Patella fractures and extensor mechanism injuries are summarized as follows:
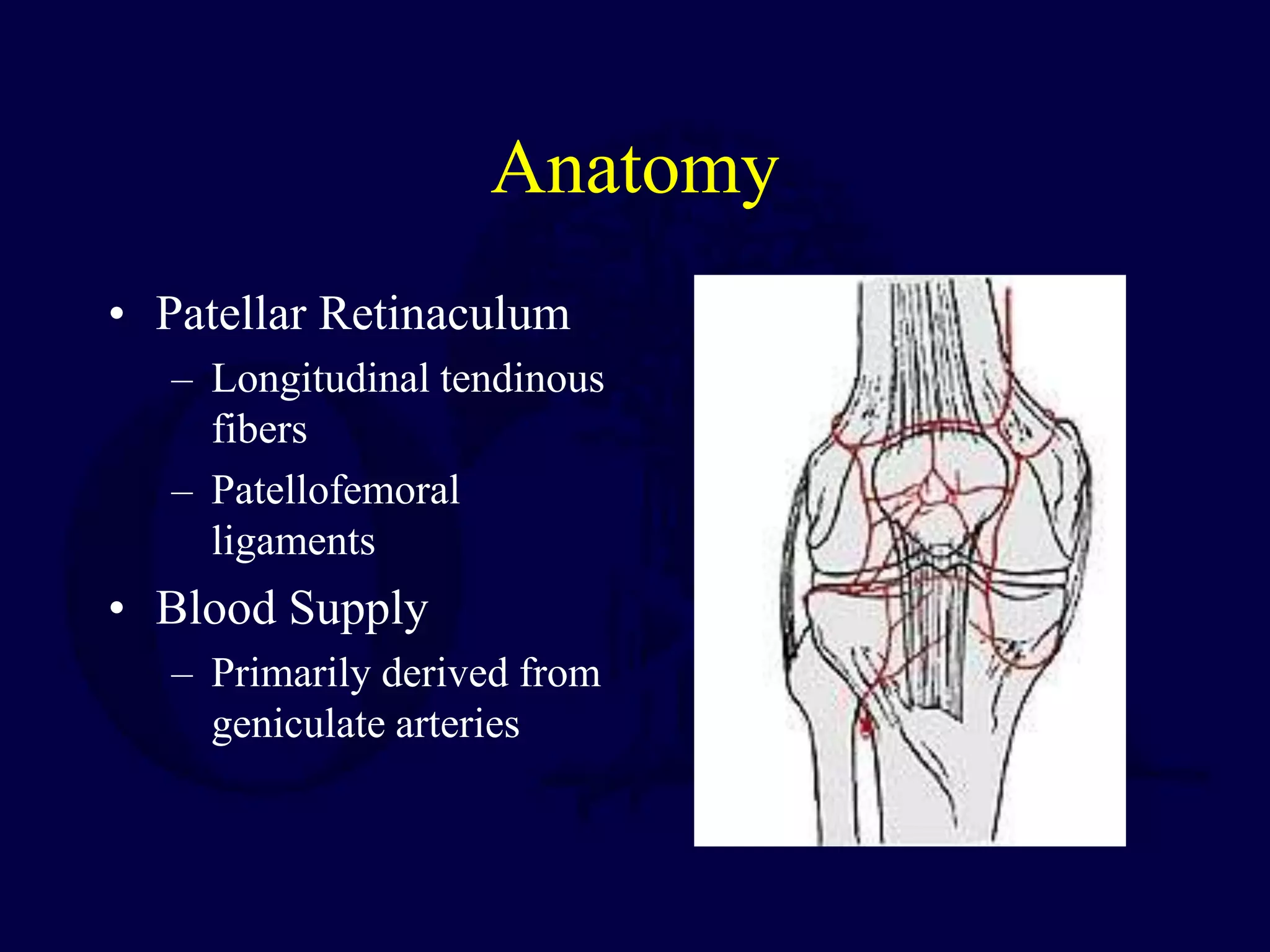
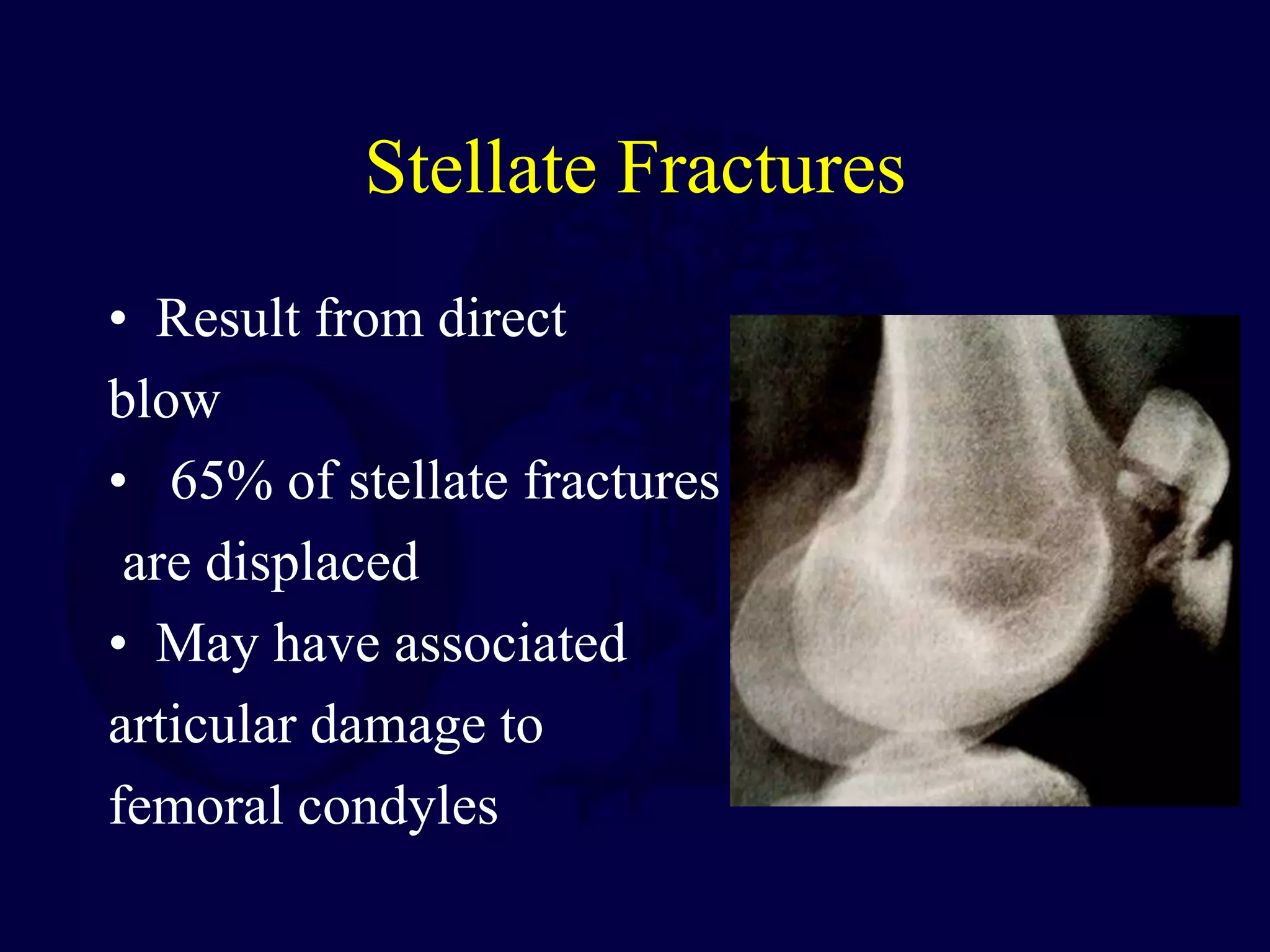
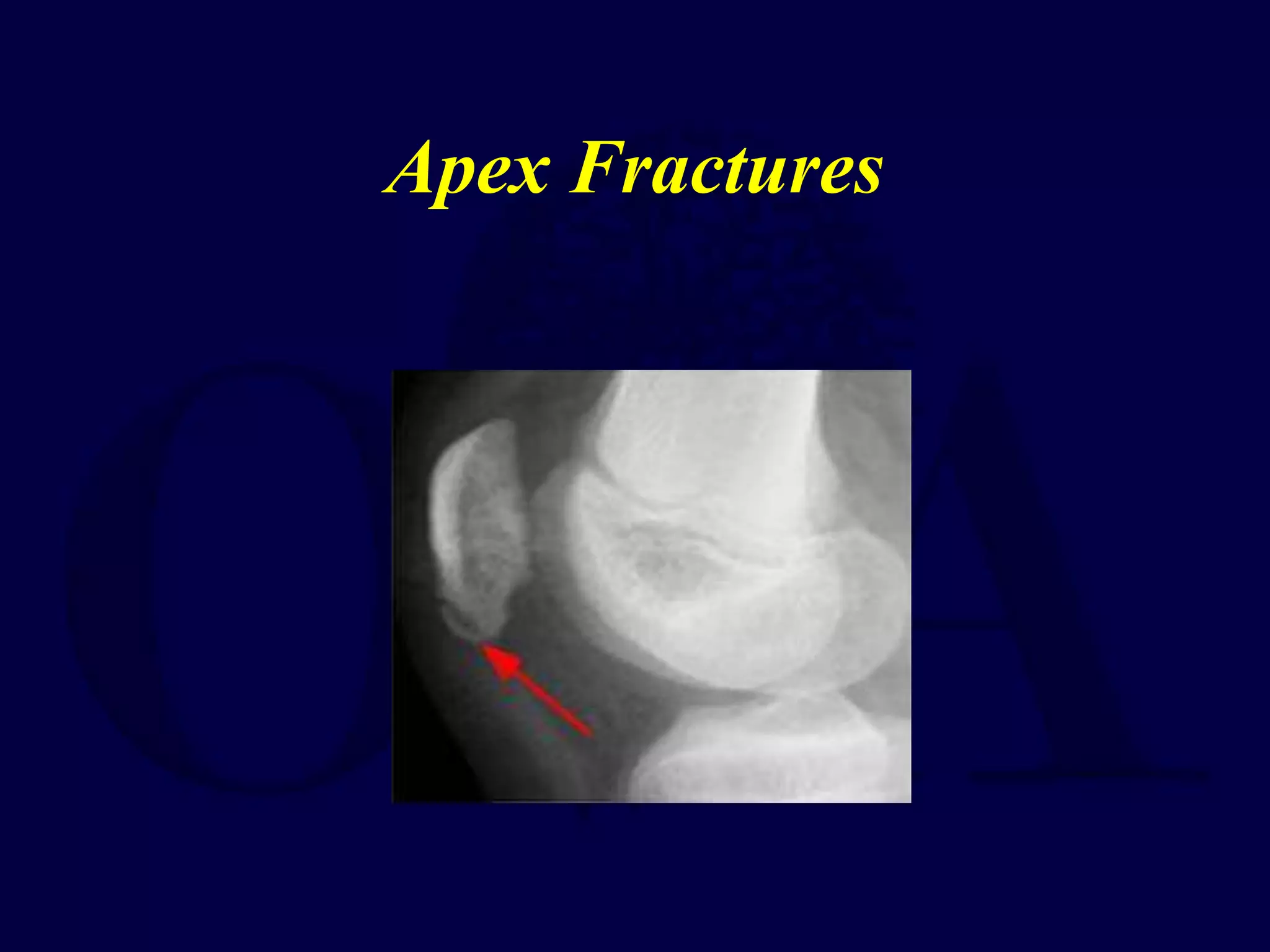
