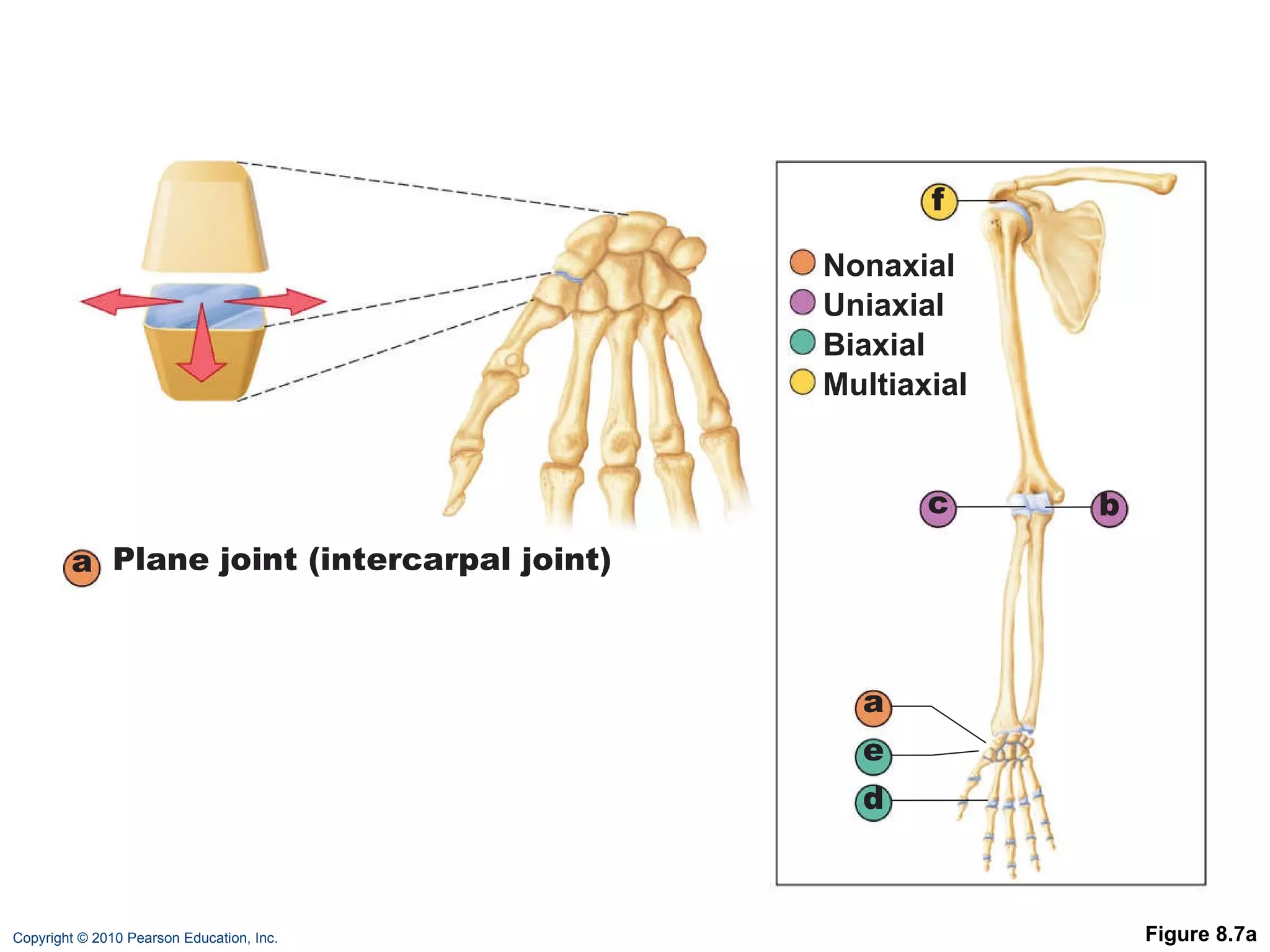
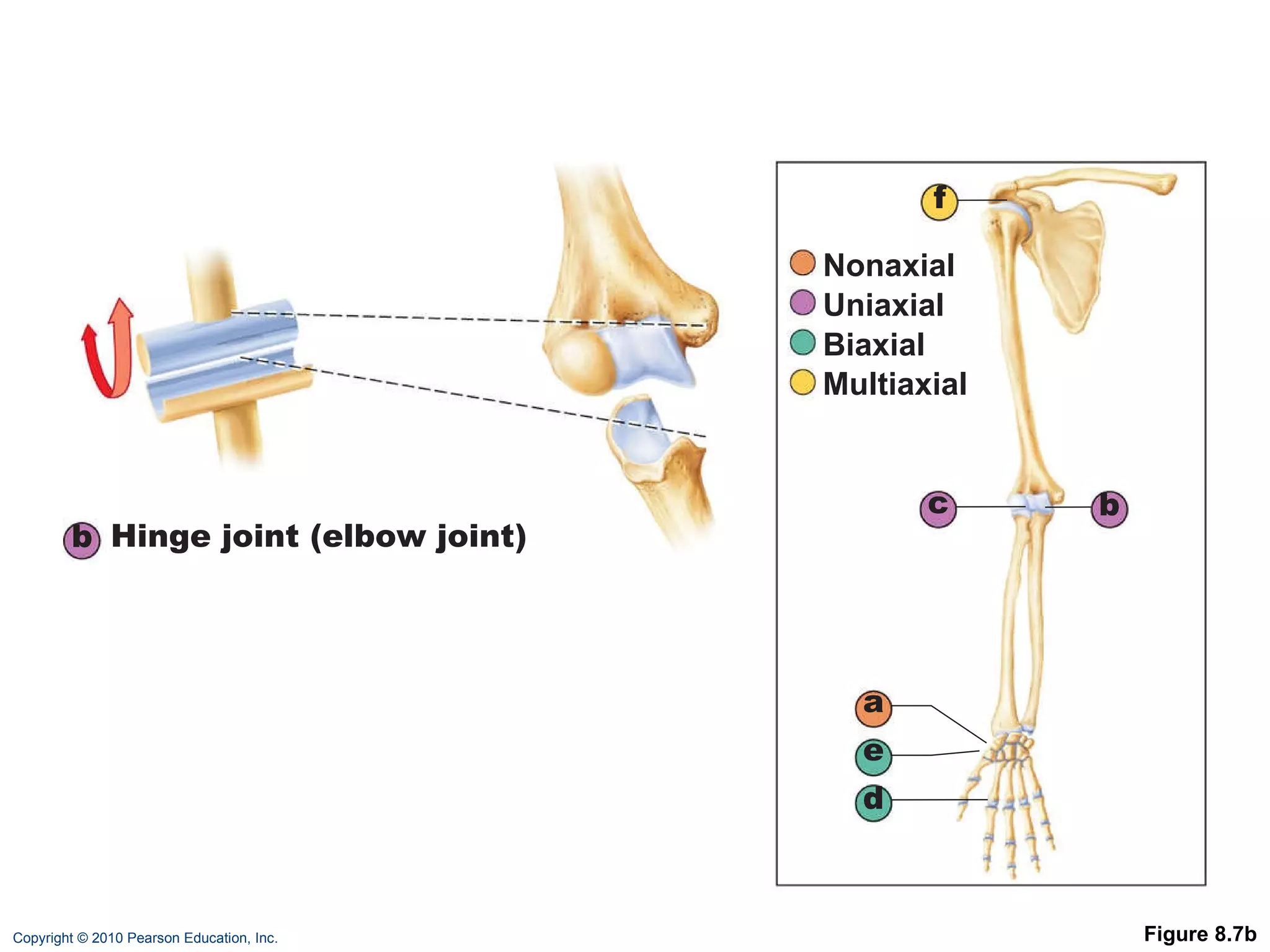
