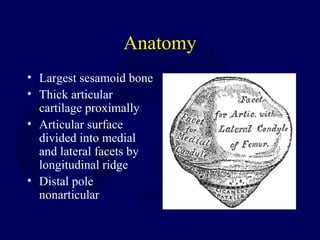
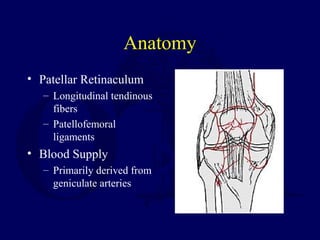
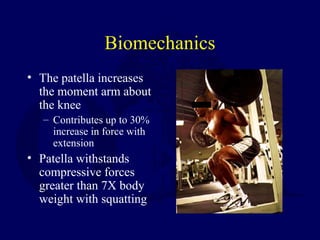
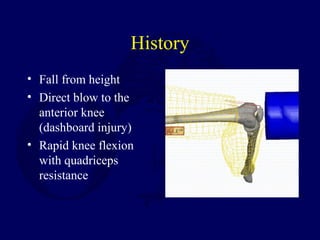
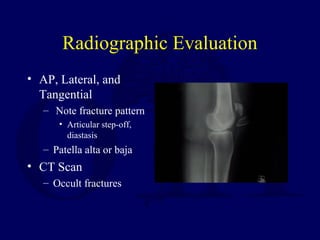
The document discusses injuries to the patella and extensor mechanism. It describes the anatomy and biomechanics of the patella. Common injury mechanisms are direct trauma from a fall or dashboard injury, or indirect trauma from forceful knee flexion against a contracted quadriceps. Injuries can include fractures or ruptures of the patella or tendons. Treatment depends on the specific injury but may involve nonoperative management with immobilization or operative fixation or reconstruction of bony or soft tissue injuries.