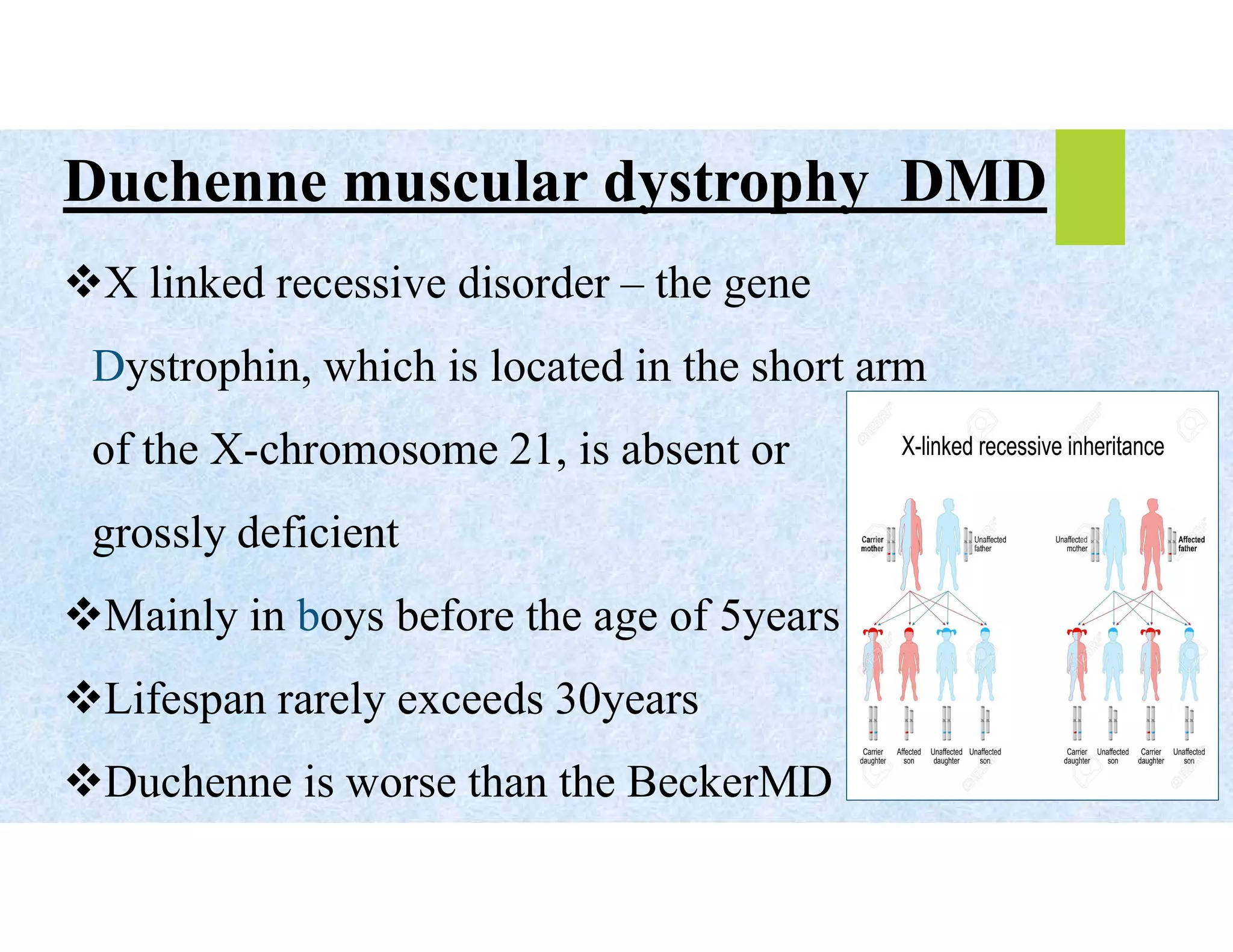
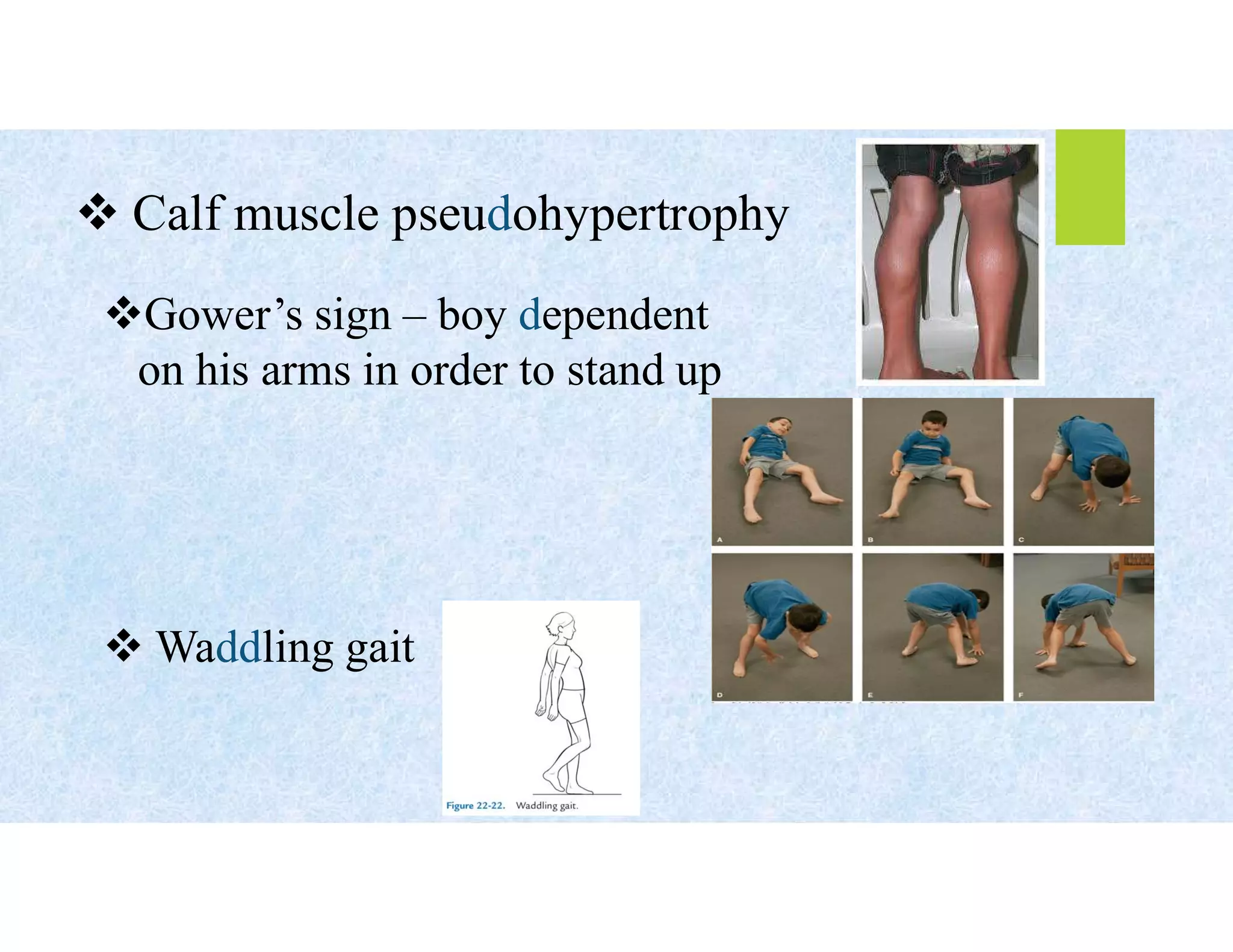
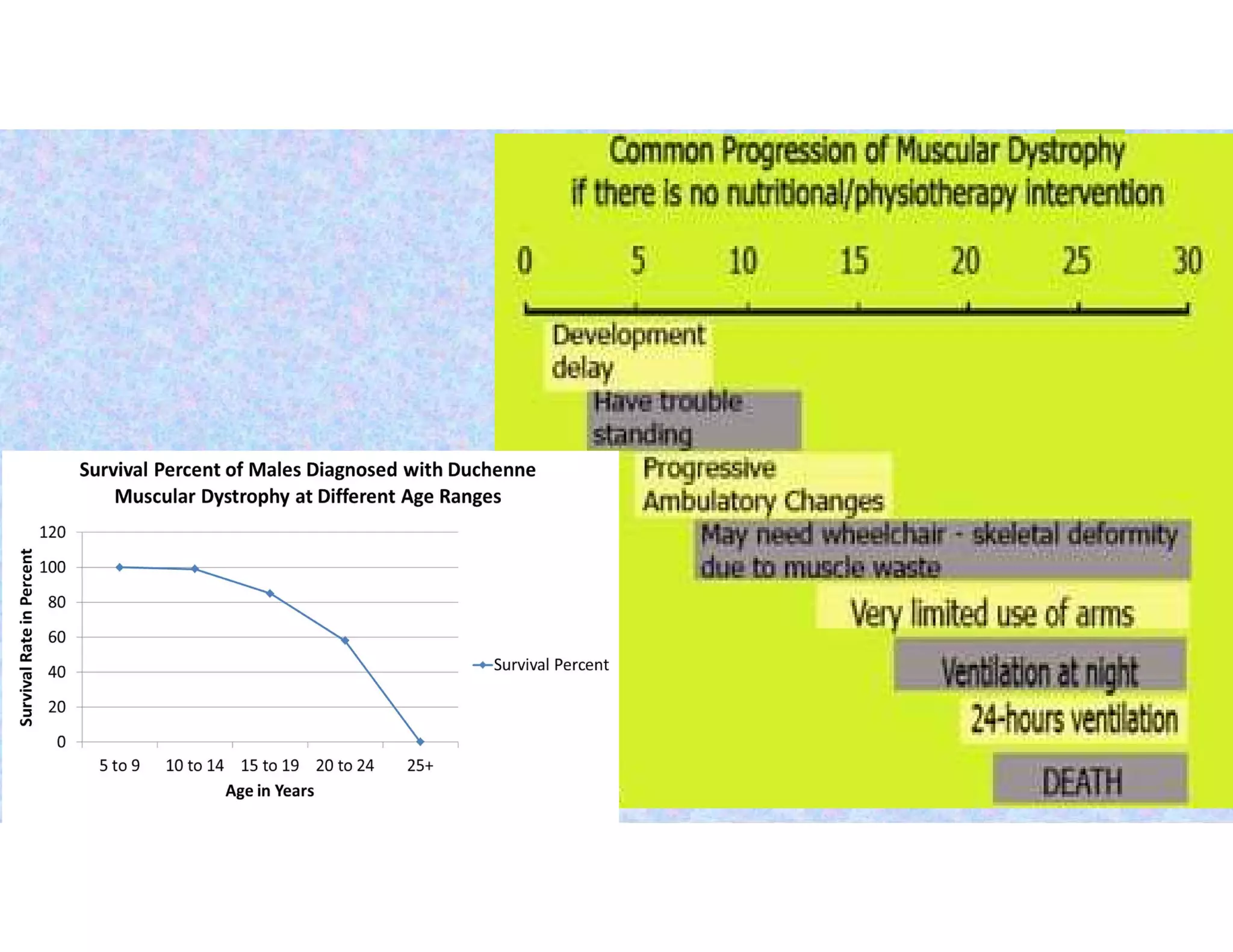
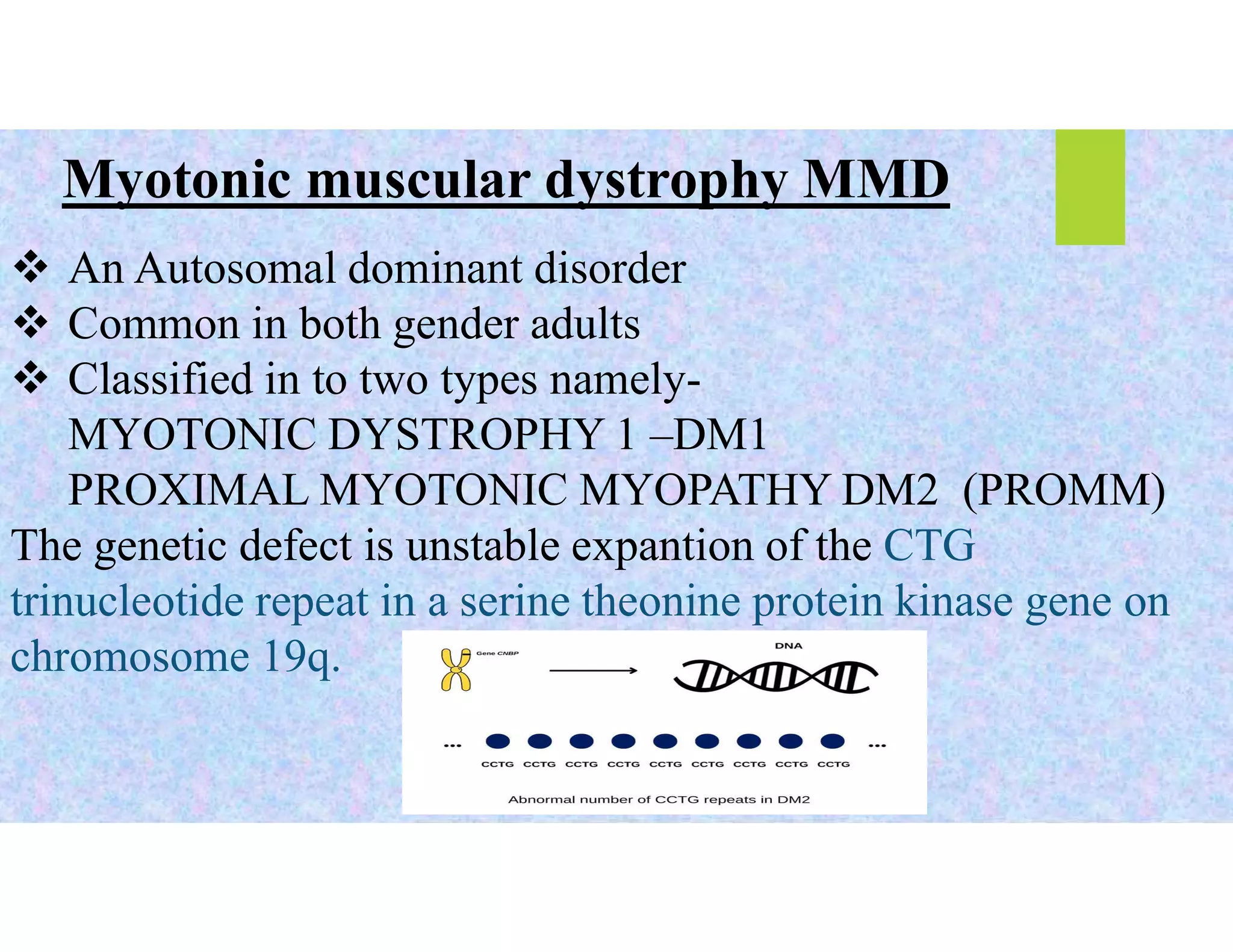