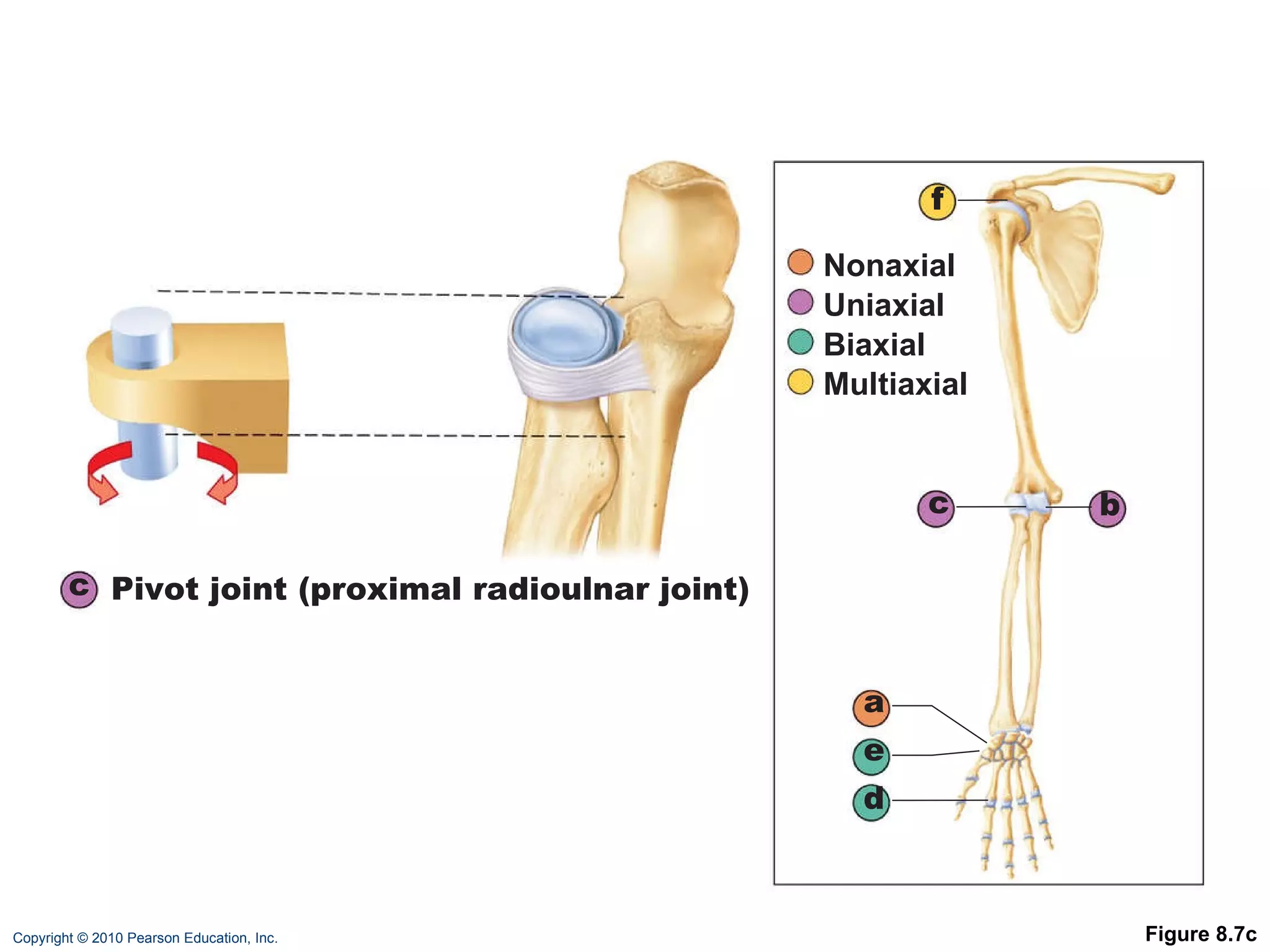
