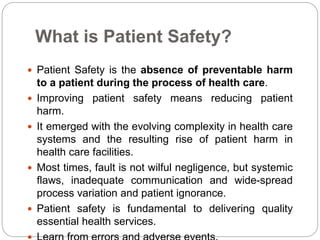
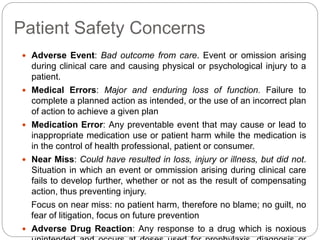
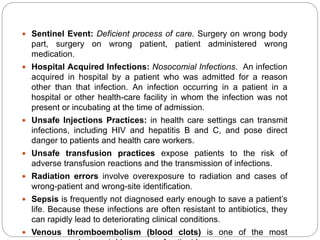
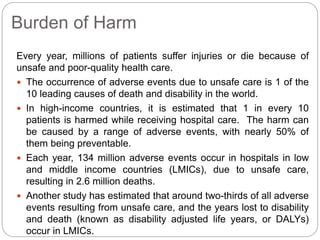
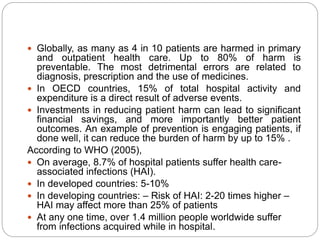
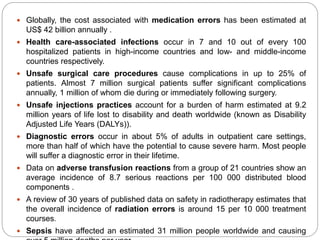
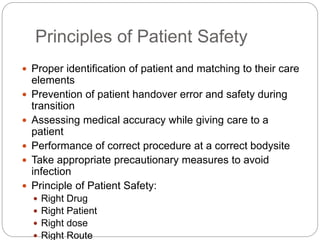
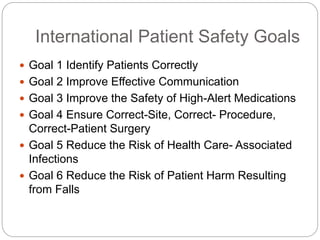
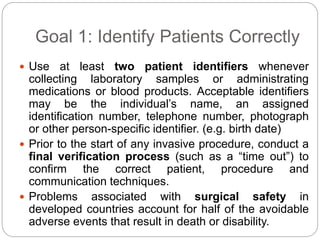
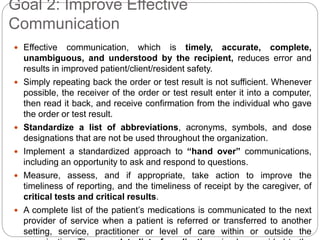
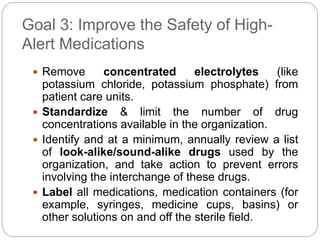
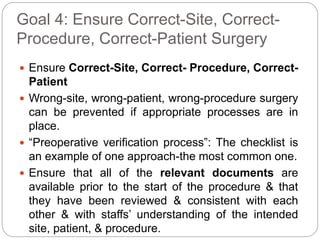
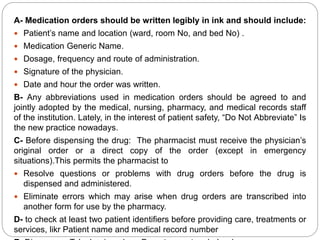
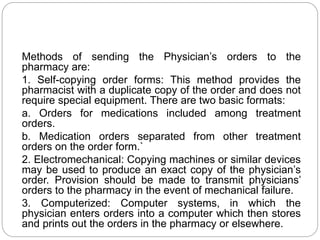
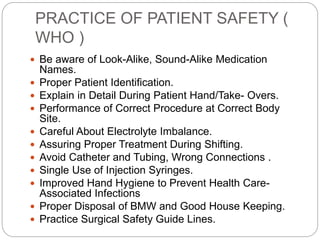
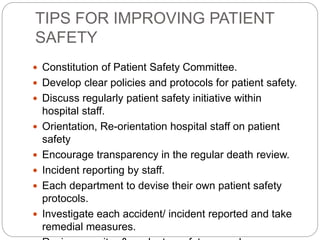
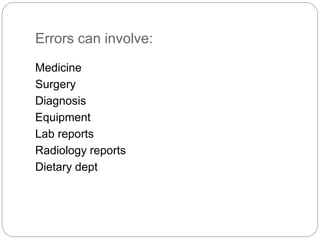
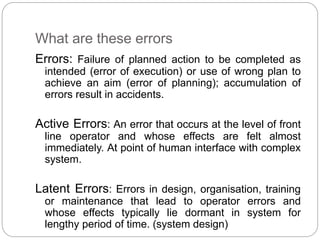
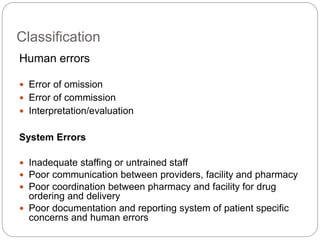
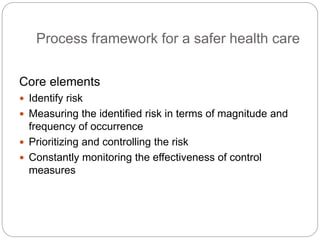
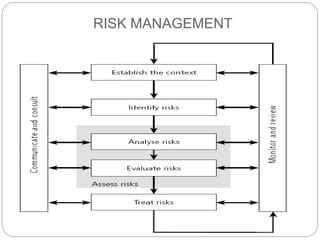
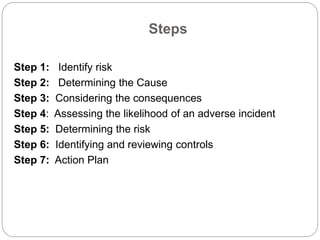
This document discusses patient safety in healthcare. It defines patient safety as the absence of preventable harm during healthcare. It notes that most patient harm is due to systemic flaws rather than individual negligence. It then discusses various types of patient safety concerns like medical errors, adverse events, infections, and falls. International patient safety goals are also presented, such as properly identifying patients, improving communication, and reducing healthcare-associated infections. The document emphasizes that improving safety requires efforts across many areas to protect patients from harm.