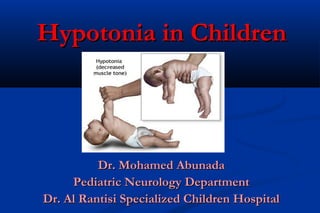
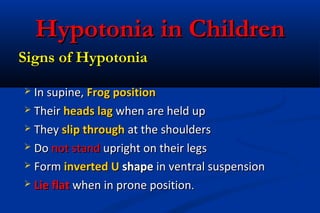
Hypotonia, or low muscle tone, is common in children and can be caused by neurological conditions that affect the brain, spinal cord, nerves, or muscles. Signs of hypotonia include poor head control, slipping through caregiver's hands when held, and lying in an inverted "U" shape when placed prone or held upright. The diagnosis involves assessing prenatal risk factors, family history, signs and symptoms, and ruling out disorders of the brain, spinal cord, peripheral nerves, muscles or neuromuscular junction through examination of reflexes and extra features present. Hypotonia can be caused by various conditions like cerebral palsy, brain malformations, genetic disorders or hypoxic ischemic encephalopathy.



![Signs of HypotoniaSigns of Hypotonia
Poor ability to cough and clear airway secretions.Poor ability to cough and clear airway secretions.
Poor swallowing abilityPoor swallowing ability
Crying character [weak, low pitched]Crying character [weak, low pitched]
Paradoxical breathing pattern. Intercostal musclesParadoxical breathing pattern. Intercostal muscles
paralyzed with intact diaphragm.paralyzed with intact diaphragm.](https://image.slidesharecdn.com/hypotoniainchildren-151012185436-lva1-app6891/85/Hypotonia-in-children-6-320.jpg)























































![ManagementManagement
Supportive [respiratory, gastrointestinal]Supportive [respiratory, gastrointestinal]
Once the correct diagnosis is confirmed, specificOnce the correct diagnosis is confirmed, specific
treatments should be offered if availabletreatments should be offered if available
Physiotherapy:Physiotherapy:
mainly preventative to avoid contractures and wasting, but will notmainly preventative to avoid contractures and wasting, but will not
increase muscle toneincrease muscle tone
Genetics counseling.Genetics counseling.](https://image.slidesharecdn.com/hypotoniainchildren-151012185436-lva1-app6891/85/Hypotonia-in-children-64-320.jpg)