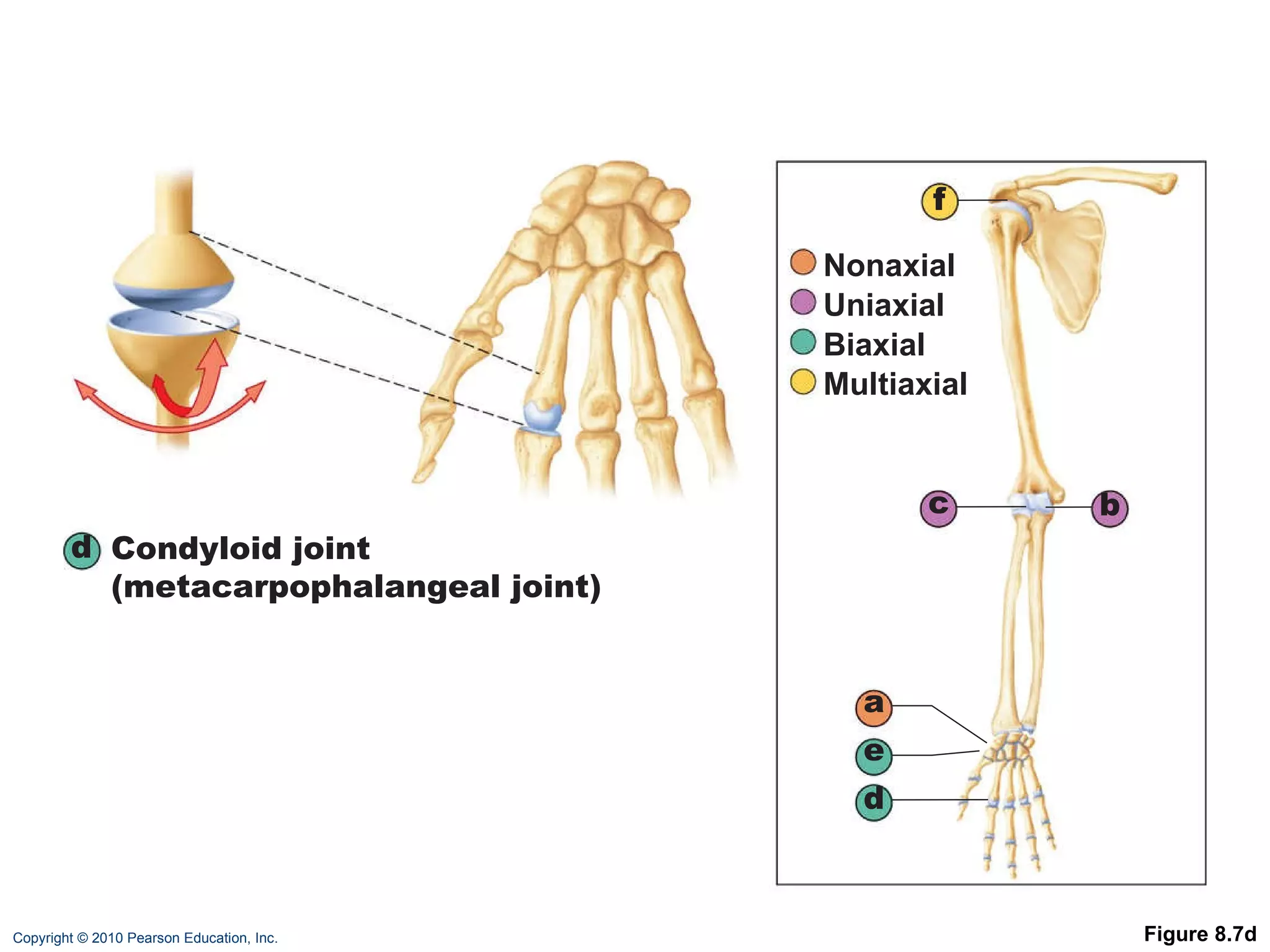
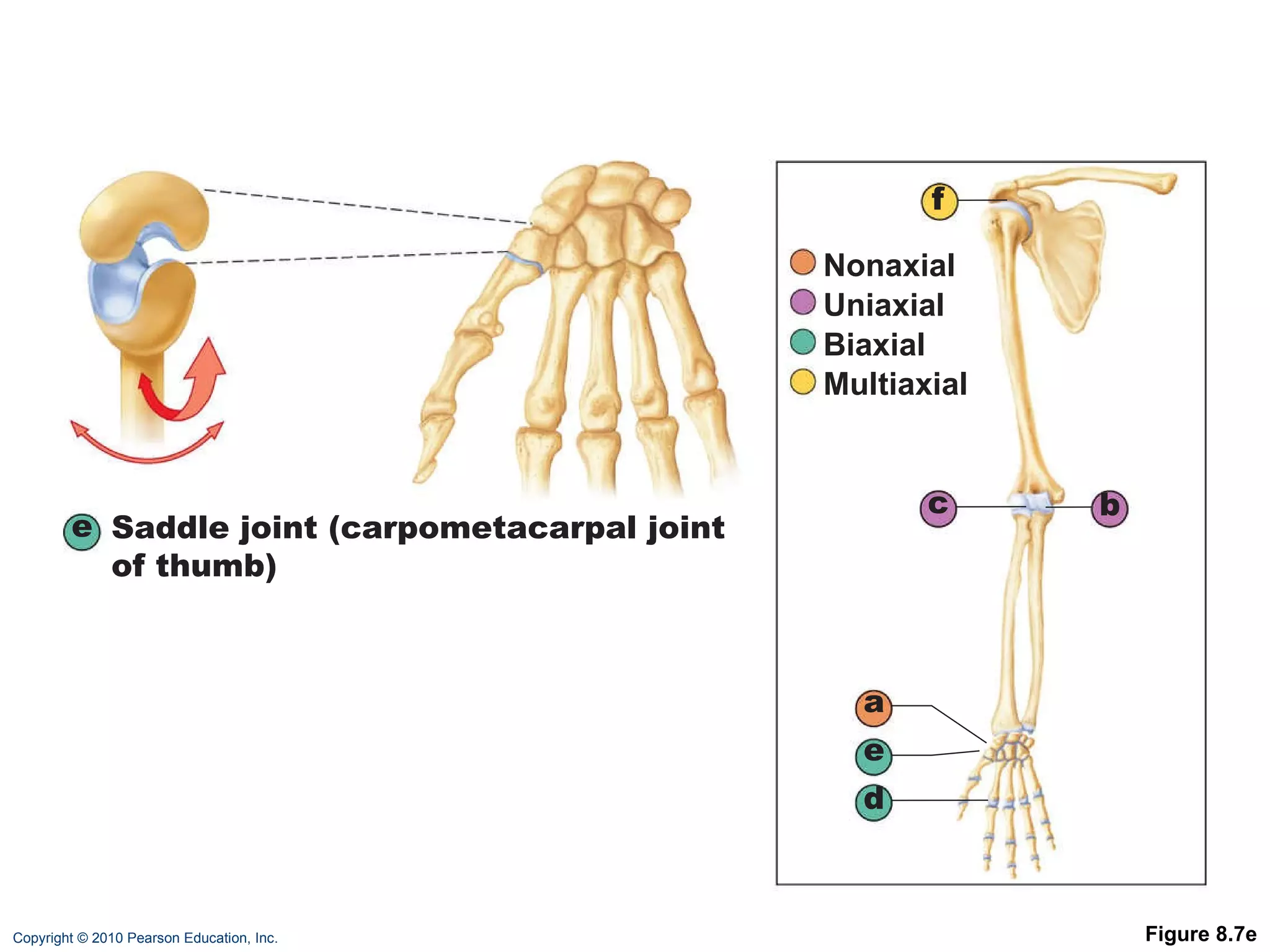
