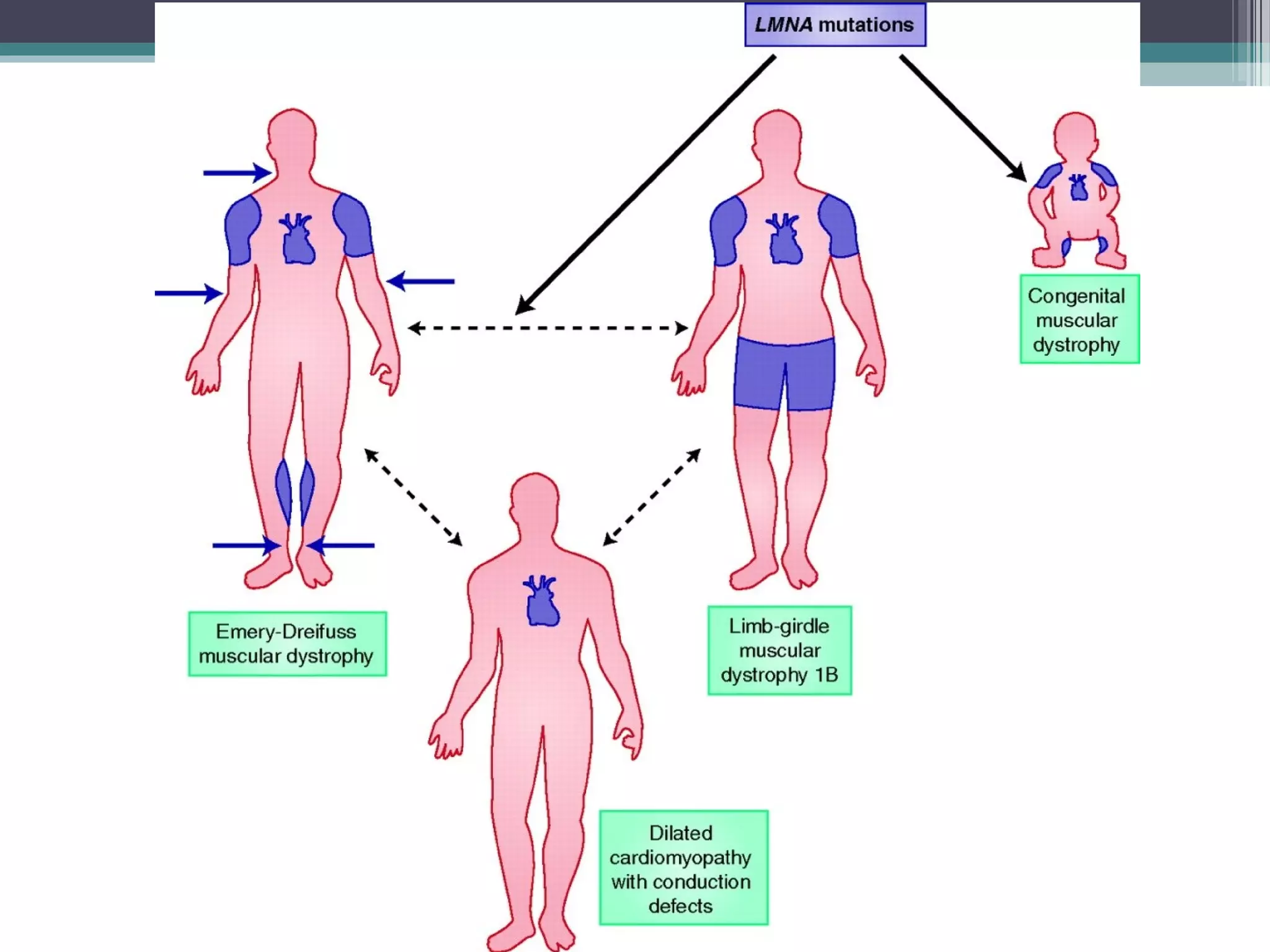
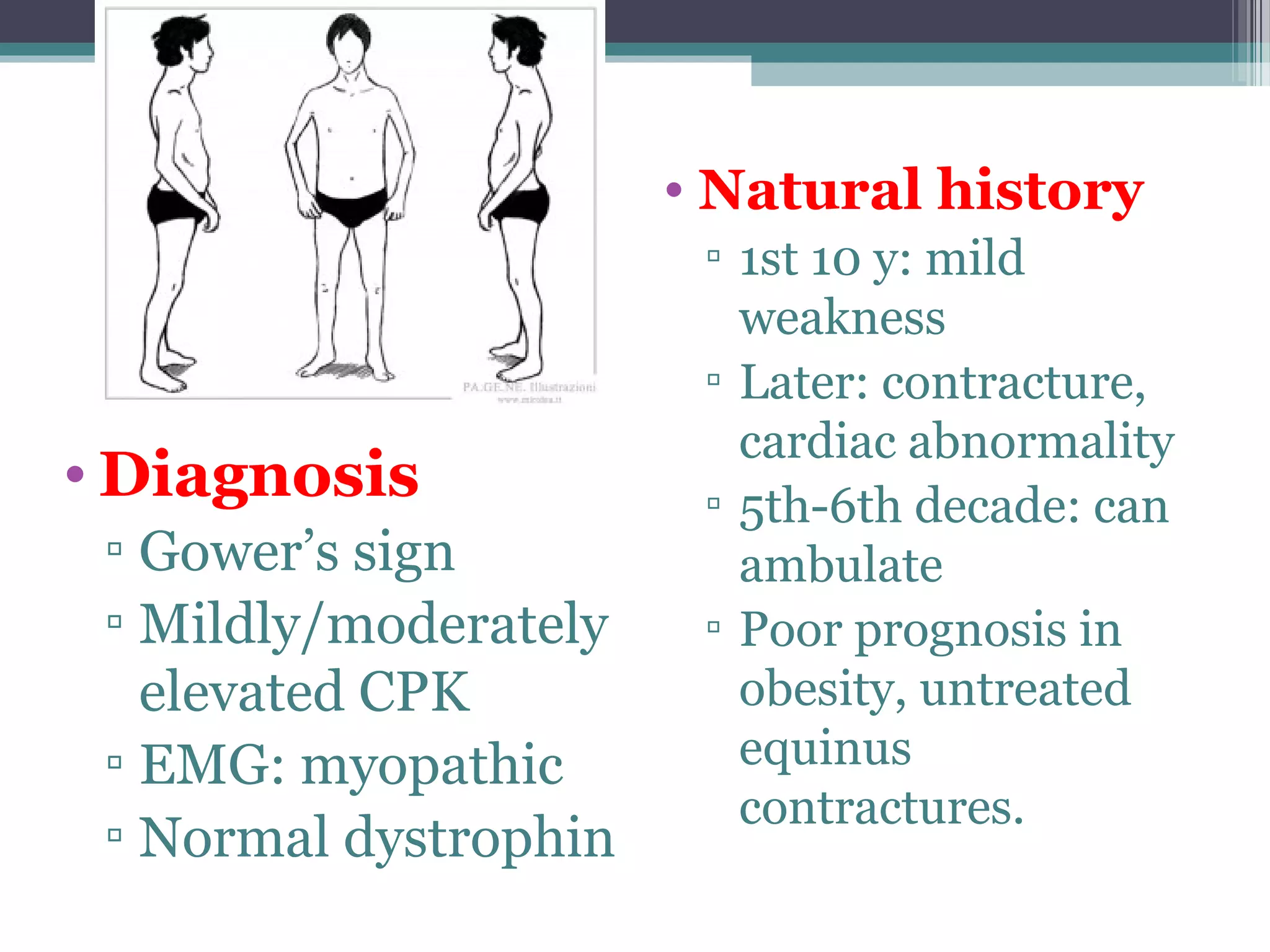
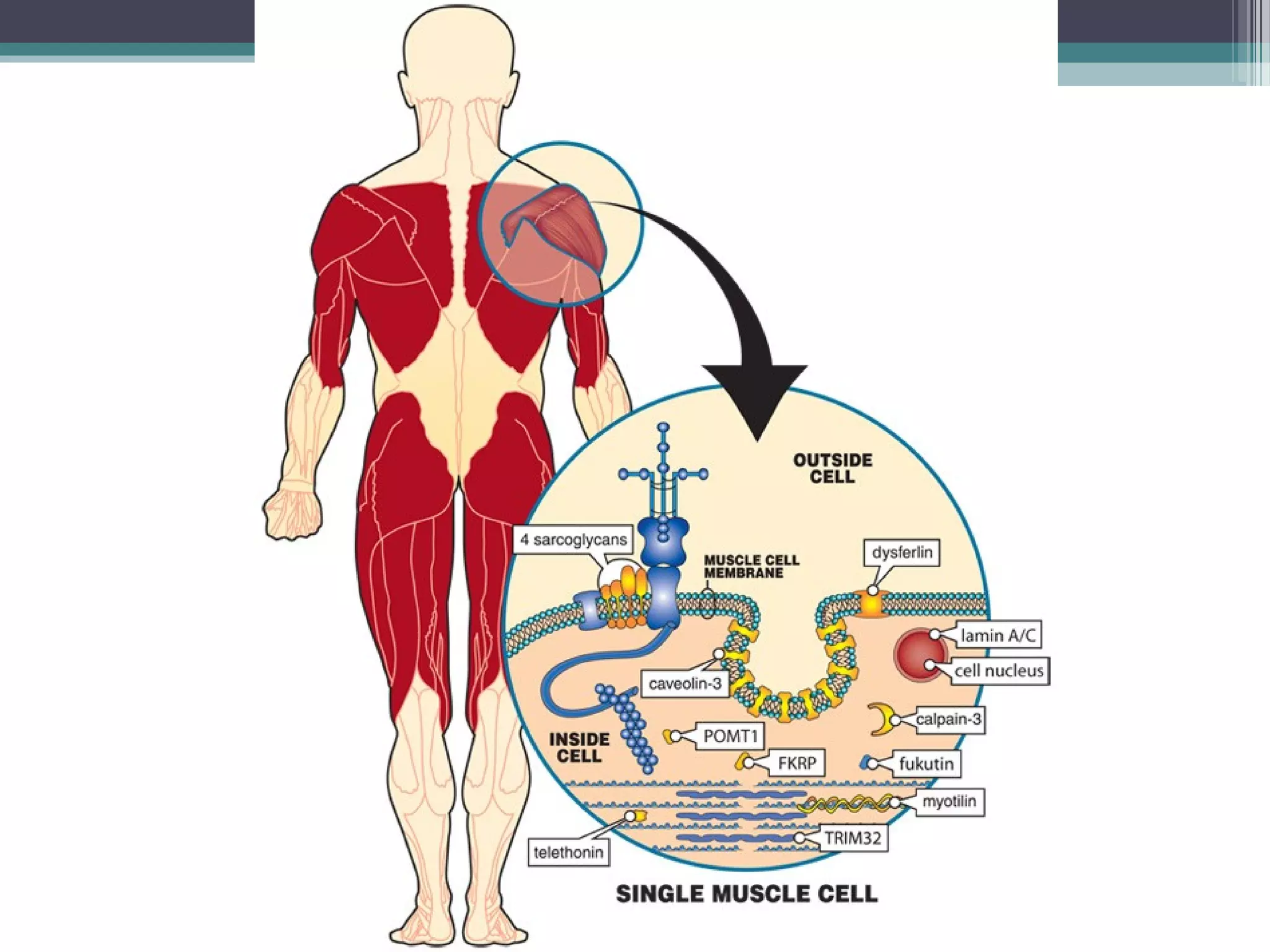
