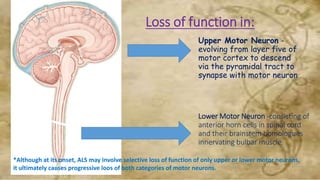
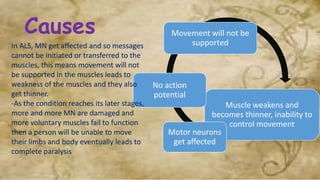
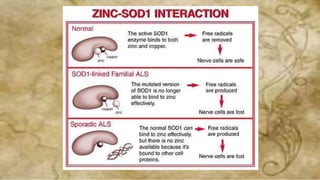
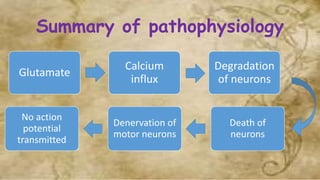
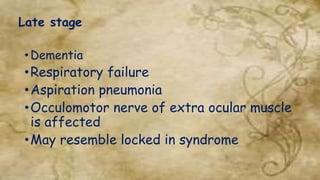
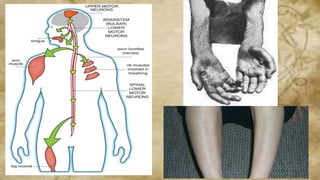
ALS is a progressive neurodegenerative disease that affects motor neurons in the brain and spinal cord. It causes the motor neurons to gradually degenerate and die, resulting in muscle weakness and atrophy. Over time, this leads to increasing paralysis as more motor neurons are damaged. While the exact causes are unknown, excitotoxicity from glutamate and mutations in genes like SOD1 are thought to be involved in the neurodegeneration. The main treatment is riluzole, which extends life by a few months. Other therapies focus on managing symptoms and maintaining function and quality of life for as long as possible. Regular dental care is important for oral health and to reduce risks of pneumonia. Adaptations may be needed to accommodate physical