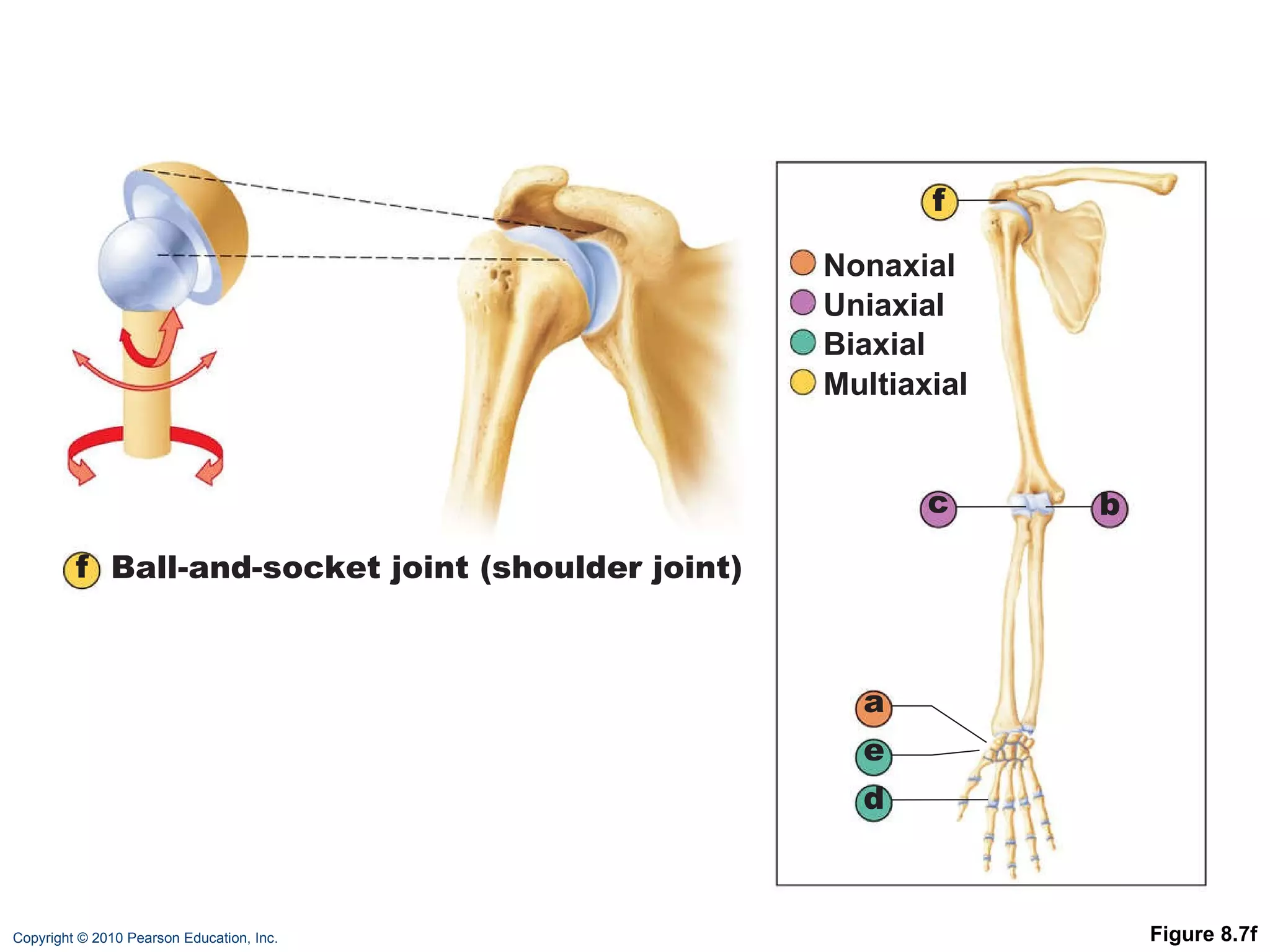