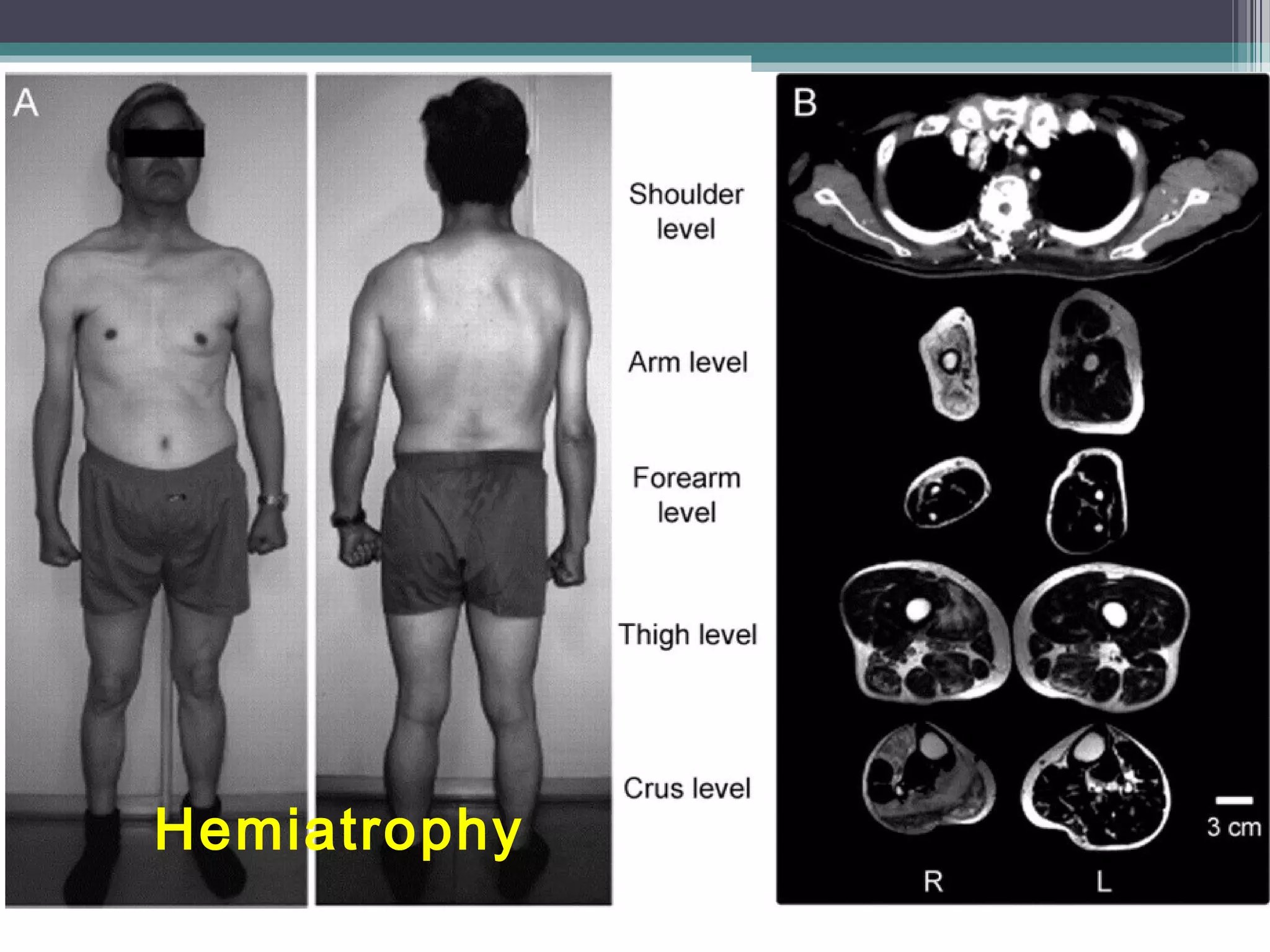
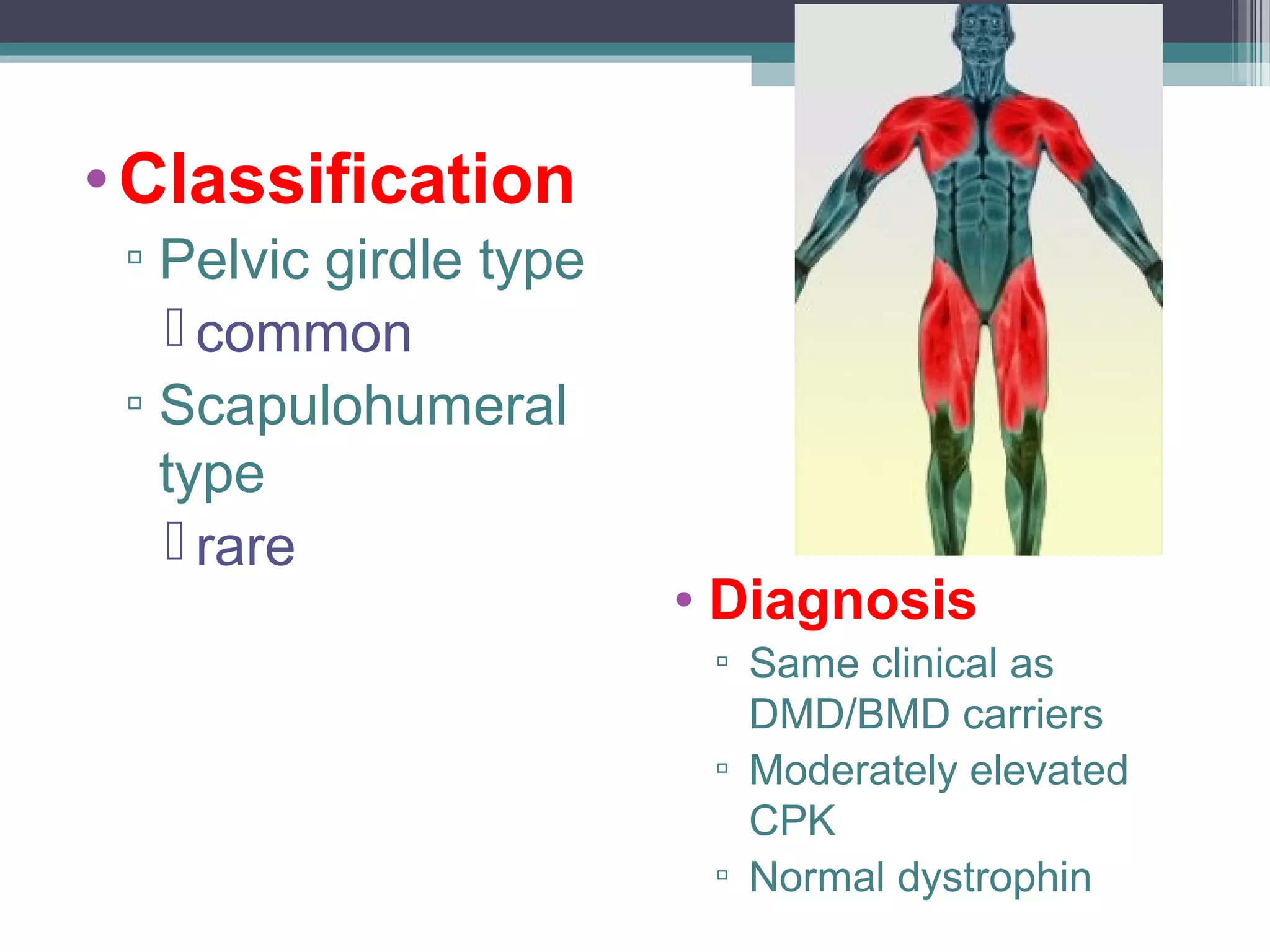
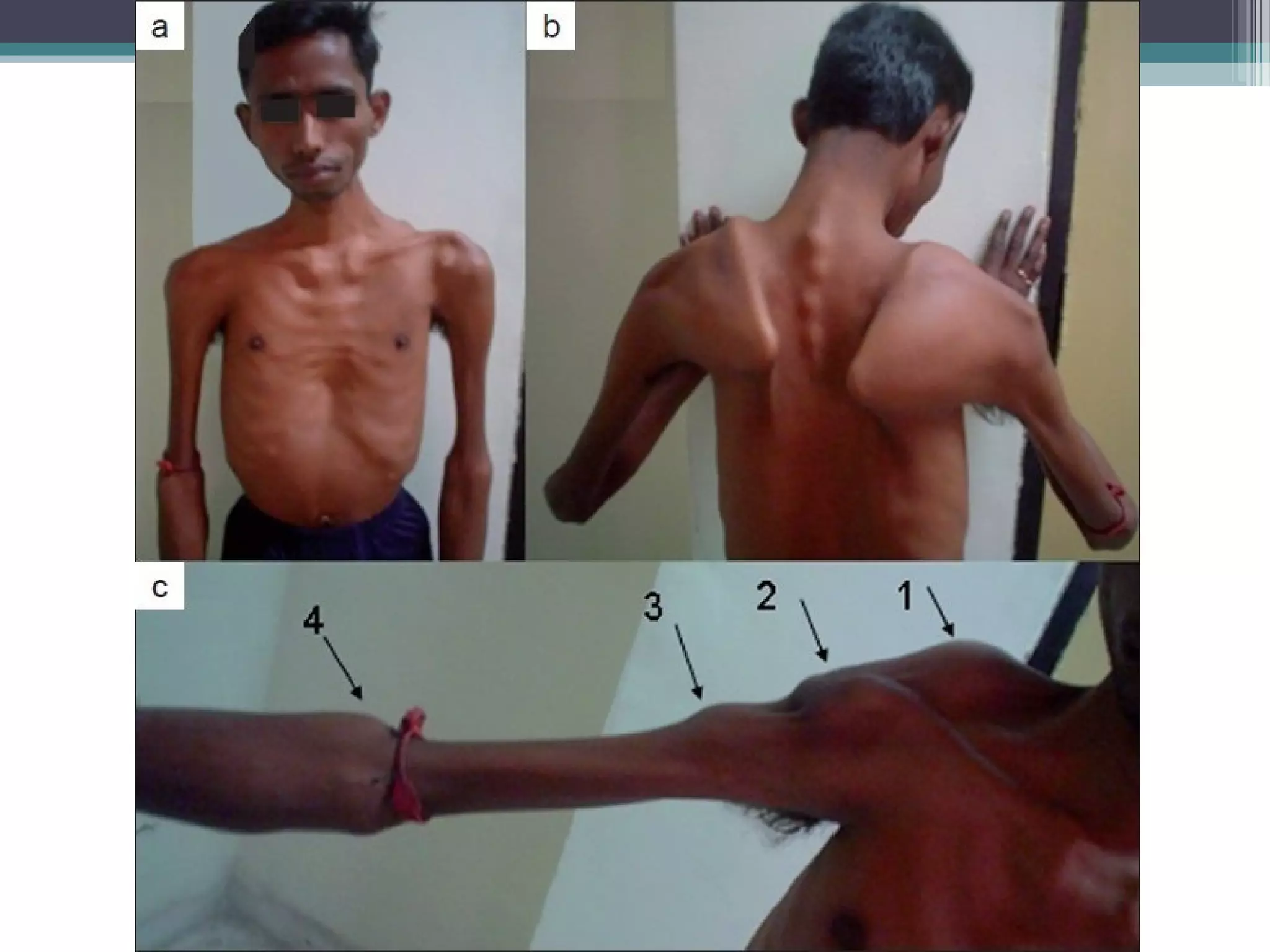
