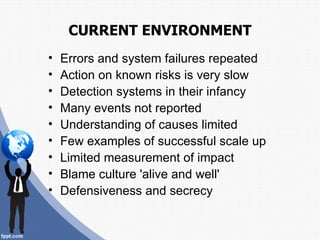
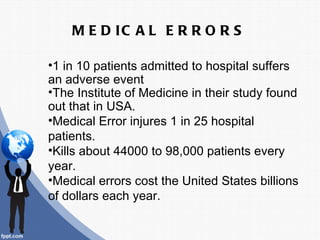
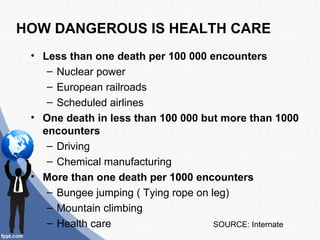
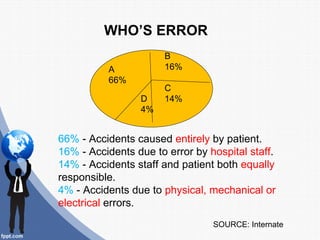
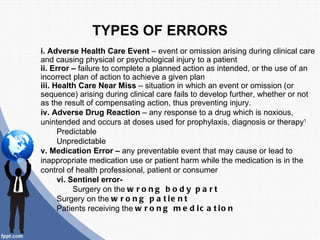
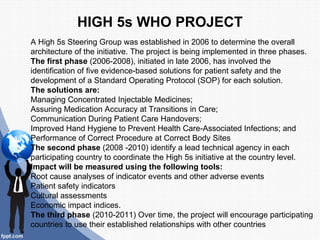
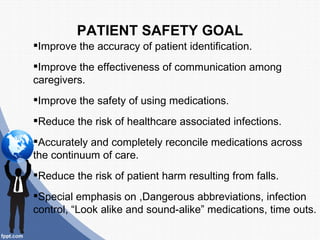
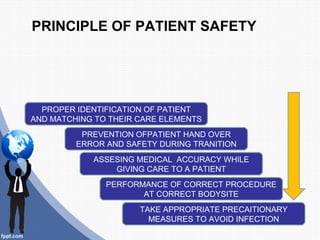
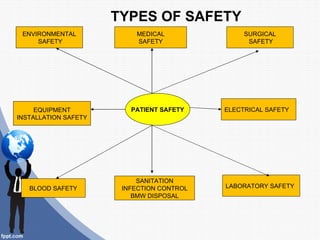
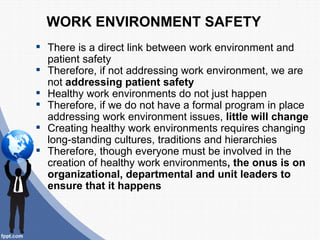
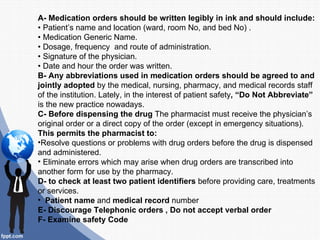
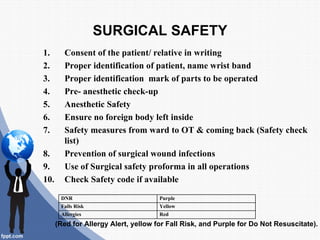
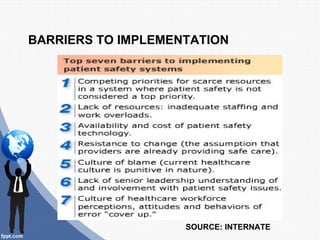
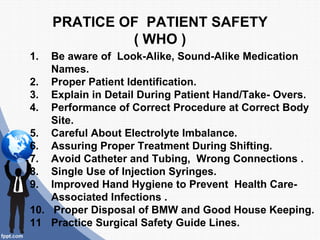
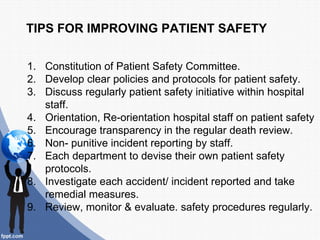
The document discusses the importance of patient safety in healthcare, outlining key concepts, types of errors, and systems in place to prevent harm to patients. It emphasizes the need for a blame-free culture, effective communication, and systemic improvement to reduce medical errors, which significantly impact patient outcomes. The World Health Organization's initiatives and guidelines are also highlighted as essential frameworks for enhancing safety measures in healthcare settings.