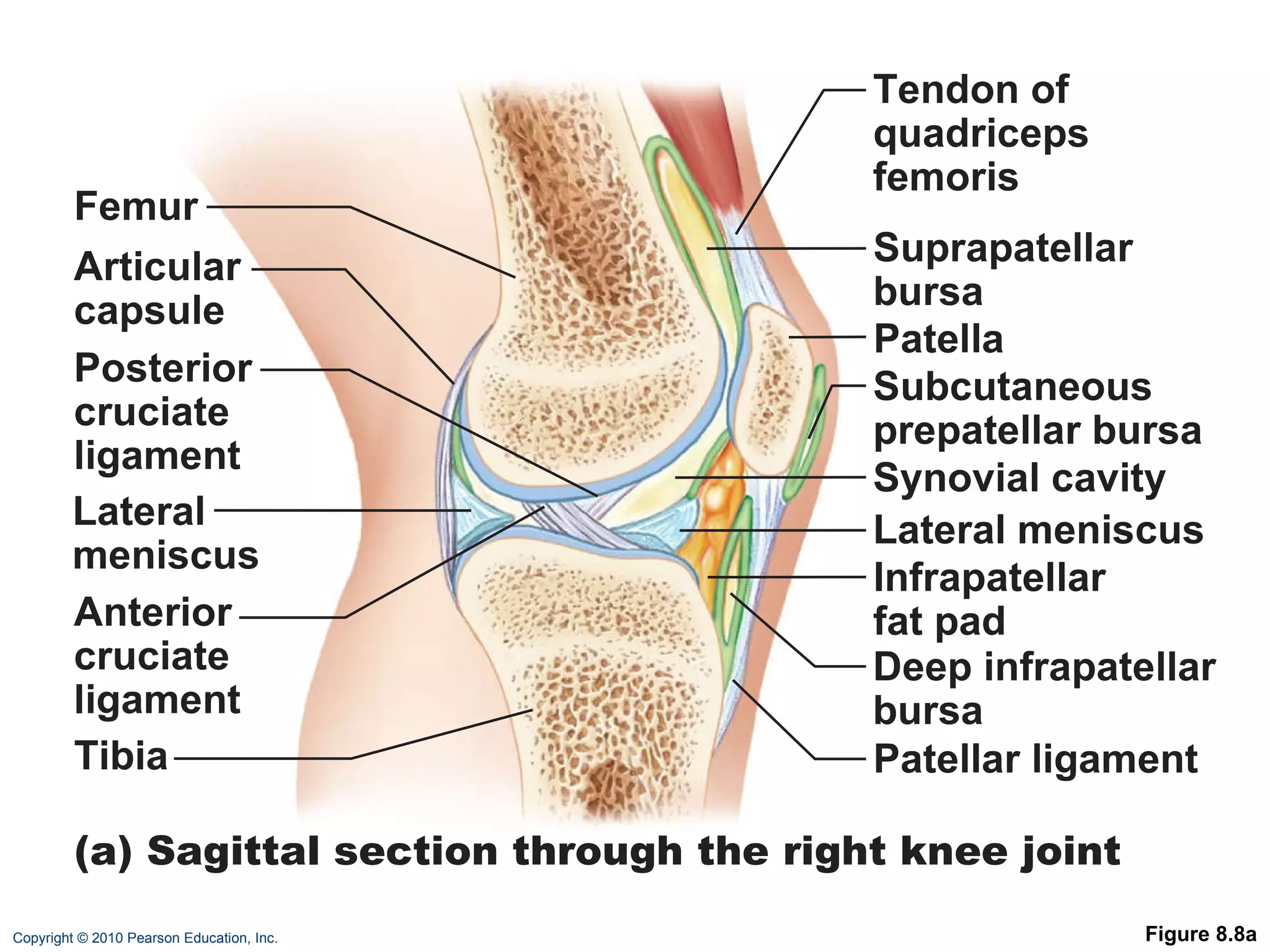
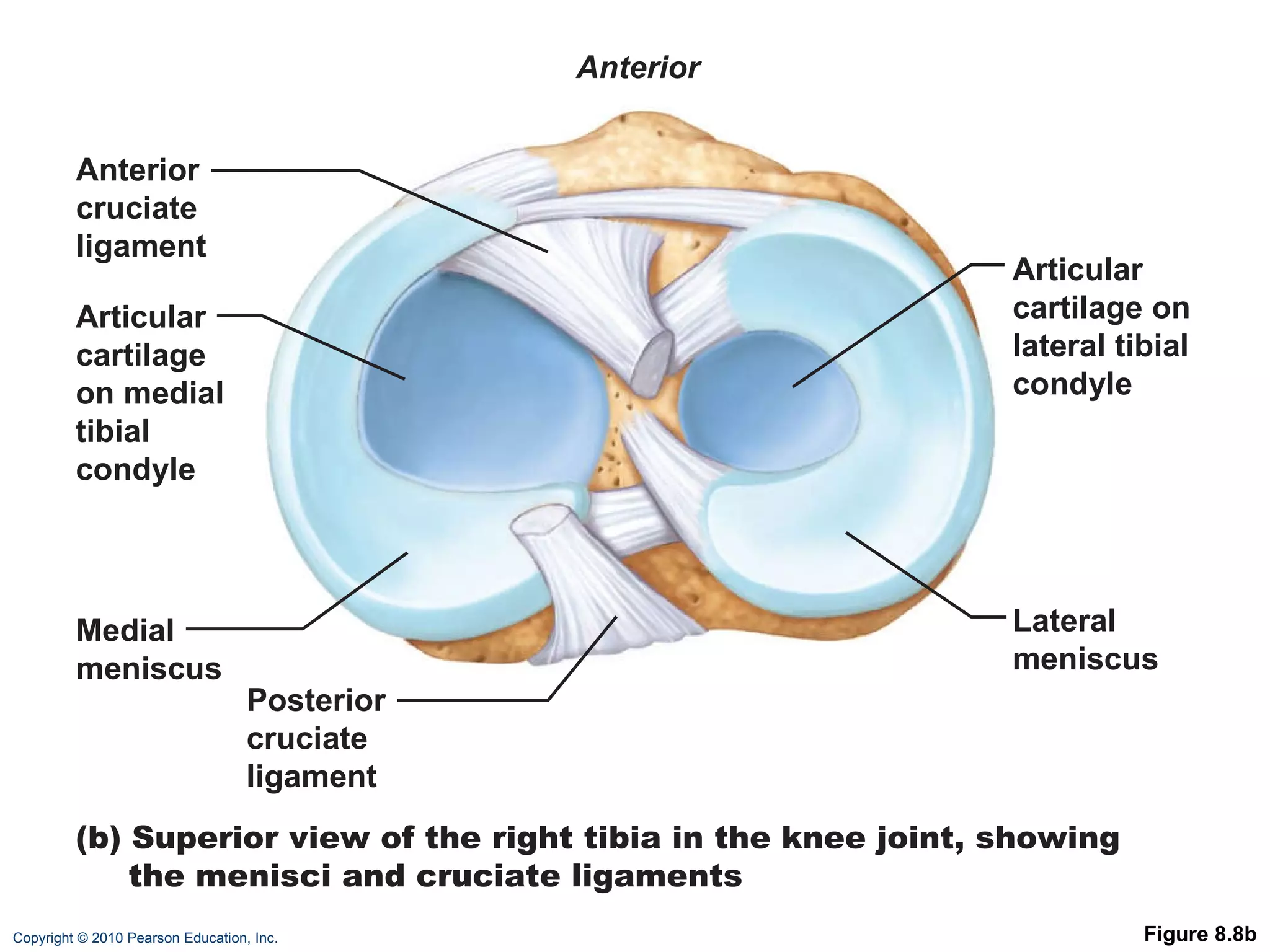