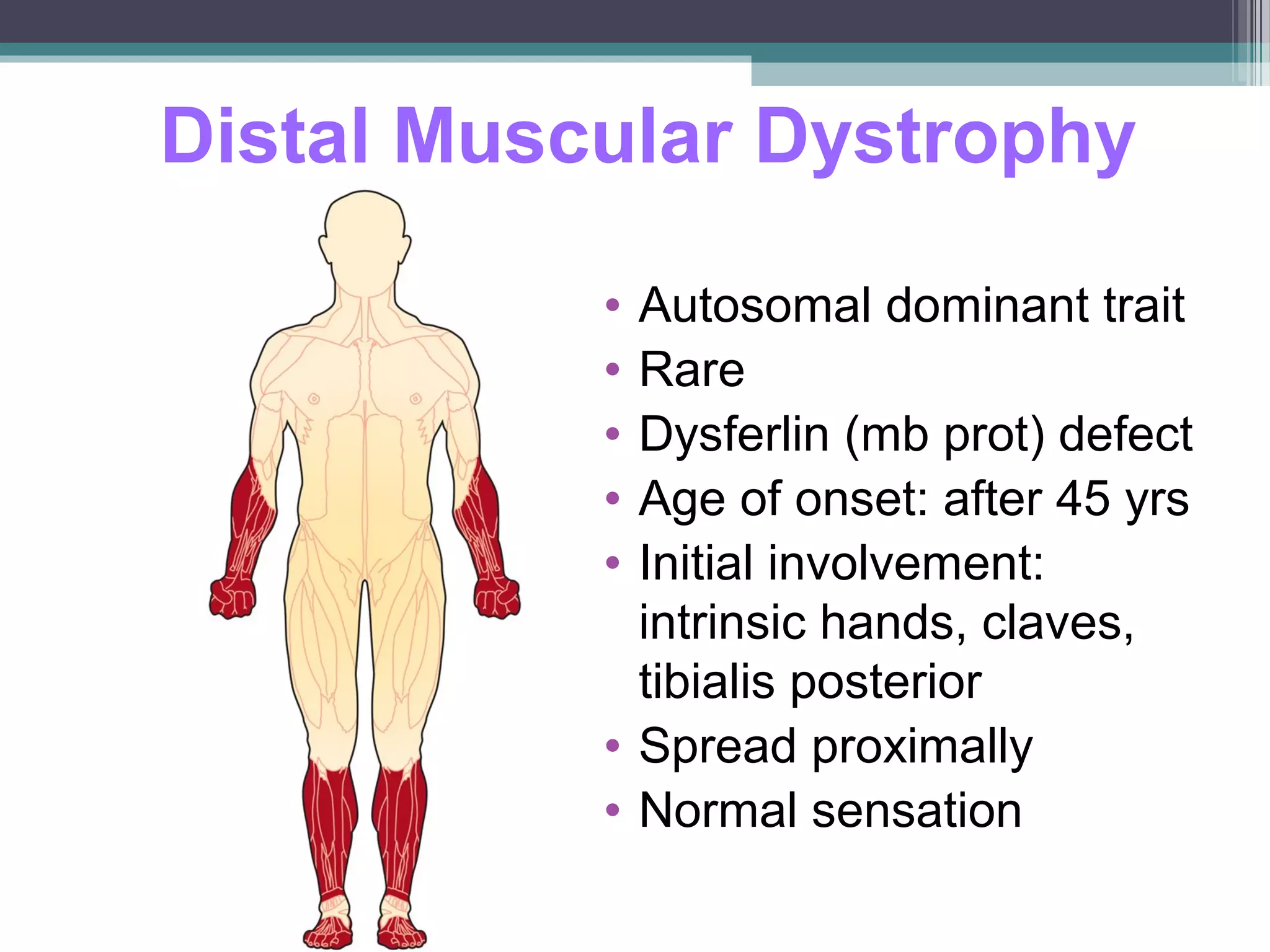
Muscular dystrophy is a heterogeneous group of inherited disorders characterized by progressive muscle weakness and loss of muscle tissue. The document discusses several types of muscular dystrophy including Duchenne muscular dystrophy (DMD), Becker muscular dystrophy, Emery-Dreifuss muscular dystrophy, limb-girdle muscular dystrophy, fascioscapulohumeral muscular dystrophy, distal muscular dystrophy, congenital muscular dystrophy, and myotonic muscular dystrophy. For each type, the document outlines causes, epidemiology, clinical manifestations, diagnosis, natural history, and treatment.