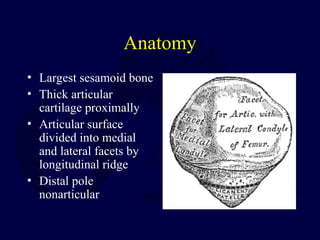
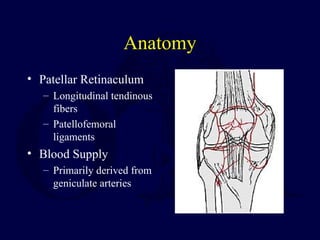
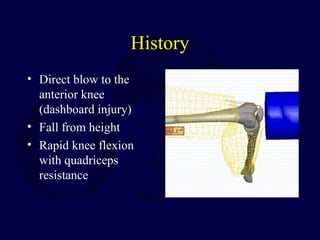
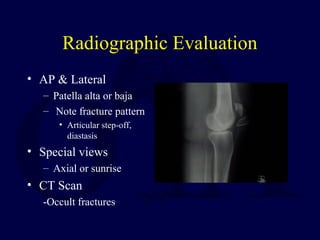
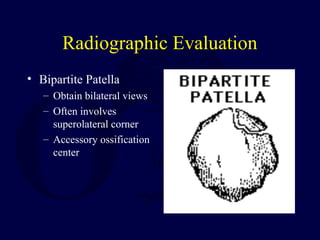
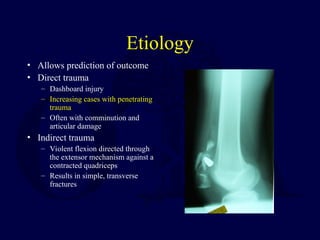
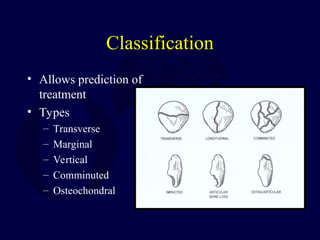
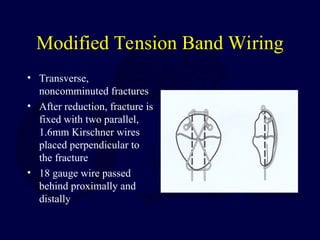
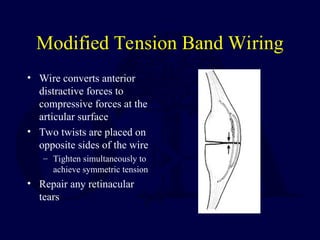
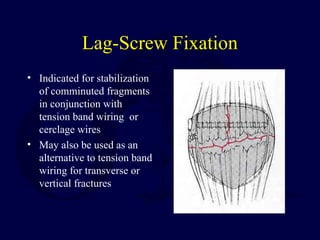
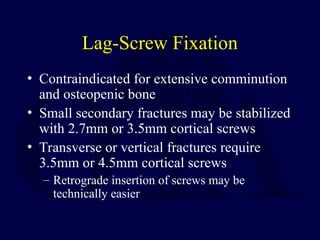
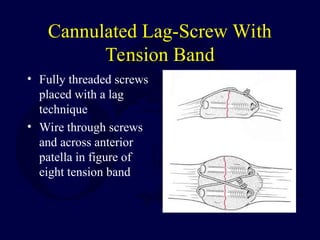
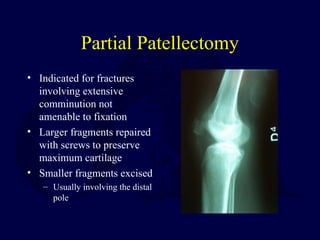
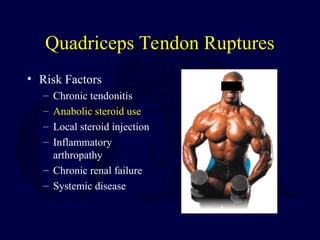
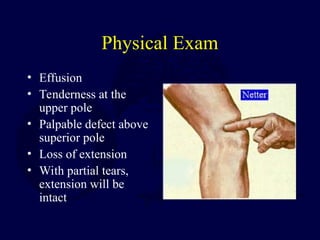
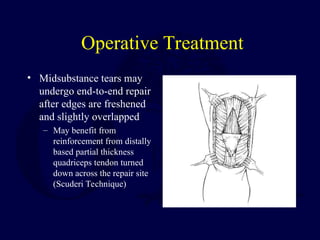
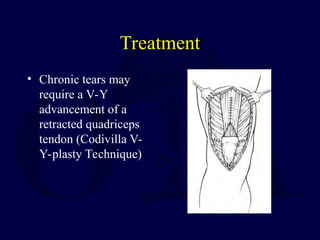
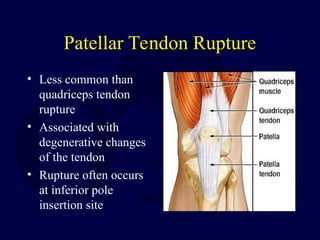
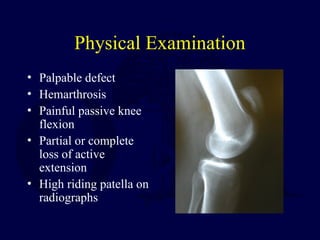
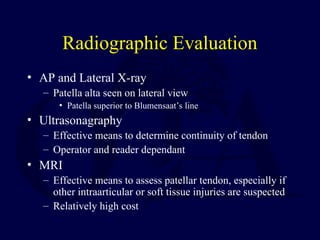
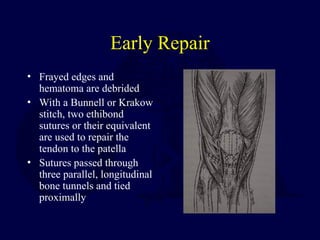
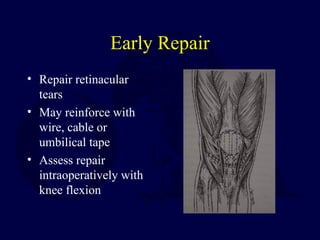
The document discusses patella fractures and extensor mechanism injuries, detailing anatomy, biomechanics, causes, examination techniques, classification, and treatment options. It outlines nonoperative and operative approaches to managing these injuries, including specific surgical techniques for repair and rehabilitation strategies. The document also addresses complications associated with each treatment option and provides insights into associated tendon ruptures.