1. Acute flaccid paralysis (AFP) is defined as sudden onset of weakness or paralysis over 15 days in patients under 15 years old. It suggests involvement of the lower motor neuron complex.
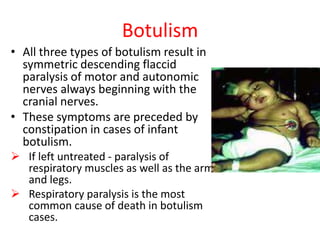
2. Common causes of AFP include poliomyelitis, Guillain-Barré syndrome, transverse myelitis, botulism, and non-polio enteroviruses. Clinical features and investigations can help differentiate between these causes.
3. Treatment depends on the underlying etiology but may include supportive care, IV immunoglobulin, plasmapheresis, and corticosteroids. Prognosis ranges from full recovery to residual deficits or death, depending on the cause and extent of