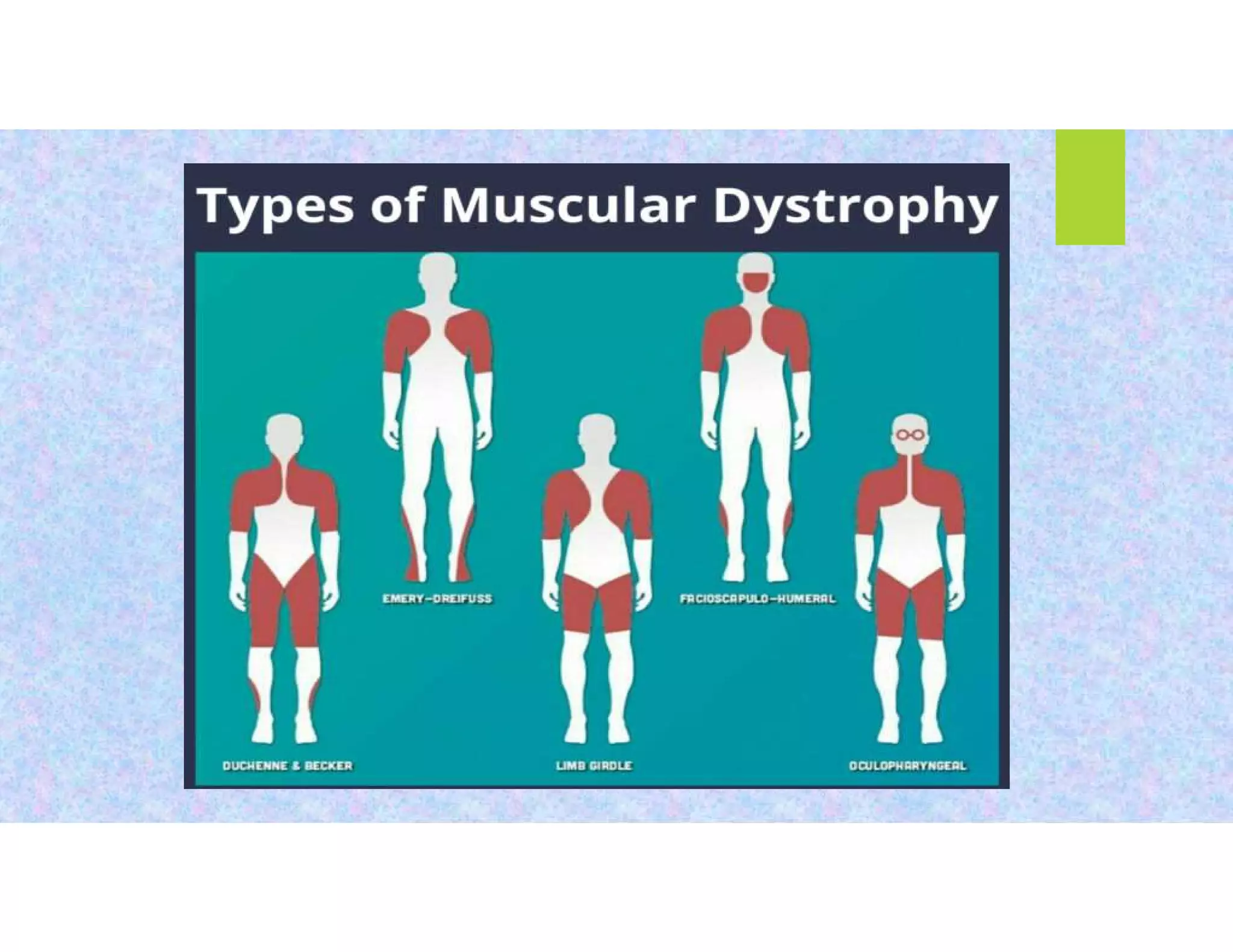
Muscular dystrophy is an inherited group of myopathies characterized by progressive muscle weakness and degeneration, with various types including Duchenne, Becker, and facioscapulohumeral dystrophies. Key features include muscle wasting, joint abnormalities, and associated complications like cardiomyopathy, with treatment options focusing on corticosteroids, gene therapy, and supportive care. Diagnosis typically involves DNA analysis, muscle biopsy, and other clinical assessments to monitor disease progression.