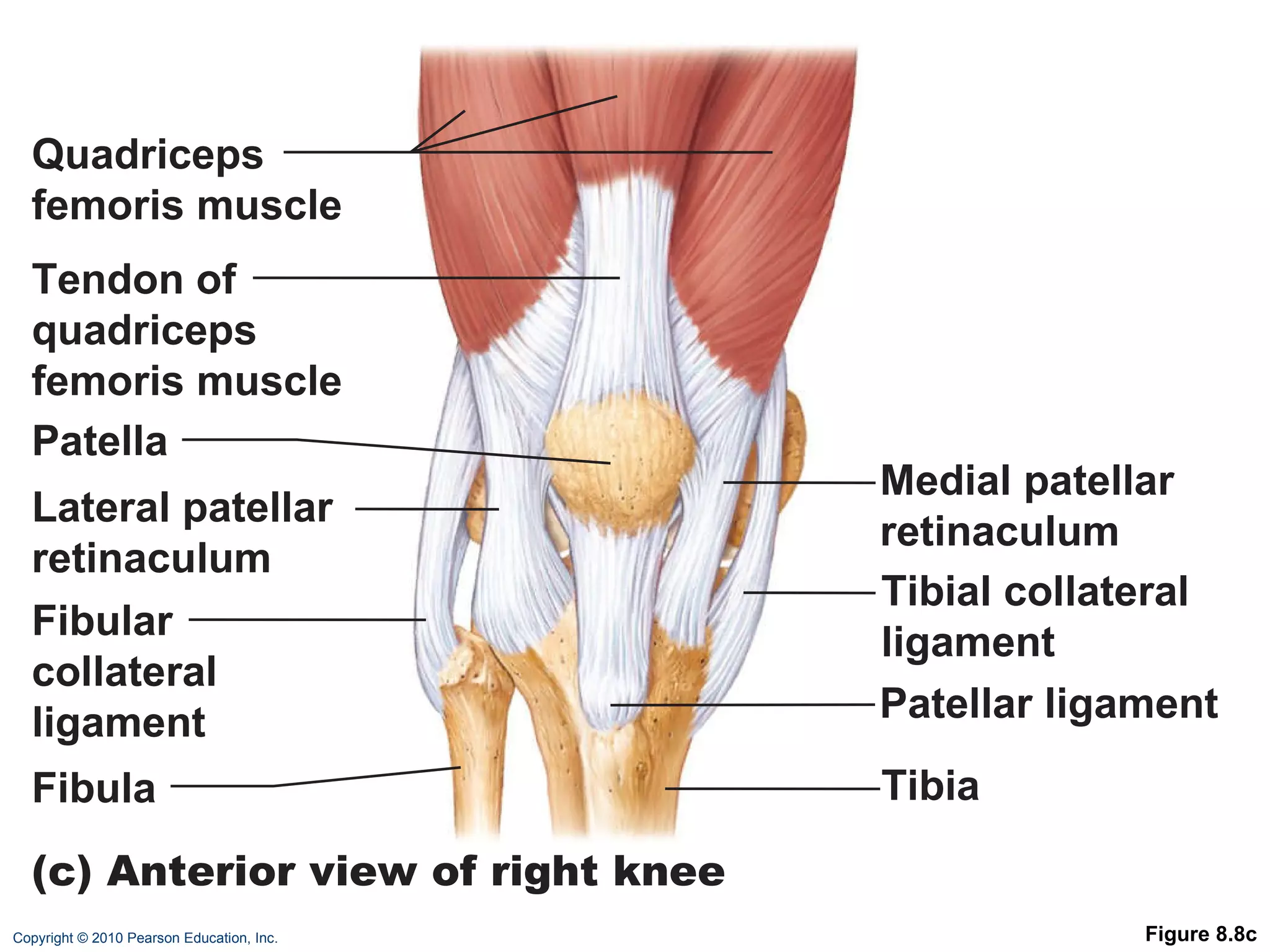
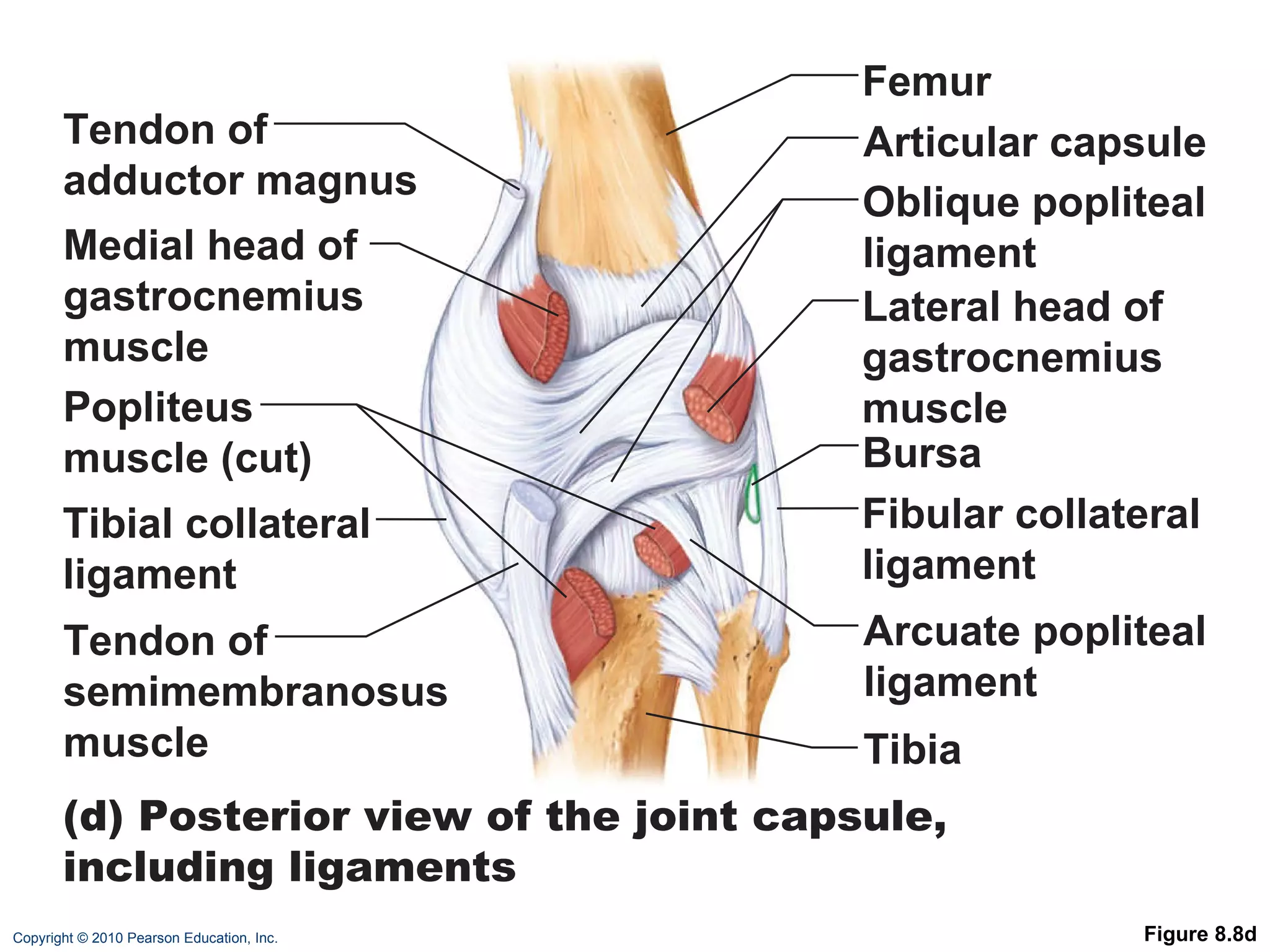