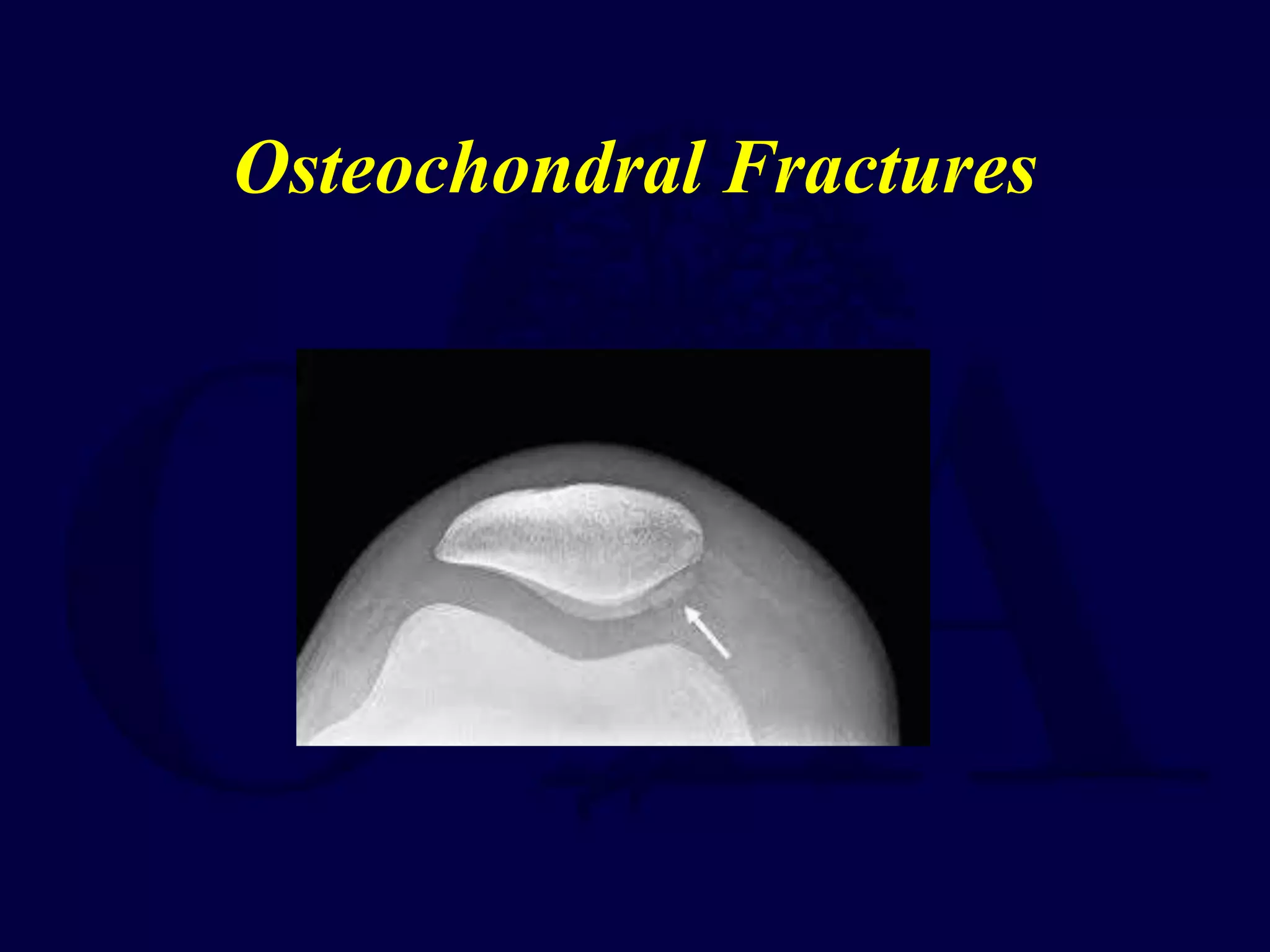
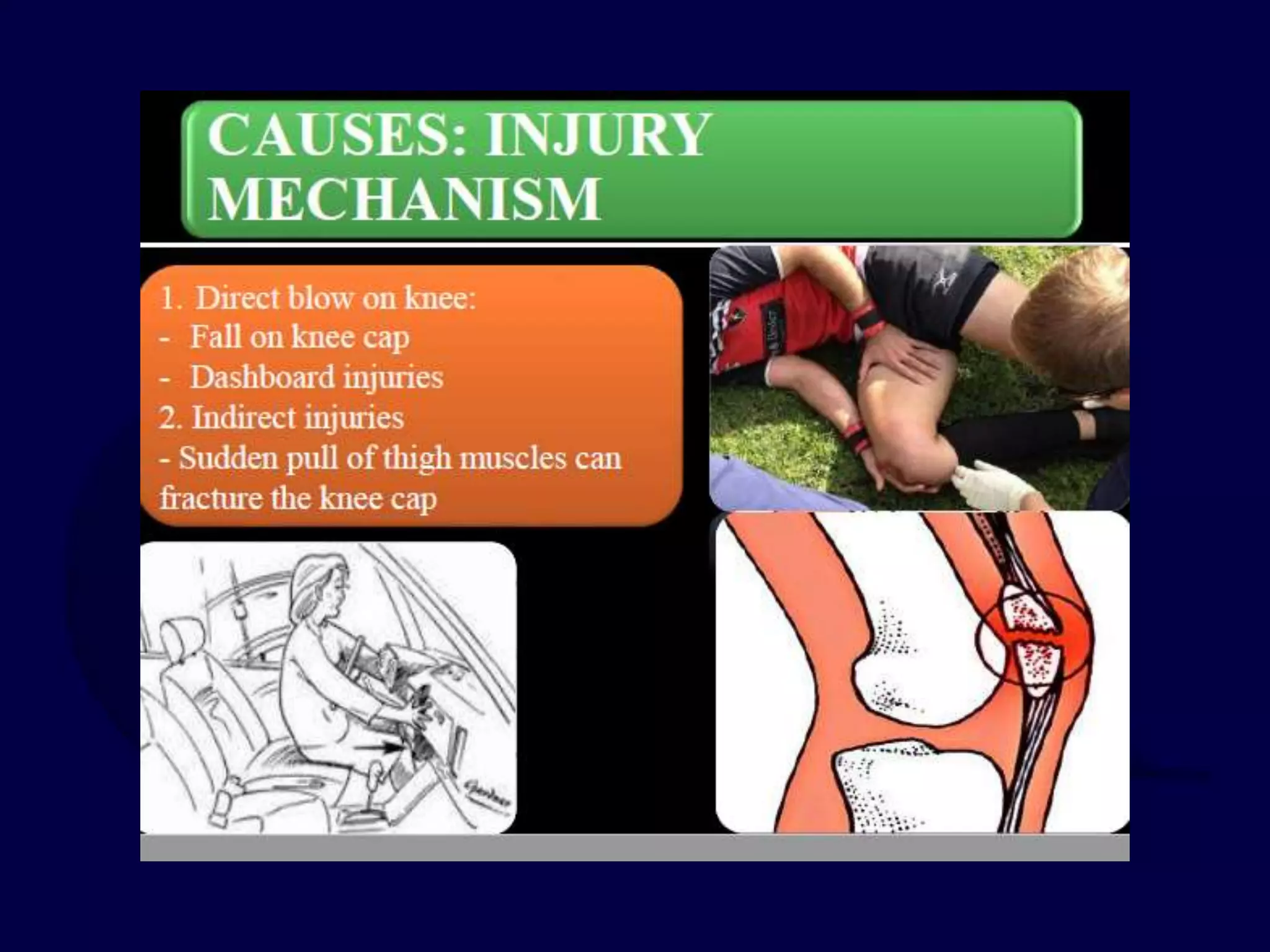
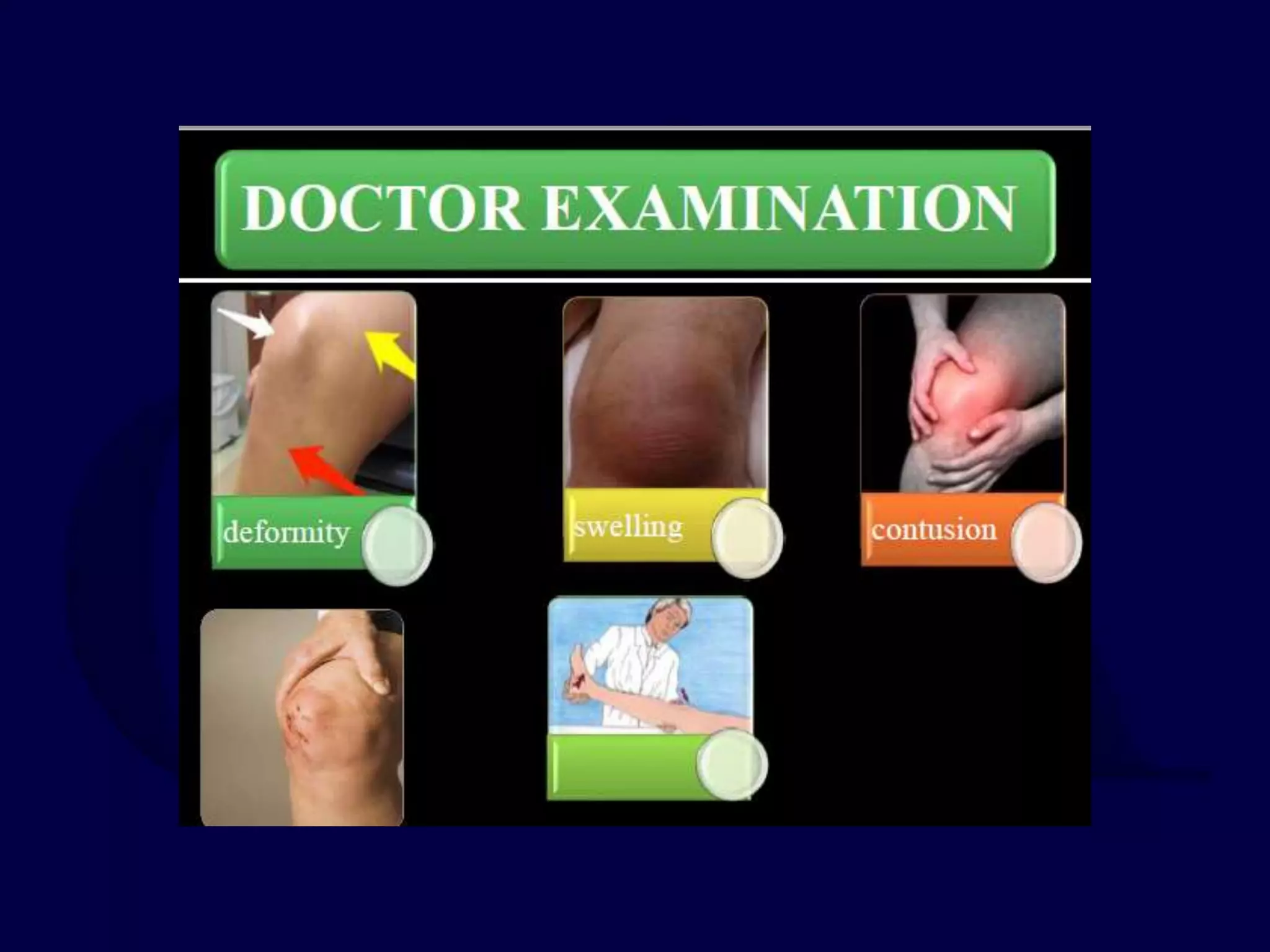
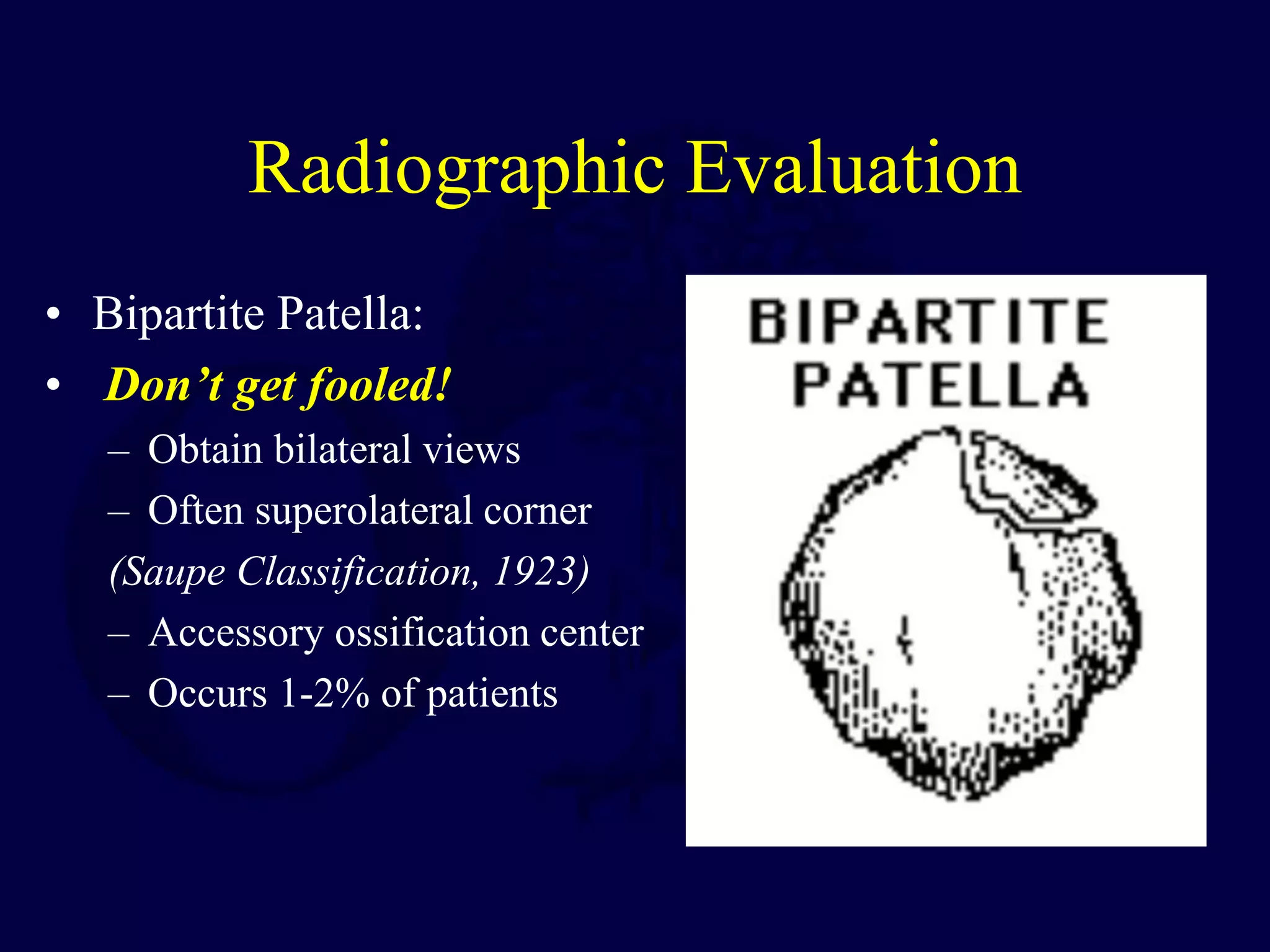
