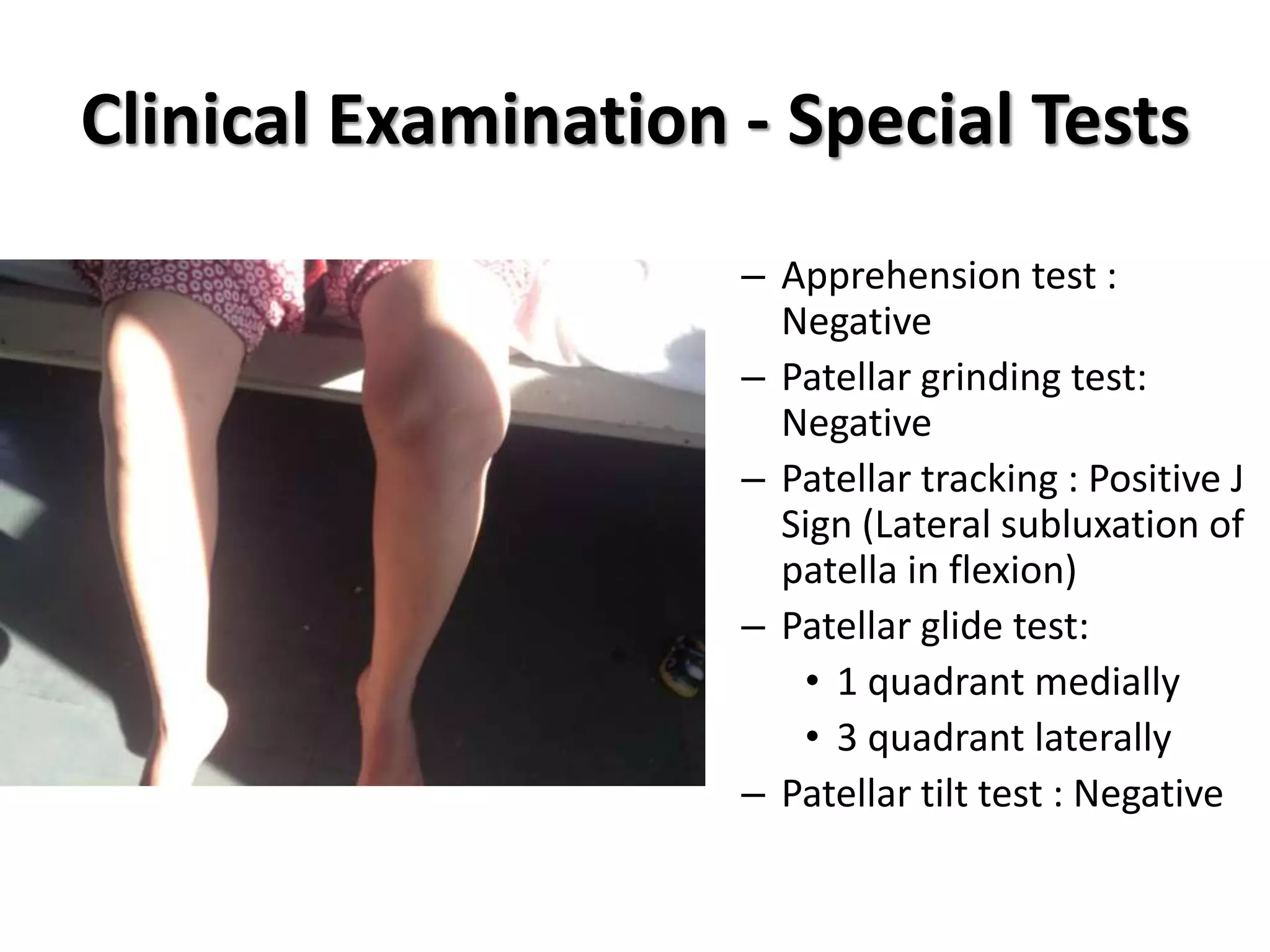
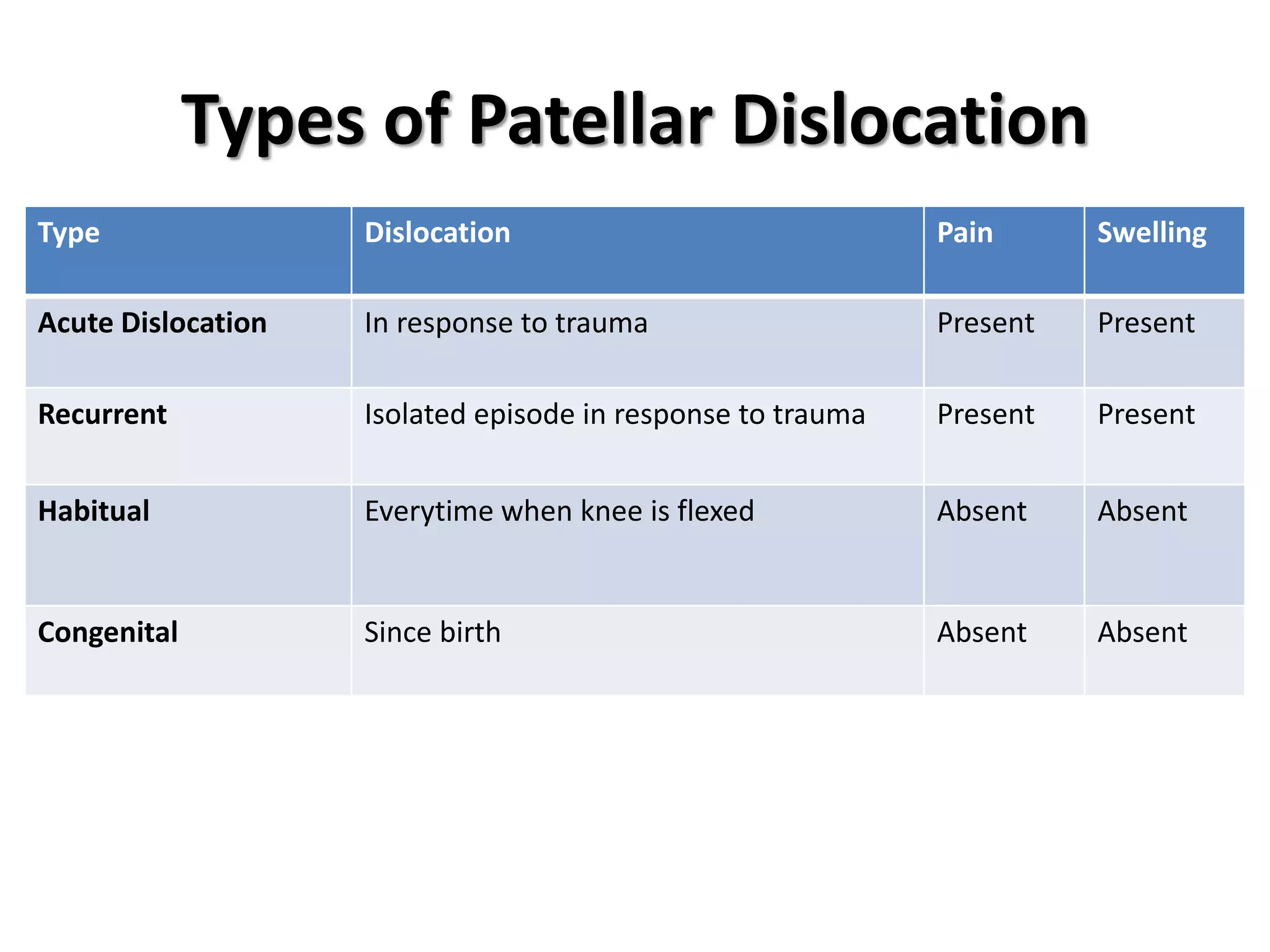
This case report describes a 21-year old female patient with a 10-year history of habitual left patellar dislocation. Examination found lateral subluxation of the patella in flexion and reduced range of motion. X-rays showed patella baja on the left side and lateral dislocation of the patella. The patient underwent a proximal and distal soft tissue realignment procedure involving lateral release, medial reinforcement, and partial medialization of the patellar tendon. Post-operatively, the patella was centrally located with improved range of motion and stability. Habitual patellar dislocation is rare in adults and can be treated with soft tissue realignment surgery to reinforce the medial structures and release tight