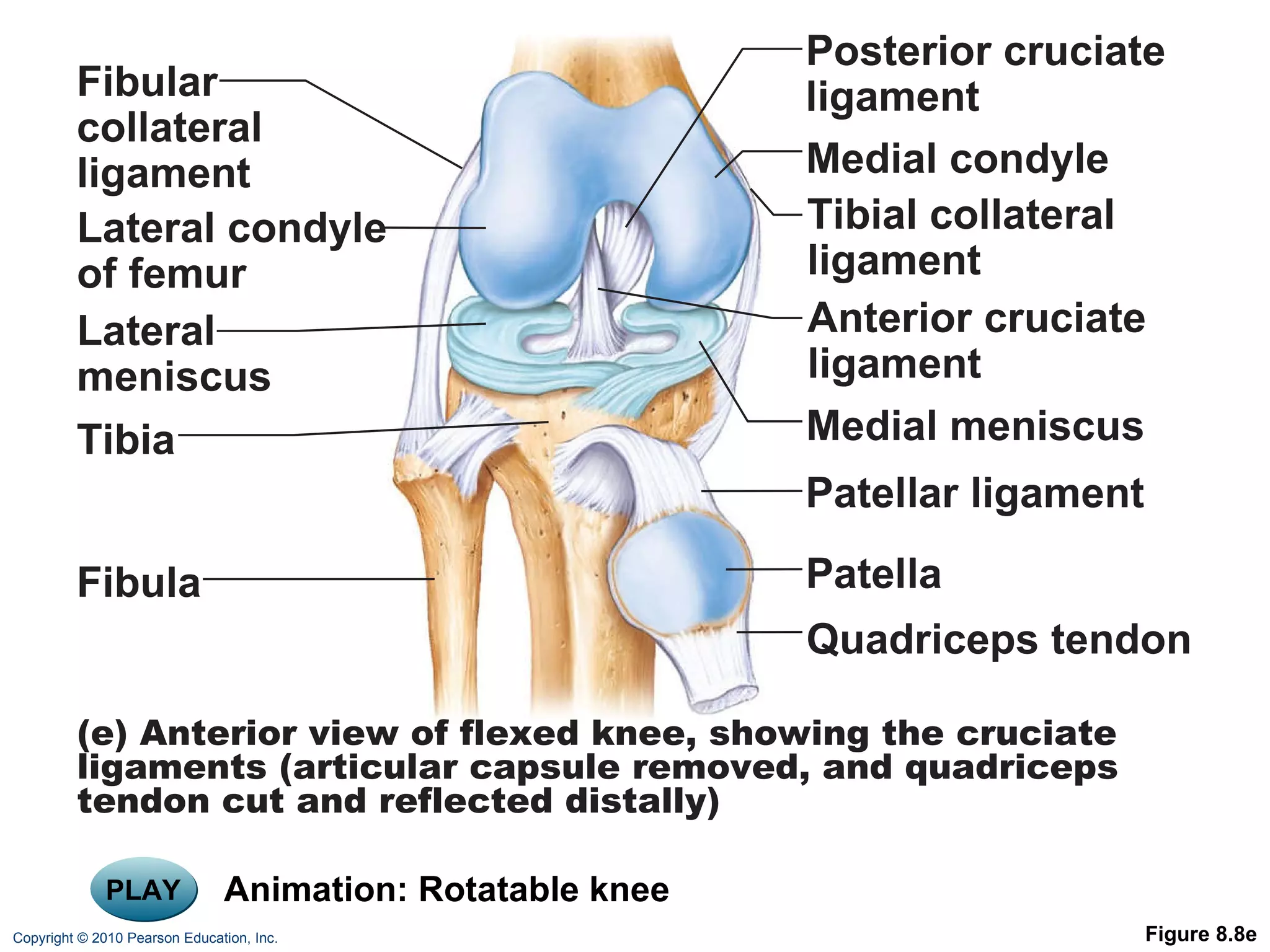
