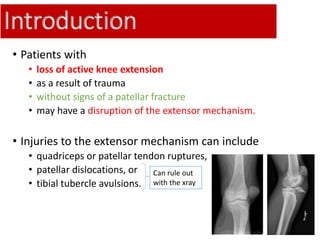
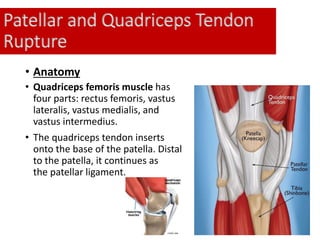
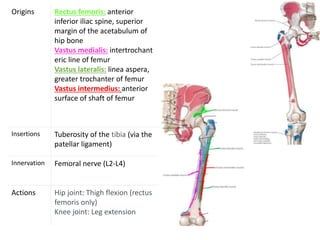
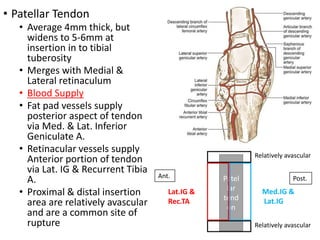
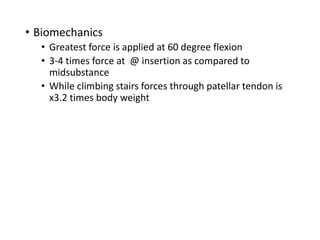
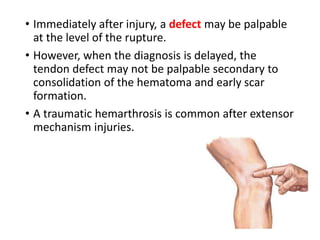
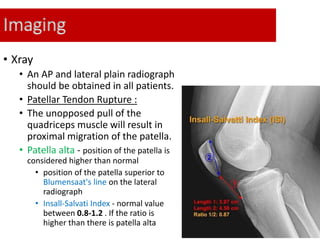
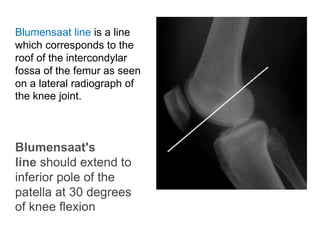
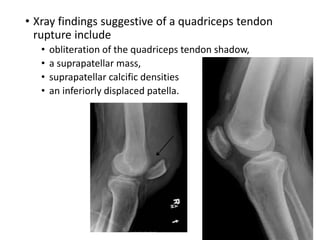
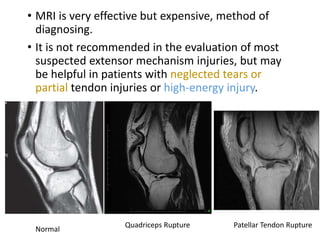
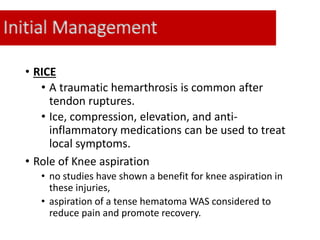
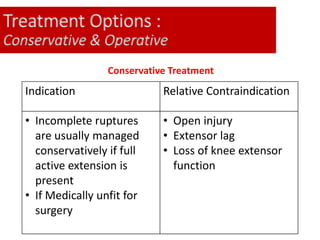
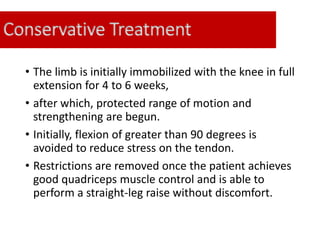
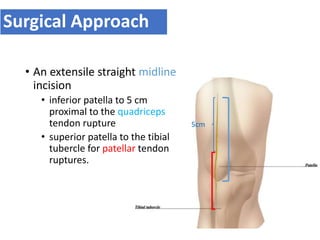
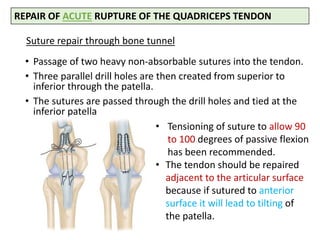
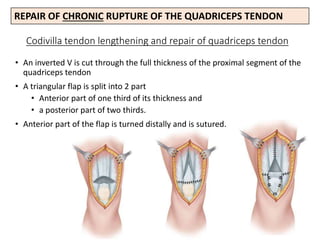
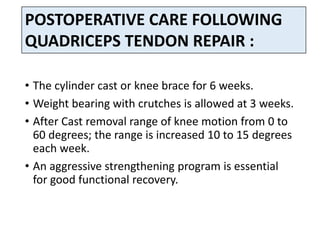
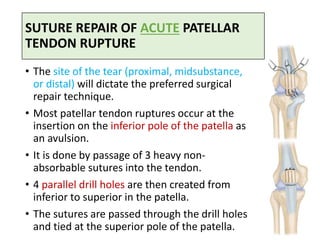
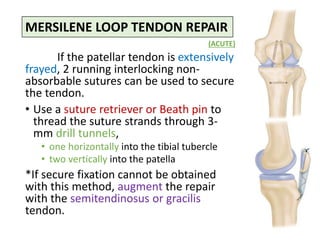
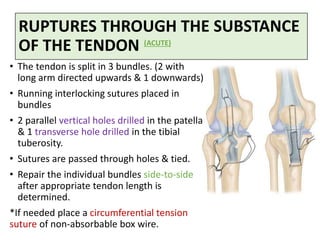
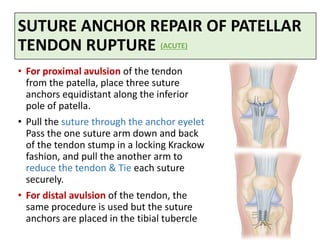
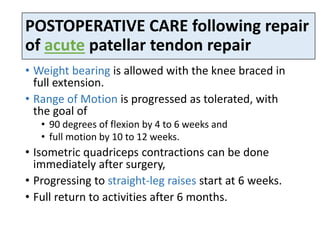