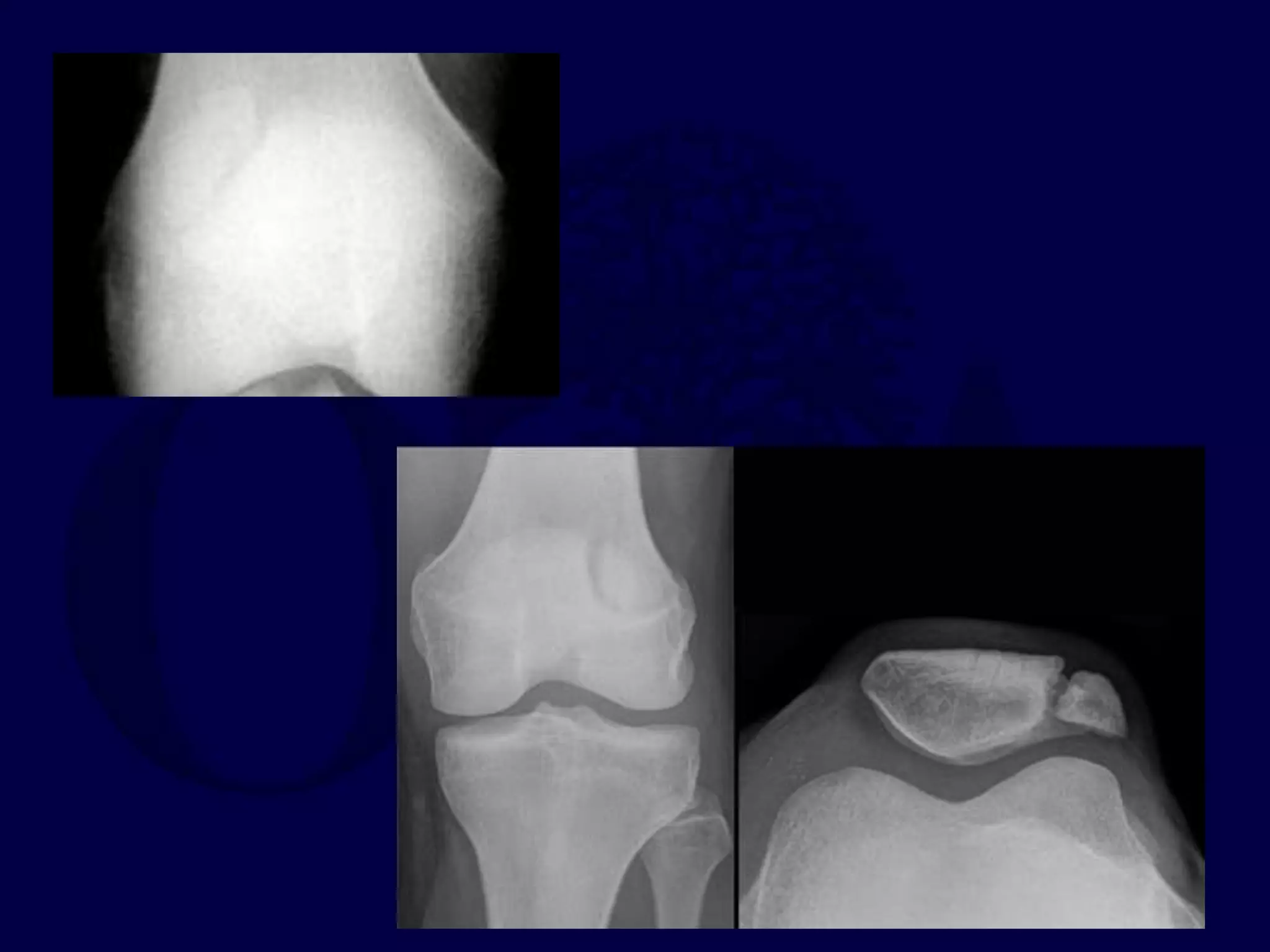
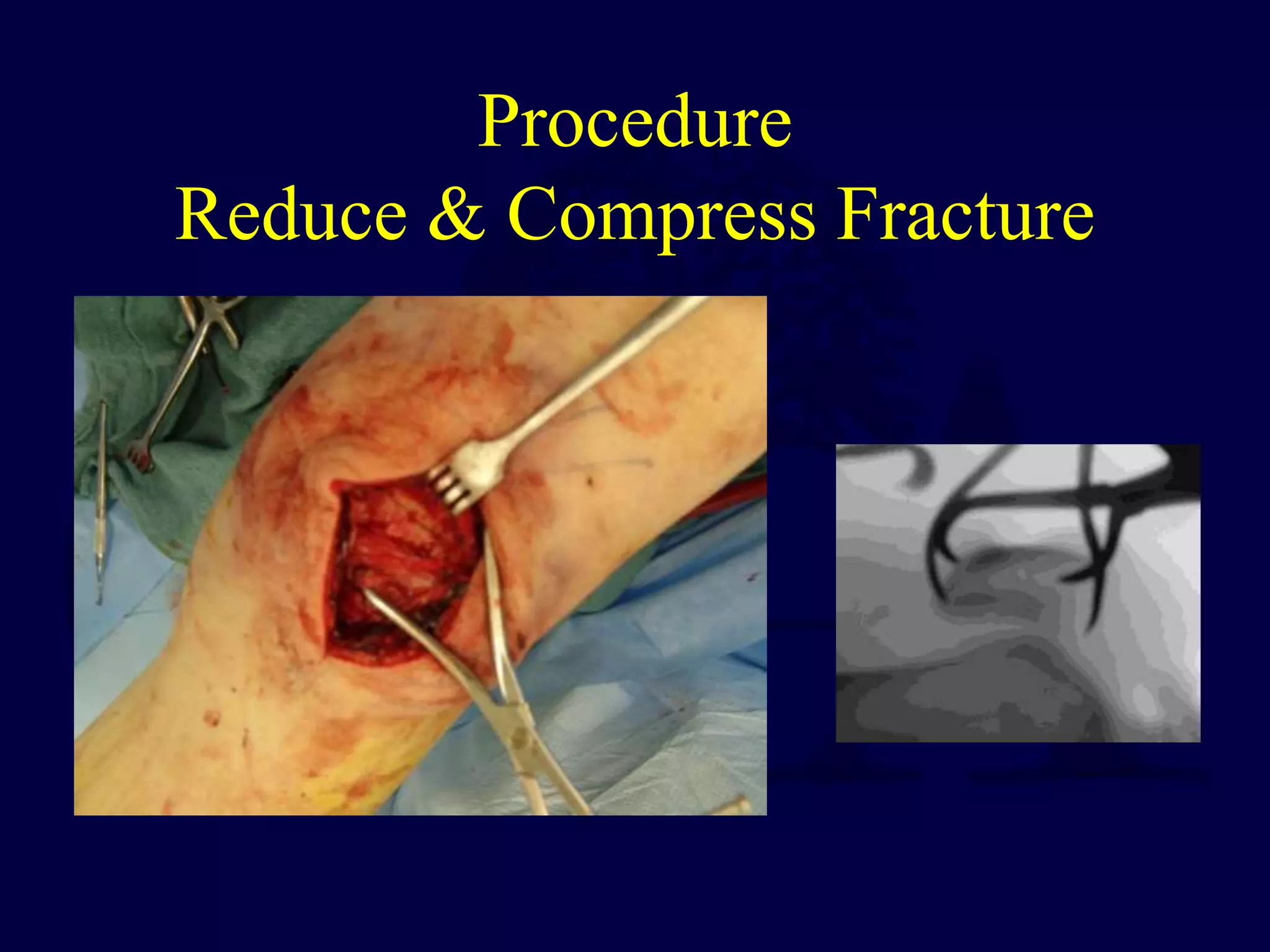
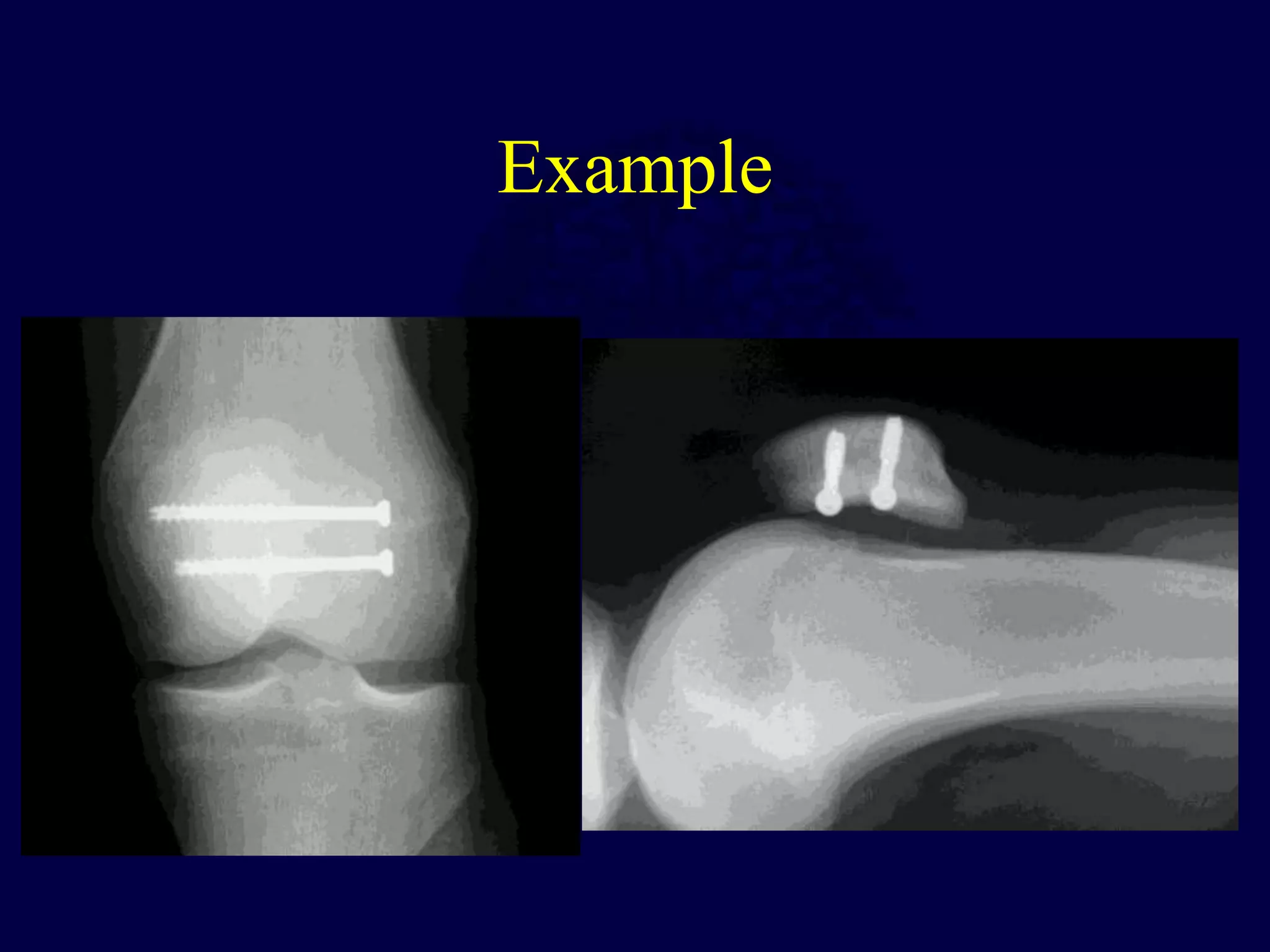
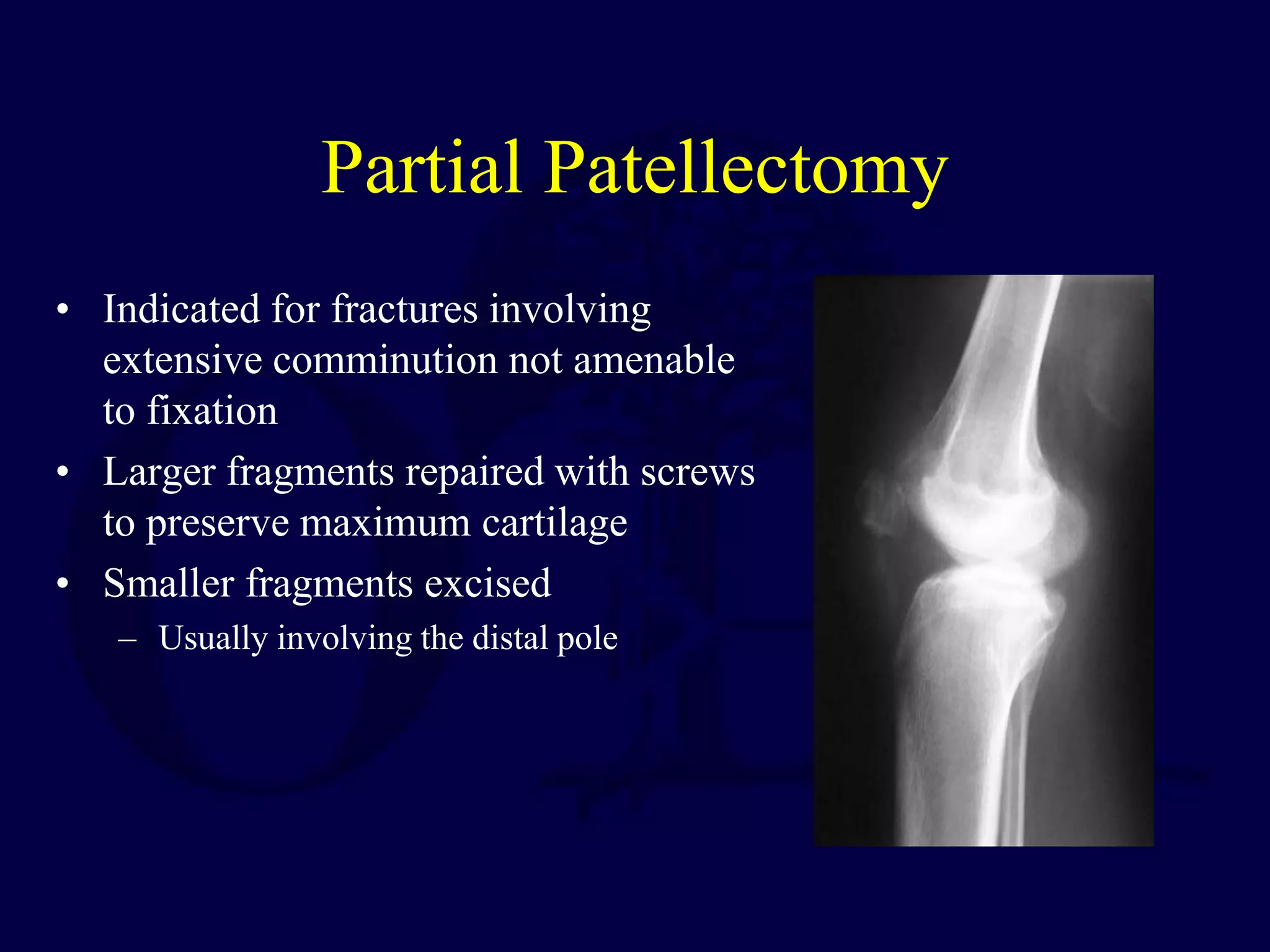
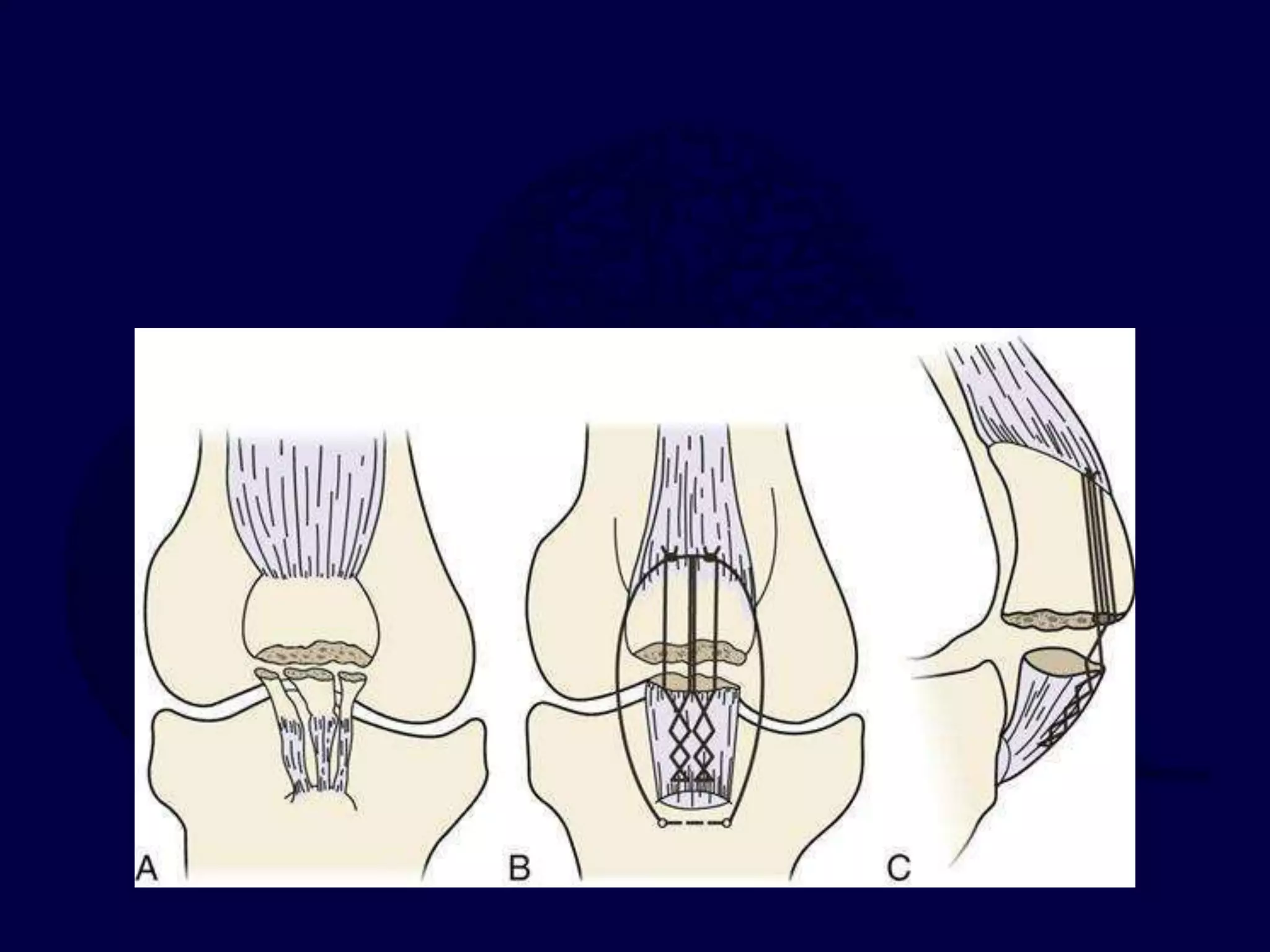
