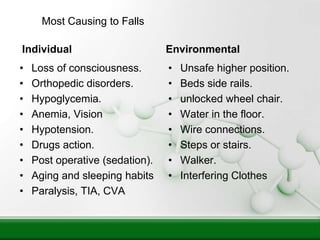
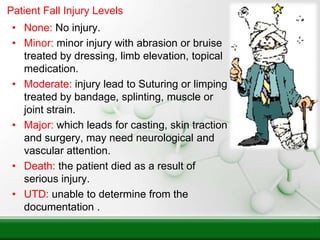
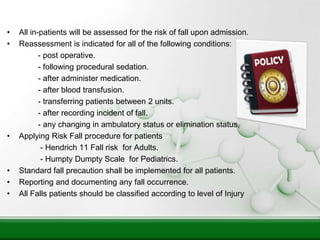
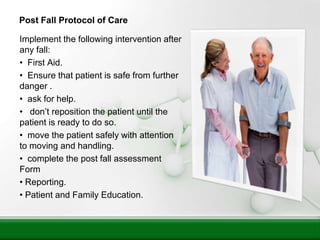
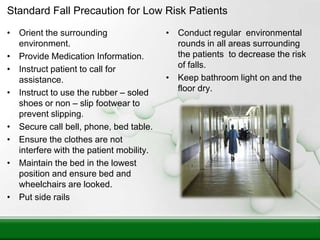
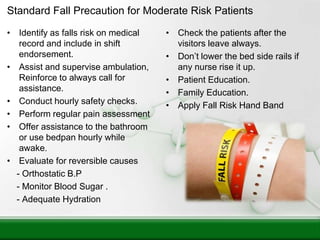
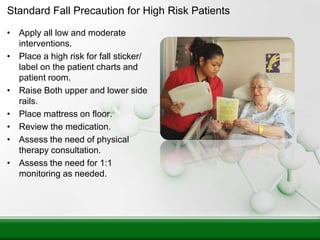
This document outlines a falls prevention program with the objectives of maintaining patient safety, reducing injury risk, and determining how falls occur. It defines falls and near falls, identifies individual and environmental risk factors, and describes a protocol for assessing falls risk upon admission and after changes. The protocol includes implementing standard precautions like raising bed rails, hourly checks, and education for low, moderate, and high risk patients. It also describes post-fall care and reporting procedures.