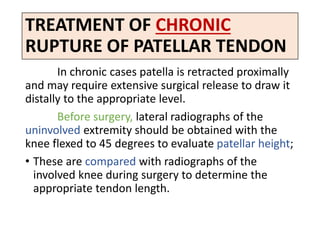
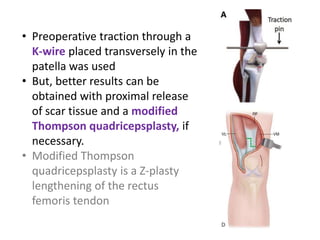
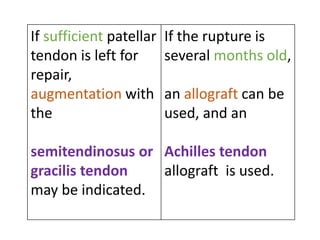
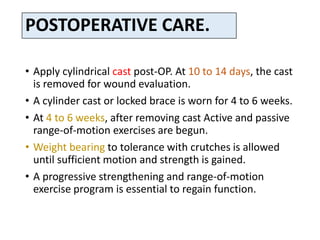
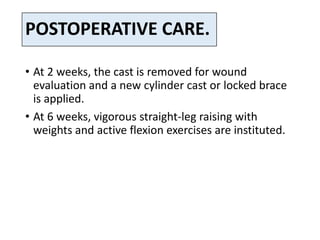
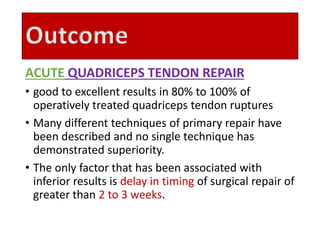
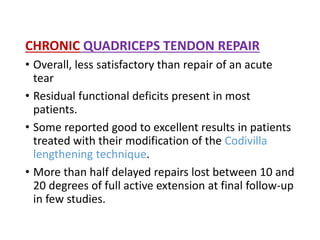
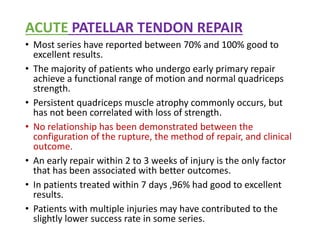
This document discusses extensor mechanism injuries in the knee, focusing on quadriceps and patellar tendon ruptures, including their anatomy, mechanisms of injury, and clinical presentation based on patient demographics. It details management strategies for both conservative and operative treatments, emphasizing the importance of timely surgical intervention for better outcomes. Imaging techniques such as X-rays, ultrasound, and MRI are also outlined, along with the post-operative care and rehabilitation protocols for recovery.