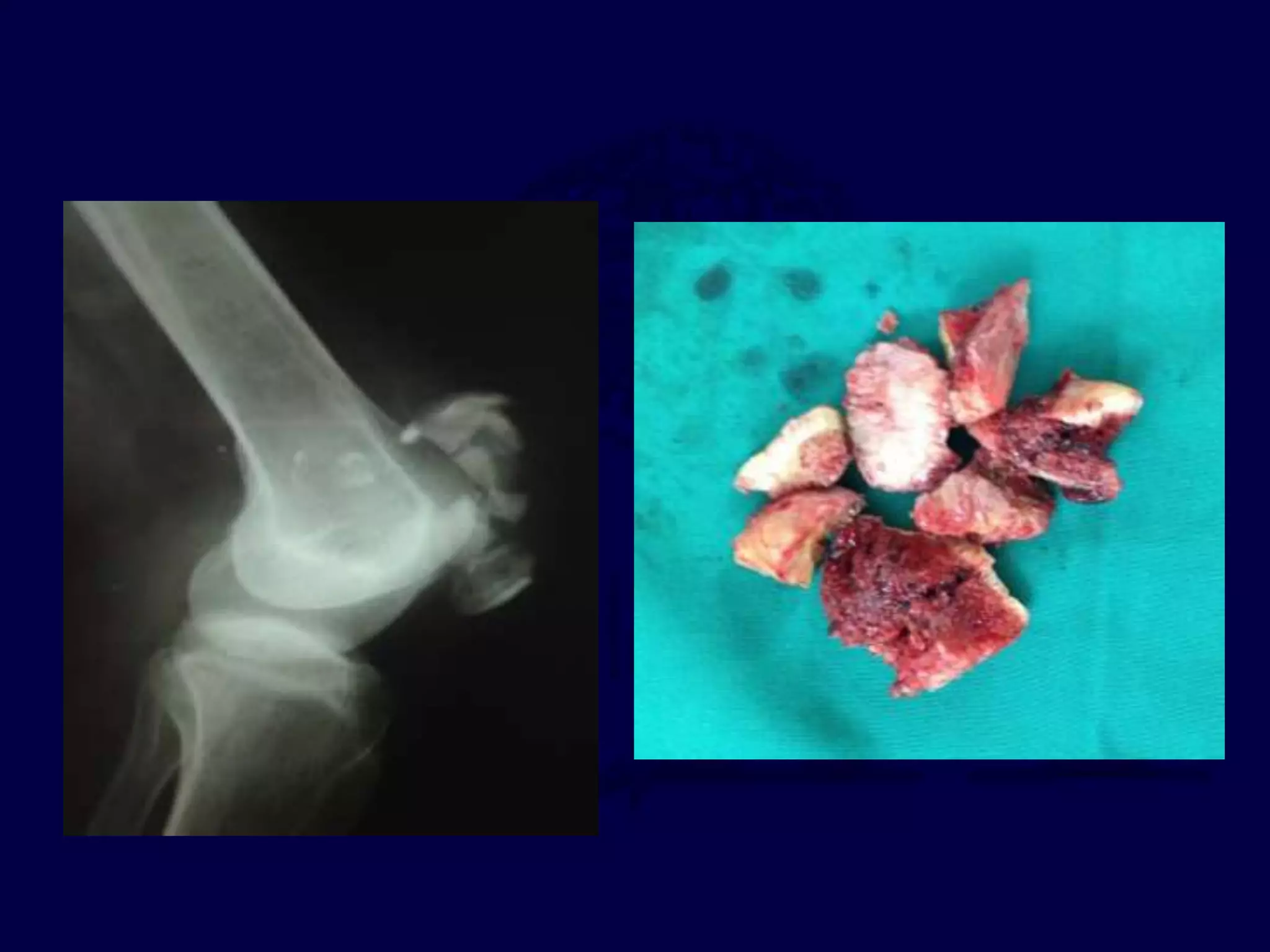
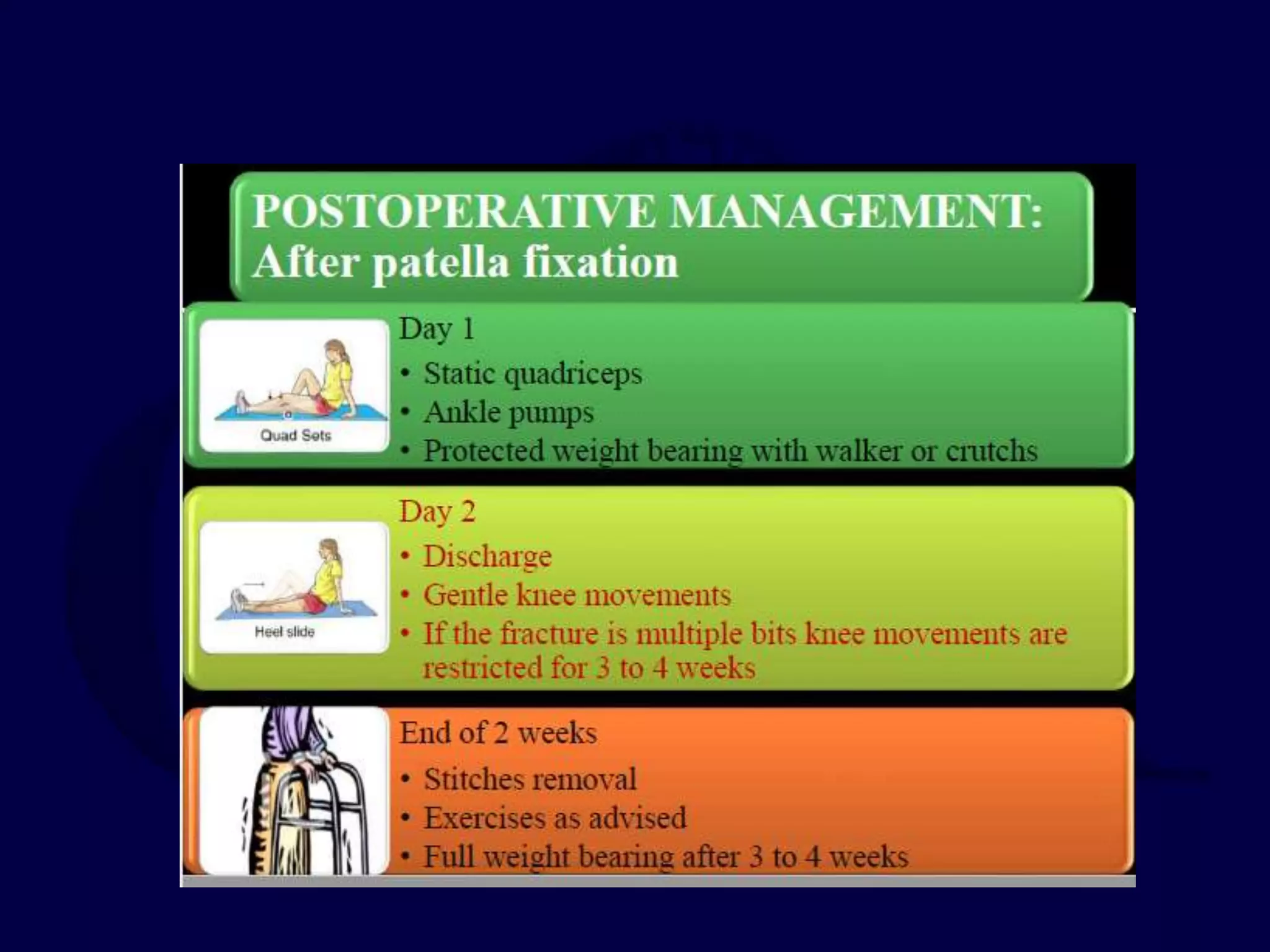
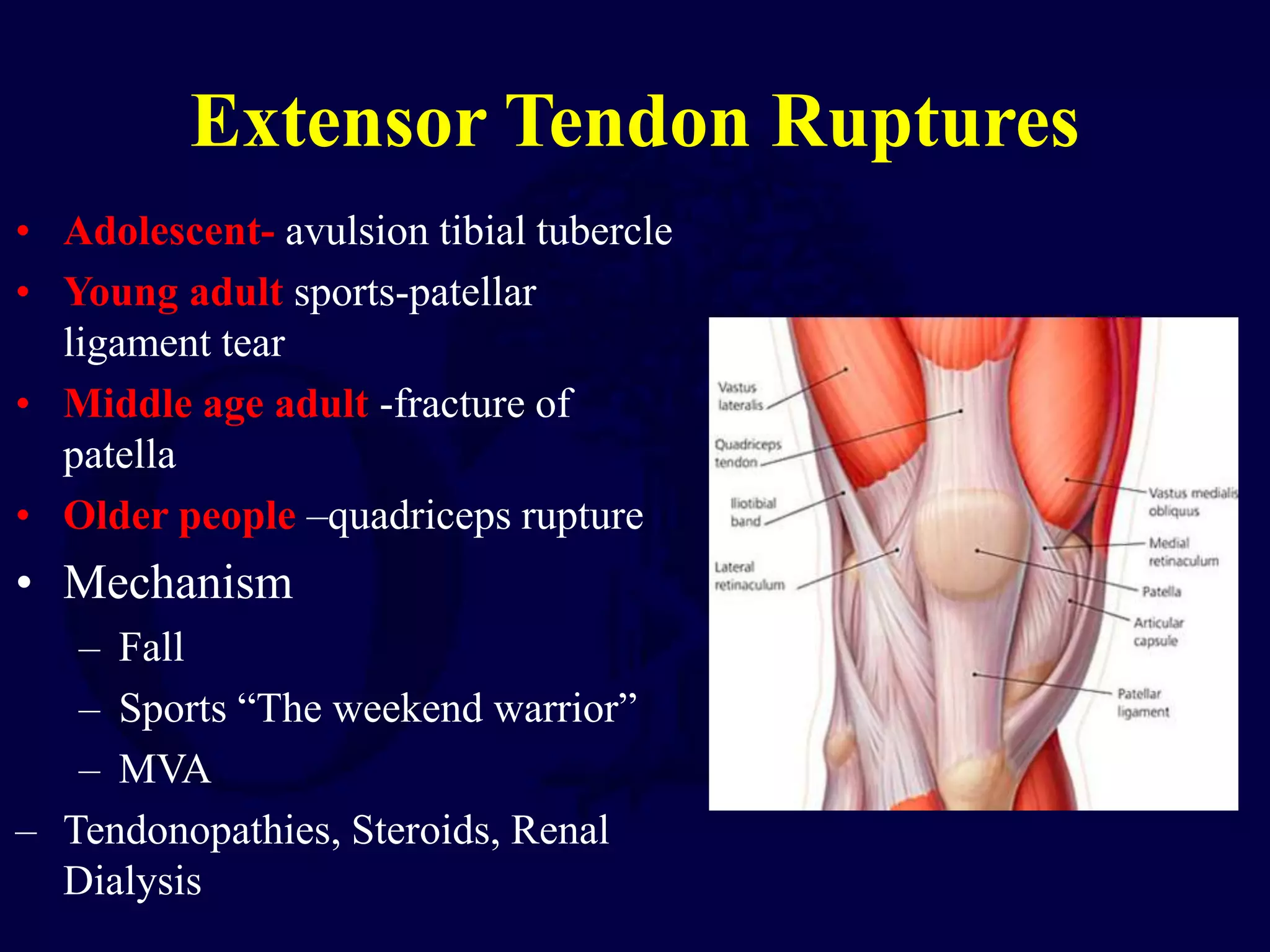
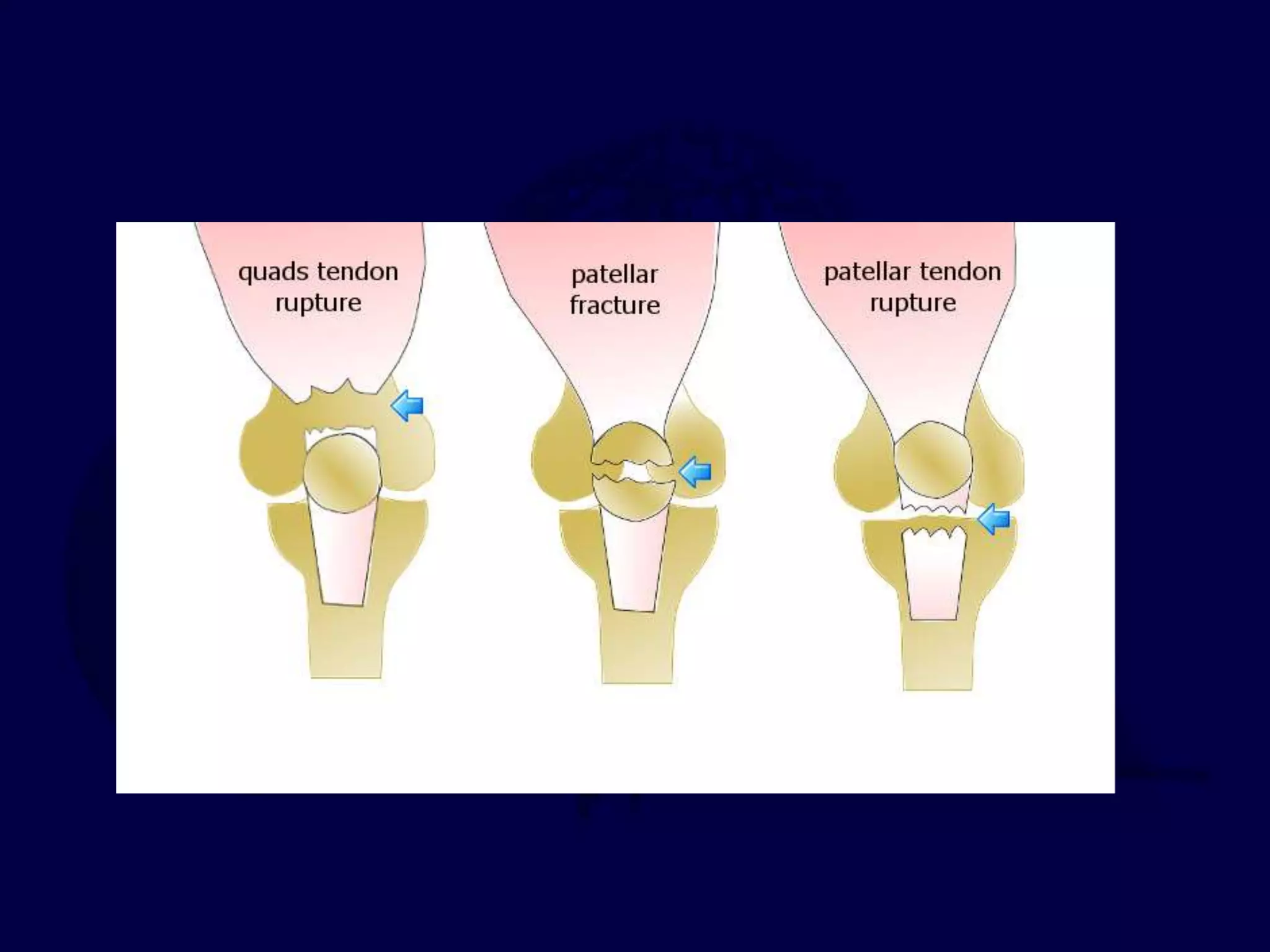
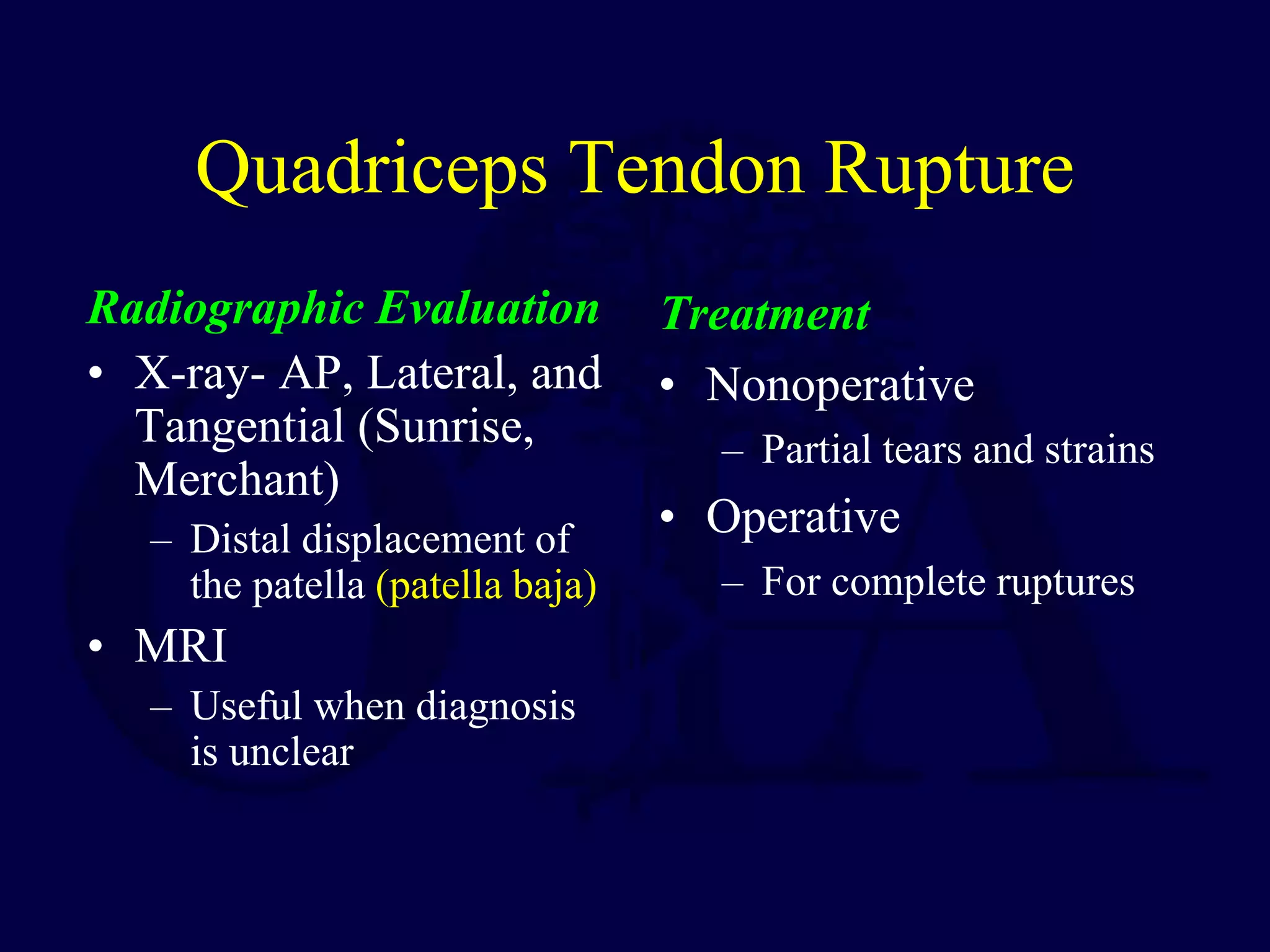
