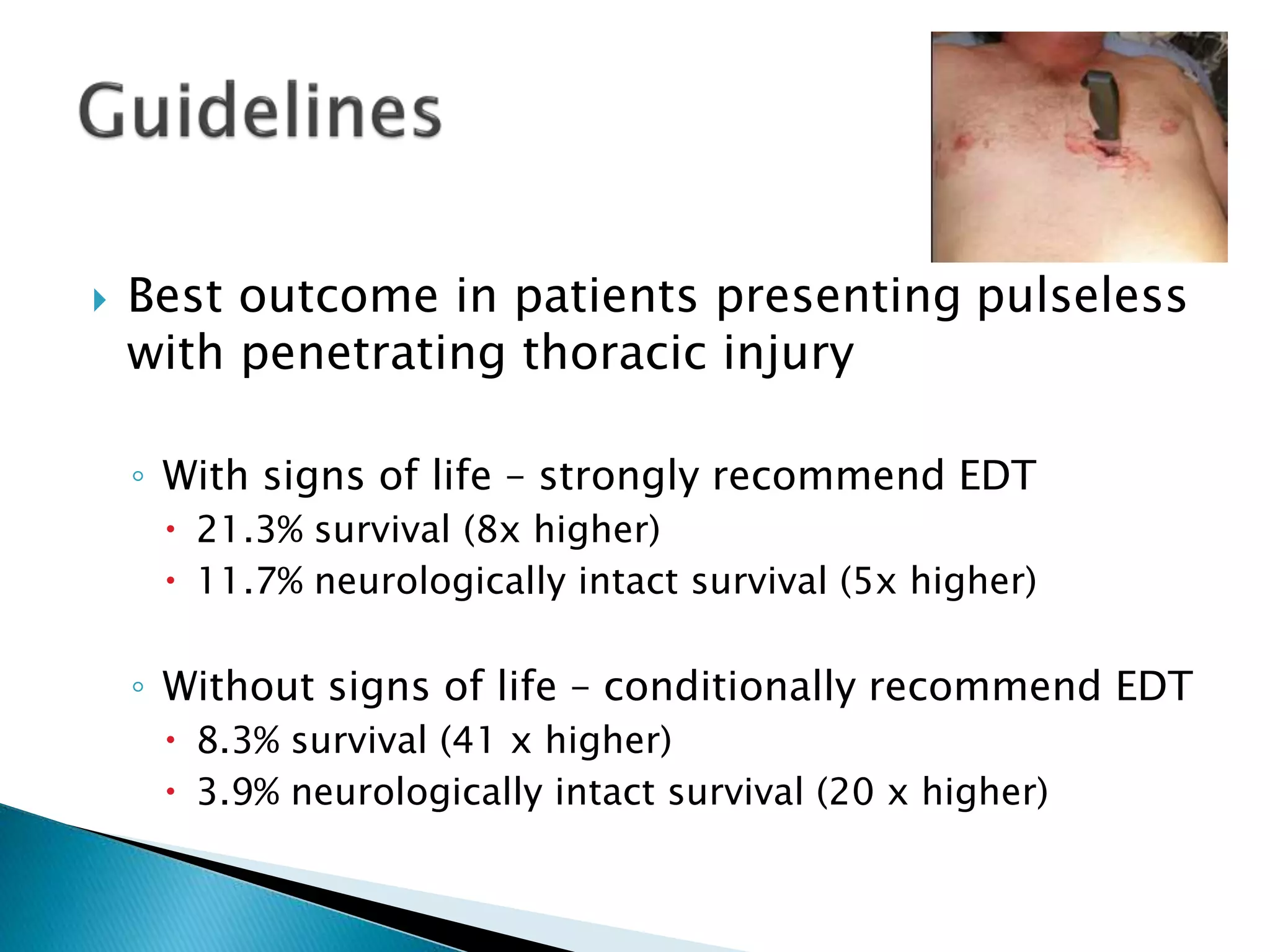
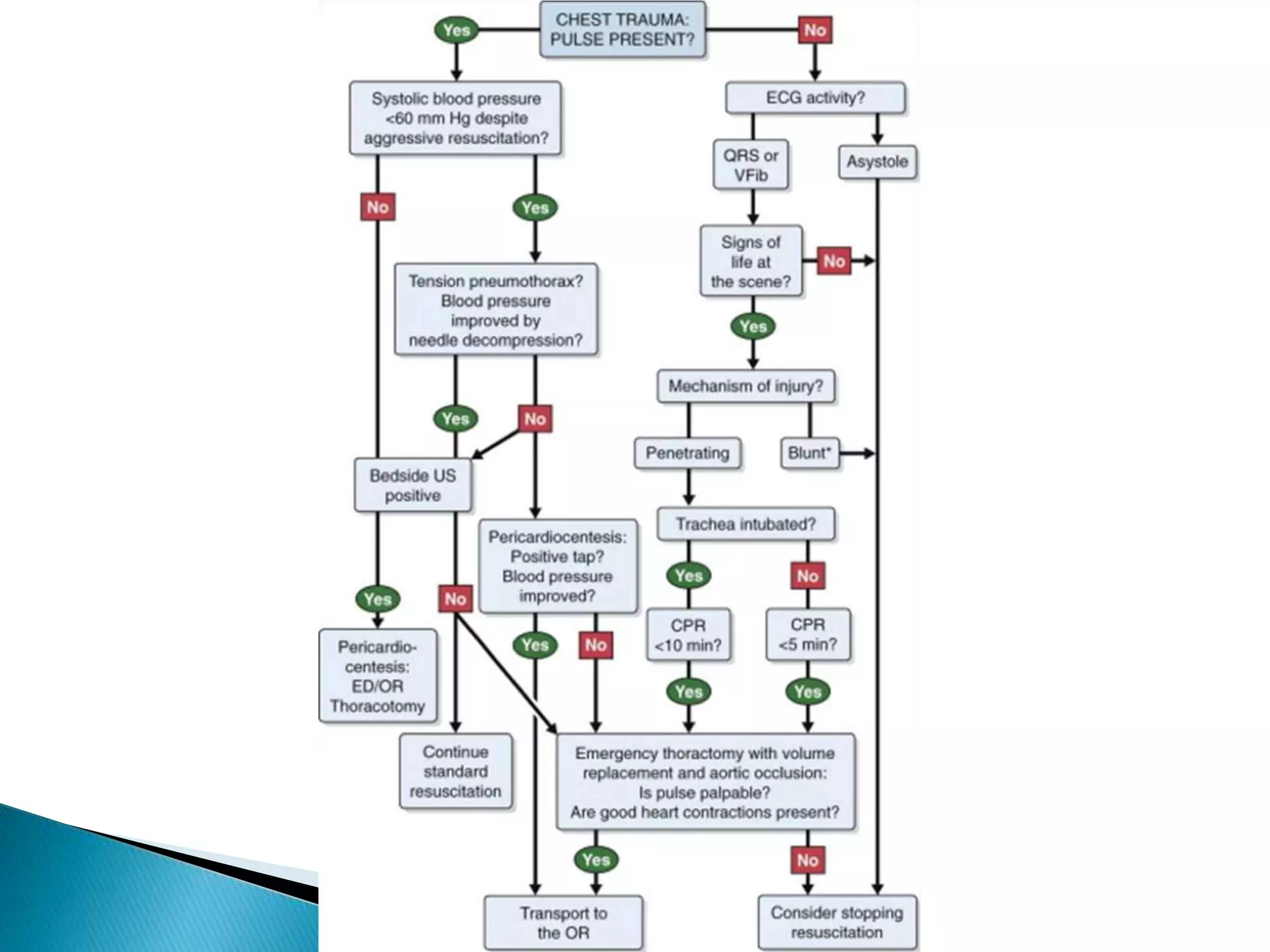
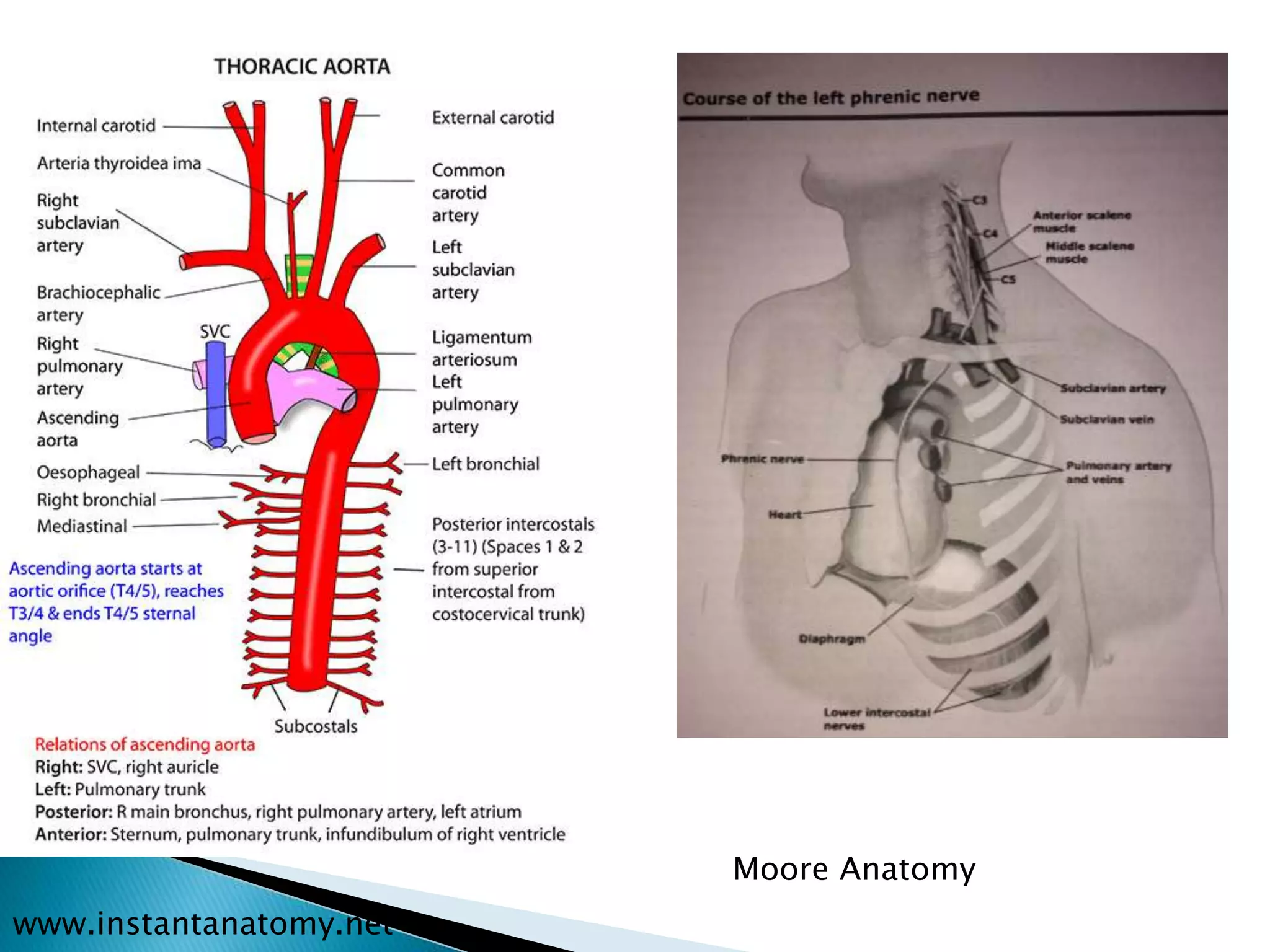
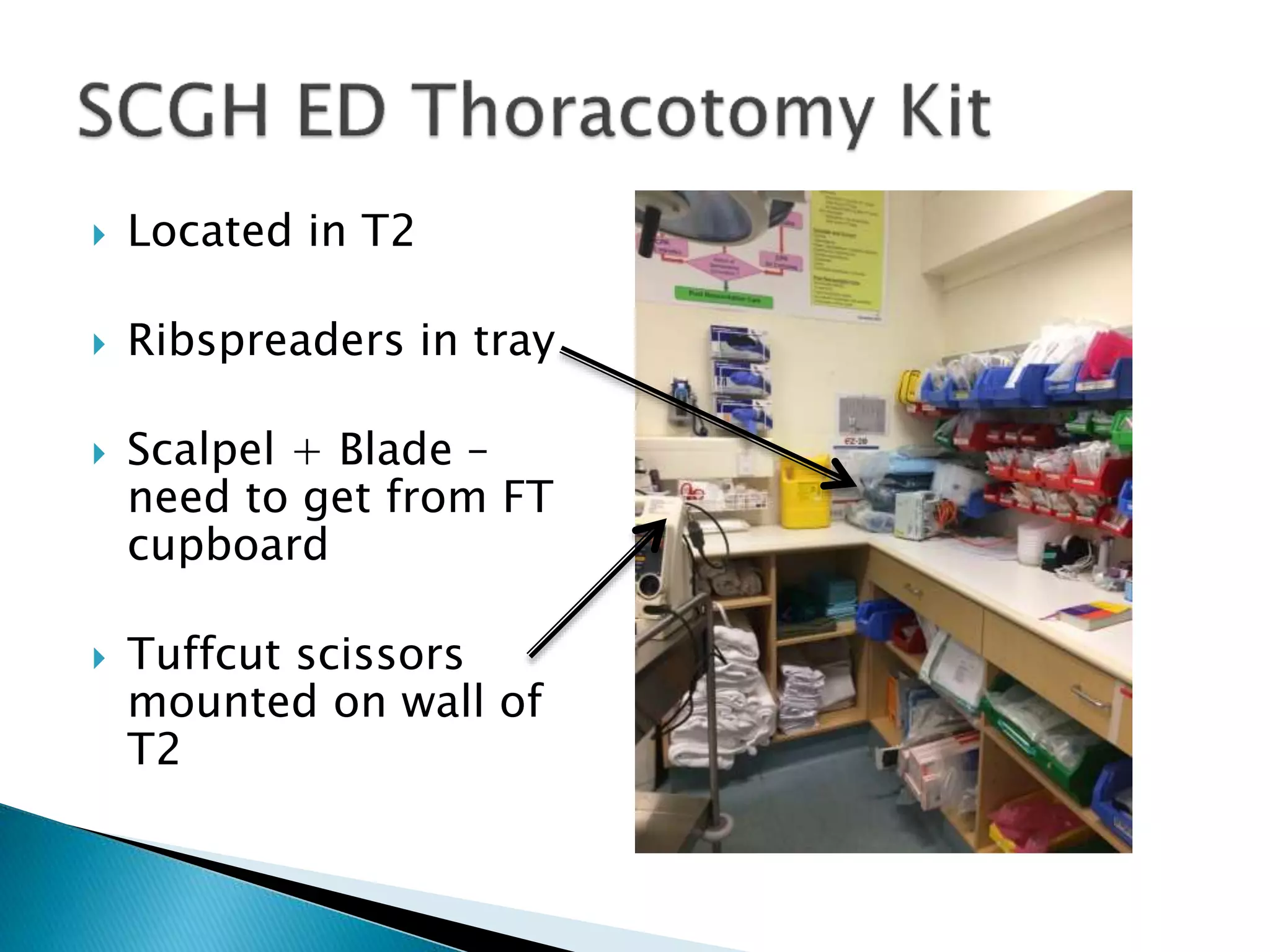
This document discusses emergency thoracotomy for traumatic injuries. It outlines indications for the procedure including hemodynamic instability from penetrating chest injuries or cardiac tamponade. Steps of the procedure are described including a clamshell incision and interventions like controlling hemorrhage, cardiac massage, and aortic clamping. Contraindications include prolonged downtime or signs of unsurvivable injuries. Studies show improved survival in penetrating injuries with signs of life when thoracotomy is performed in the ED. Proper training and equipment are needed to perform this critical lifesaving procedure.