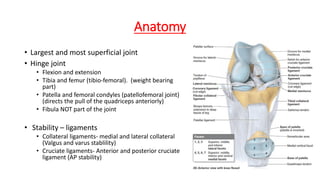
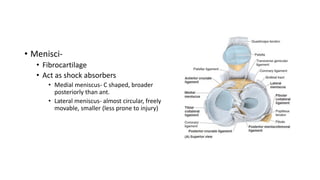
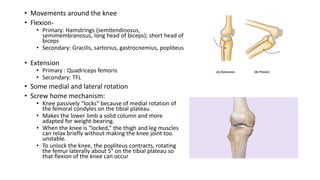
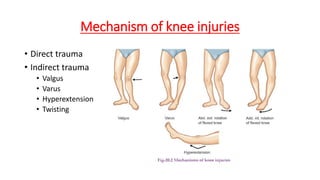
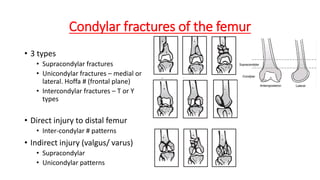
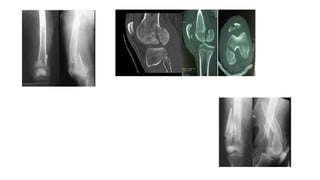
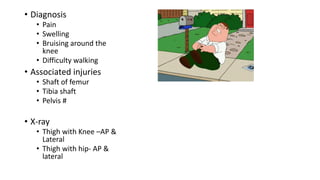
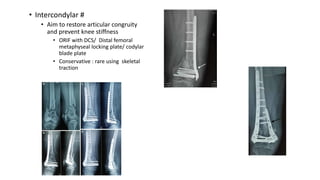
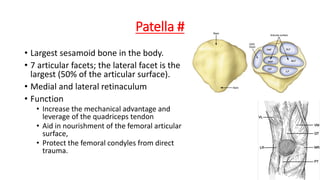
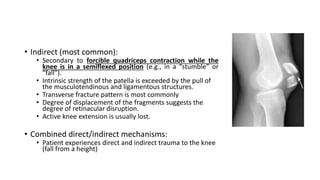
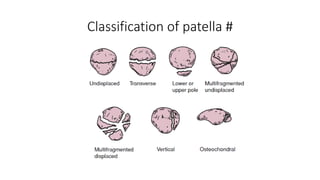
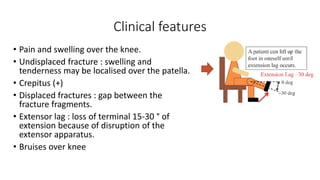
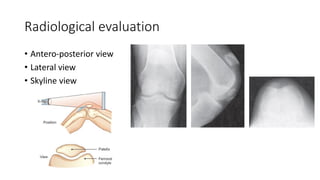
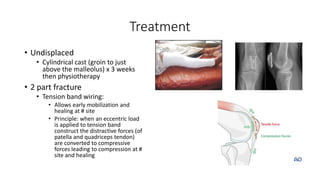
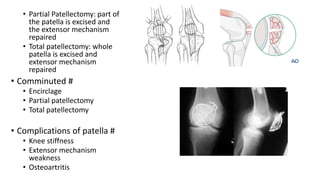
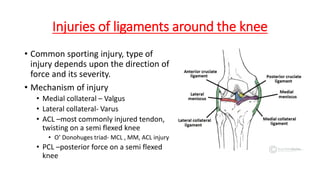
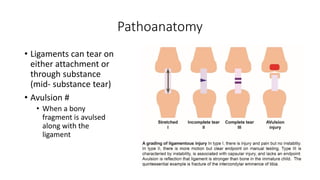
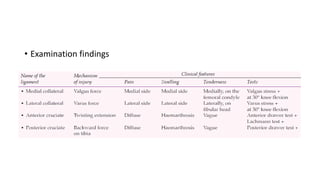
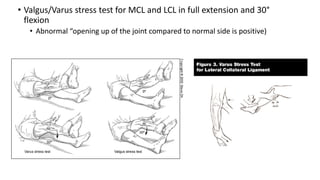
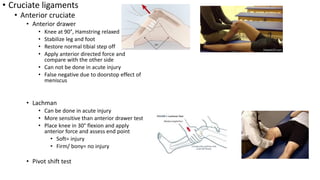
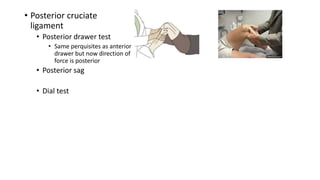
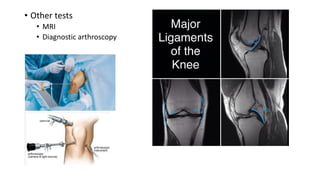
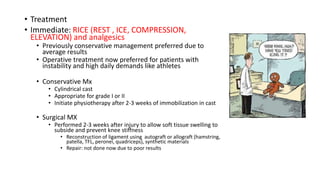
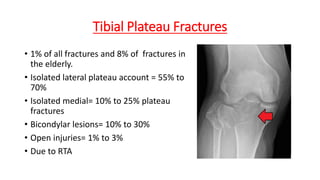
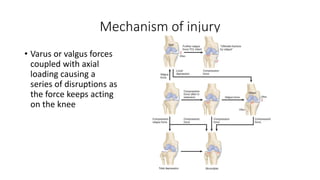
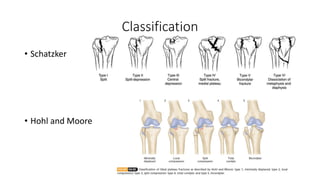
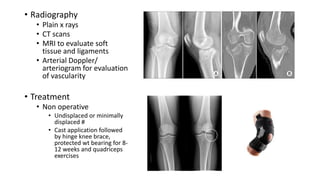
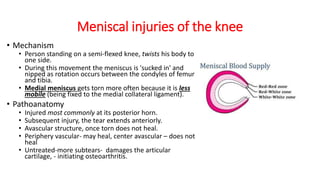
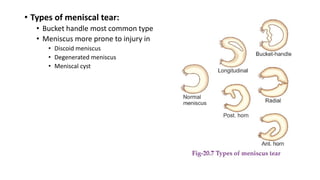
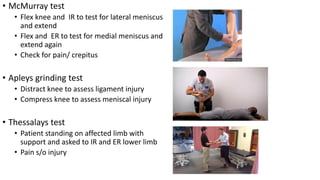
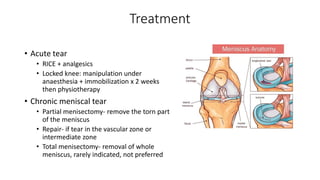
This document provides an overview of common injuries around the knee joint. It describes the anatomy of the knee including bones and ligaments. Common mechanisms of injury are discussed for fractures around the knee like condylar fractures of the femur, patella fractures, and tibial plateau fractures. Injuries to the ligaments including ACL, PCL, MCL and LCL are also summarized. Treatment approaches for many of these injuries including nonsurgical and surgical options are highlighted. Other topics covered include meniscal injuries, knee dislocations, and patella dislocations. Complications of various knee injuries are also mentioned.