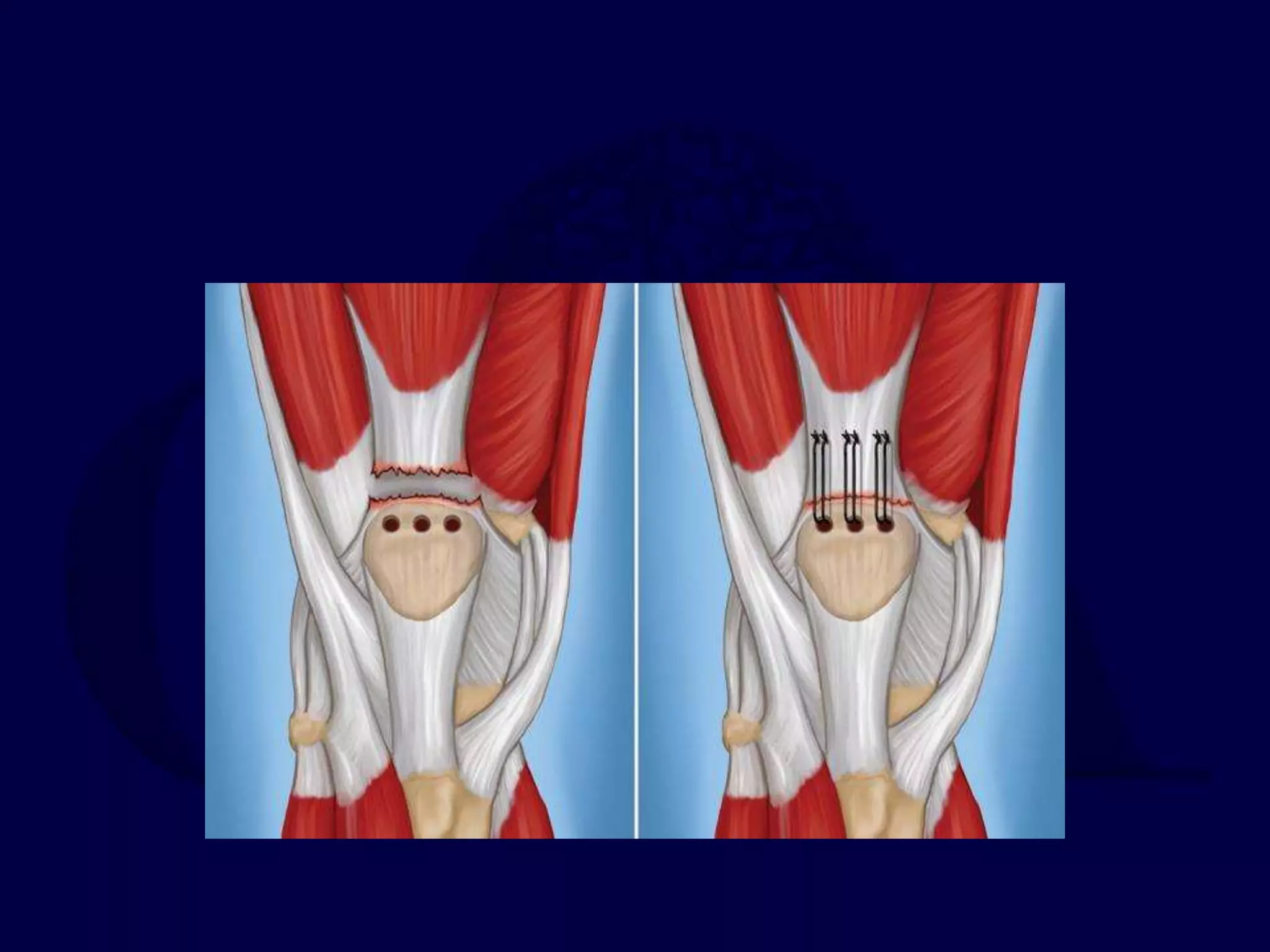
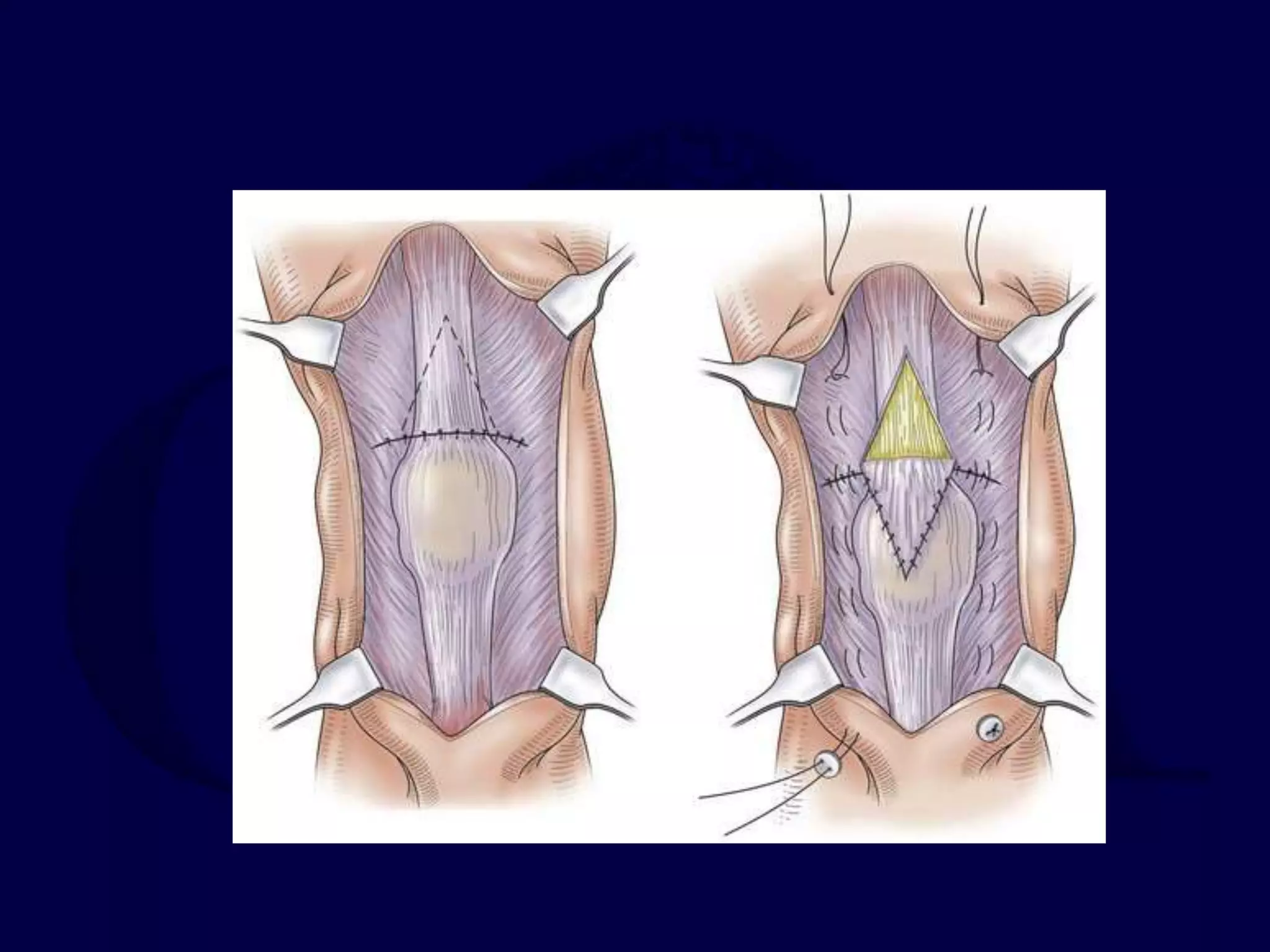
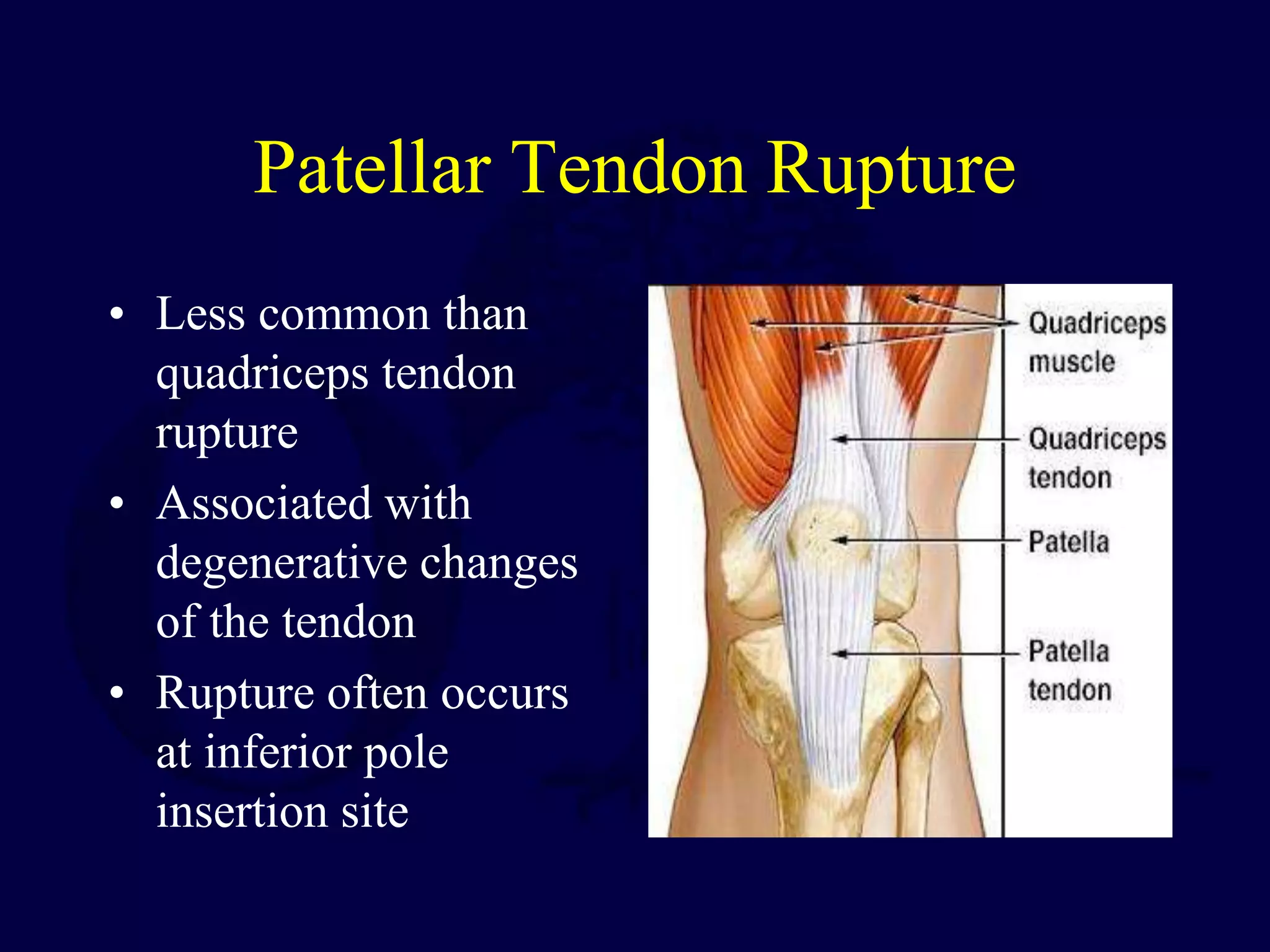
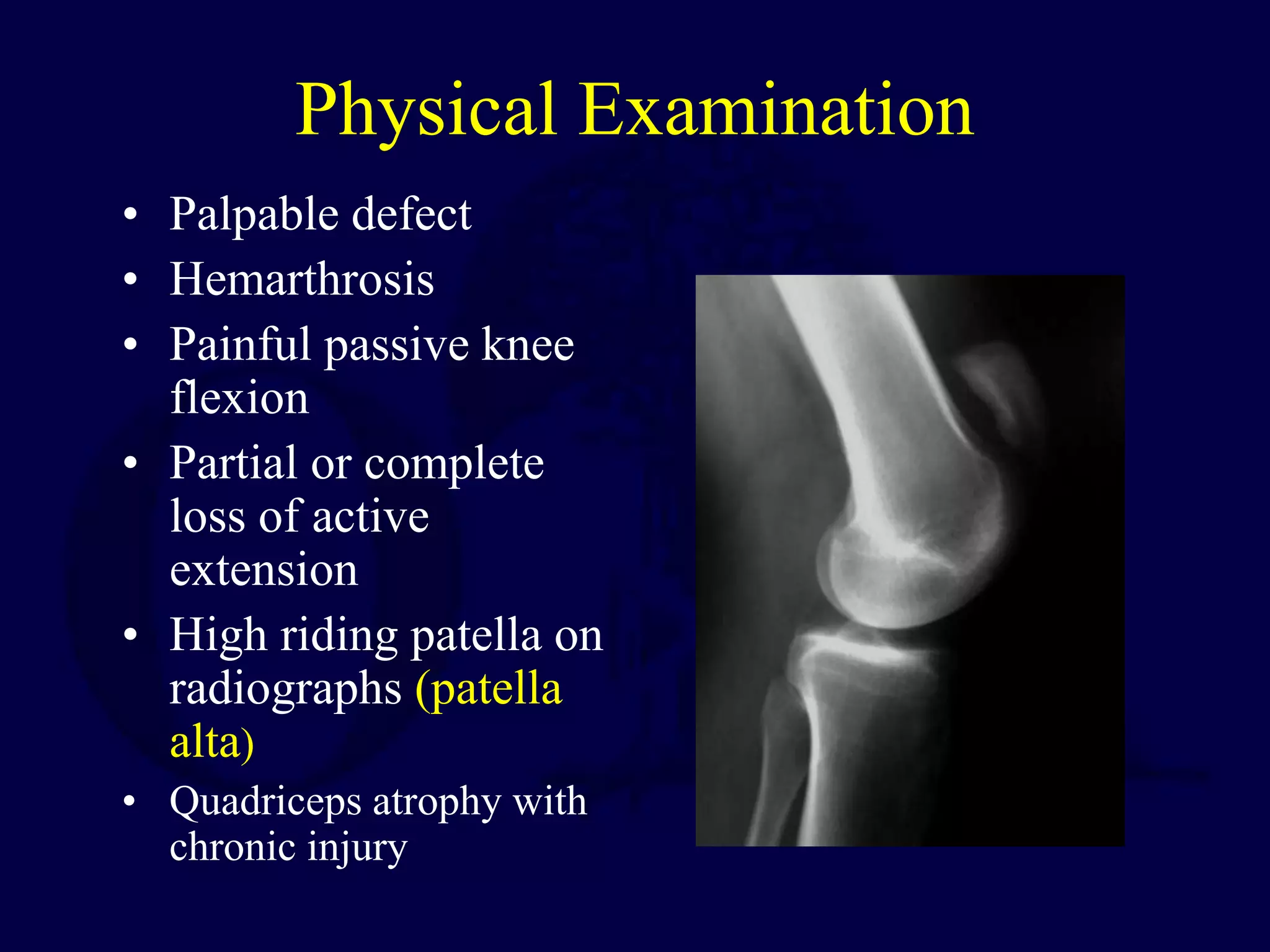
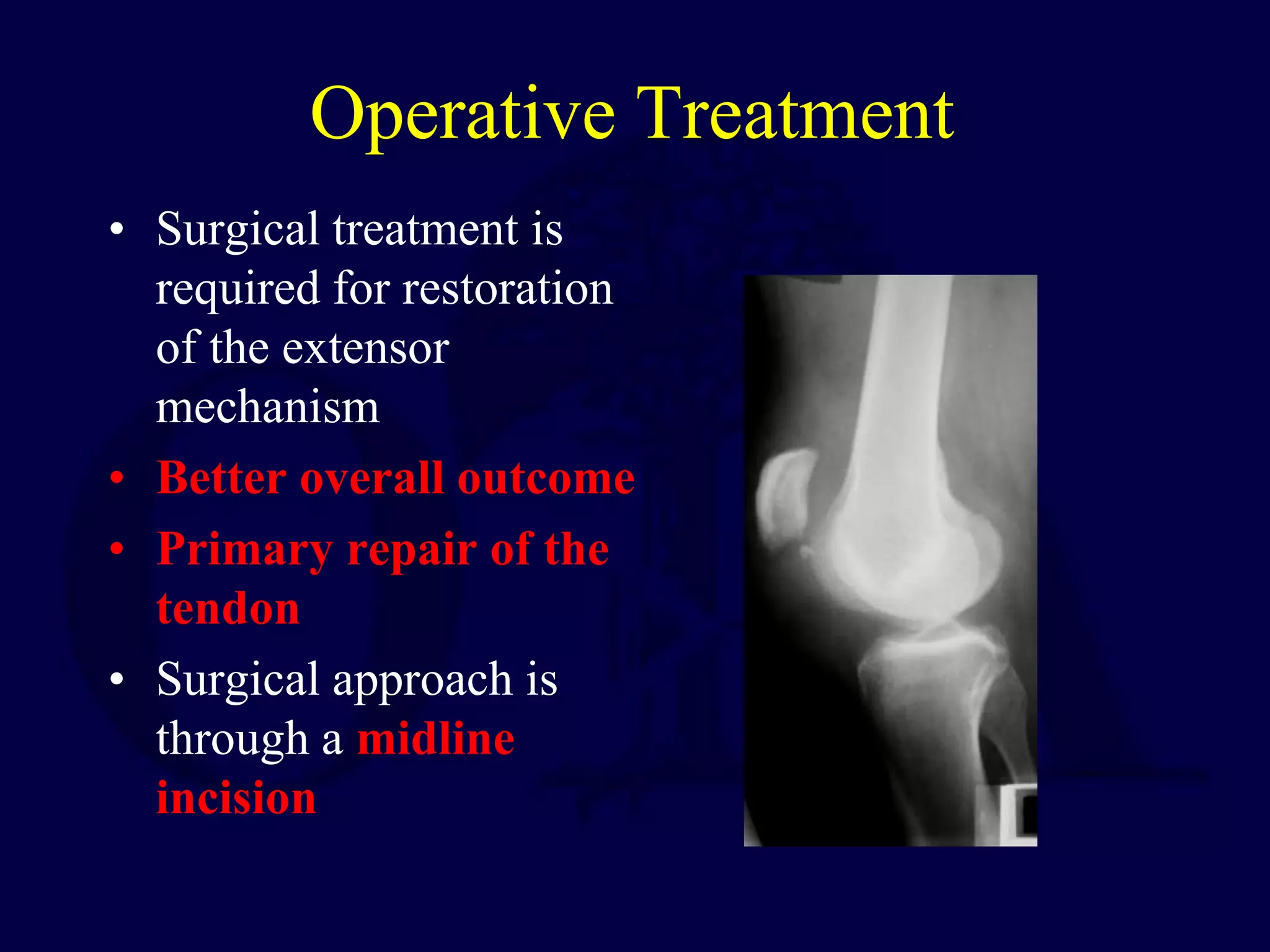
The patella is subject to significant forces and increases the leverage of the quadriceps muscle. It can fracture or the extensor mechanism can tear. Fractures are classified based on pattern and displacement. Nondisplaced fractures are treated non-operatively while displaced fractures often require surgery like tension band wiring or screws to restore function. Extensor mechanism injuries like quadriceps tendon tears are also common and may require surgical repair. Complications can include stiffness, infection, and arthritis if not properly treated.