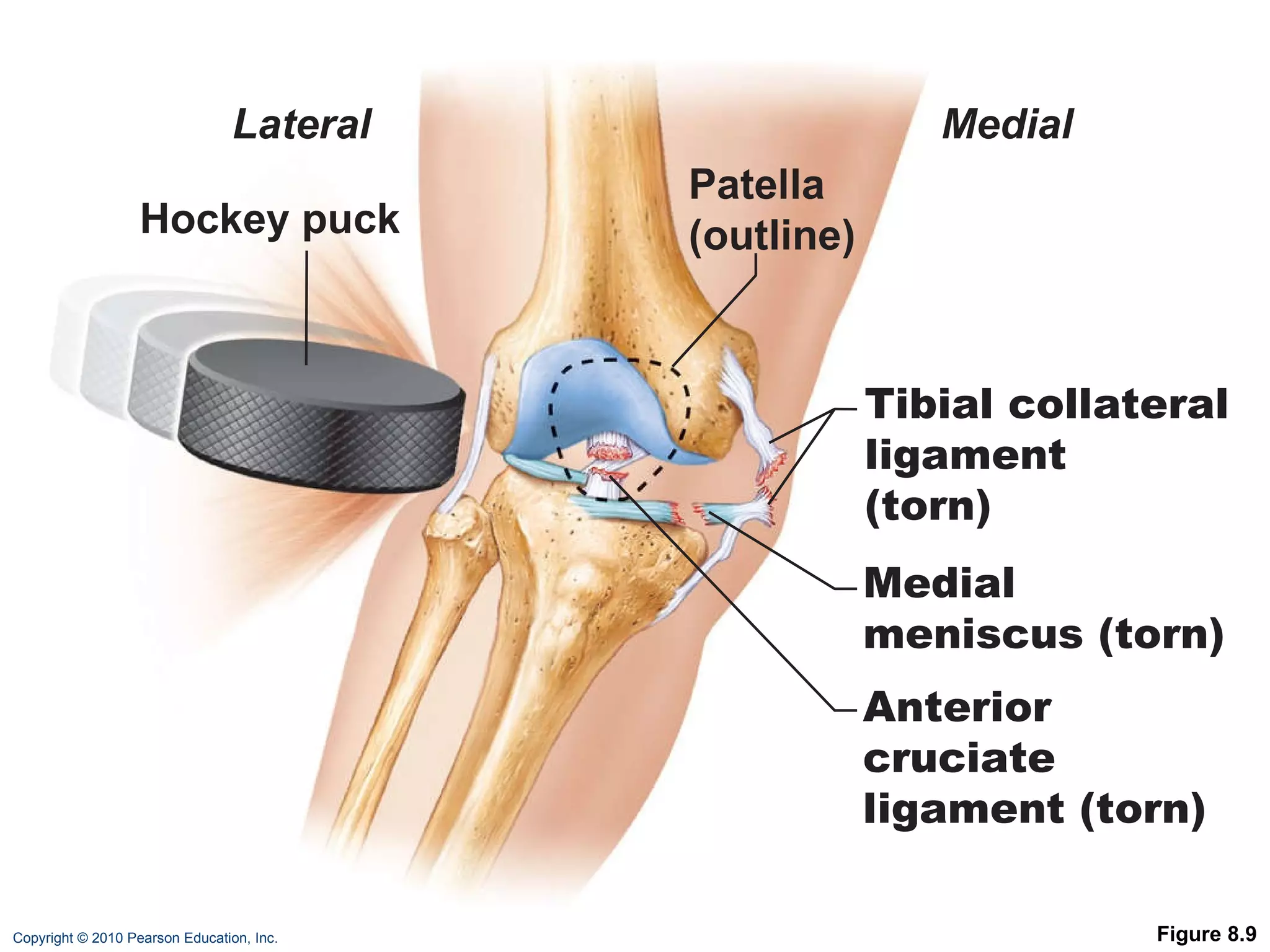
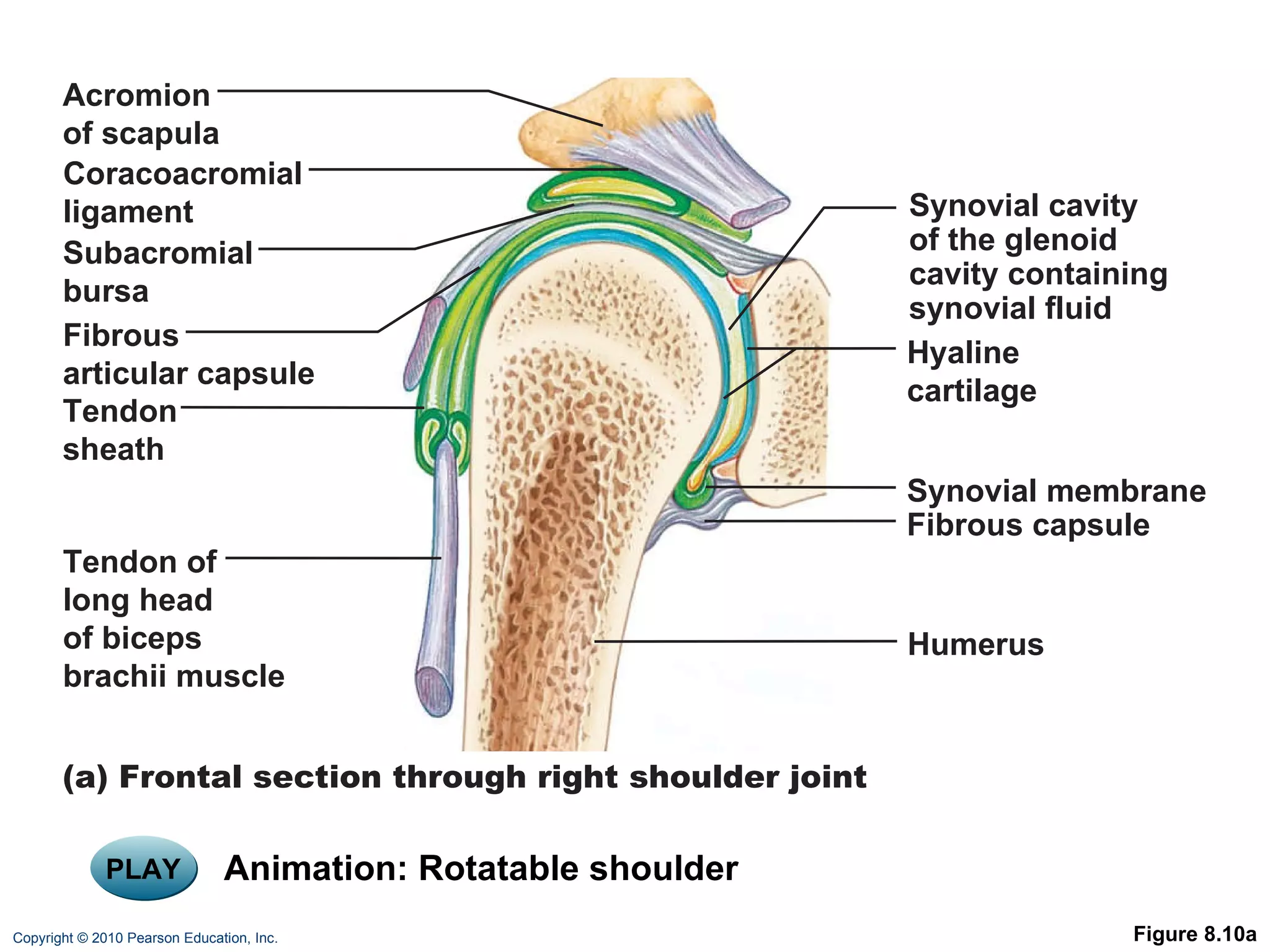
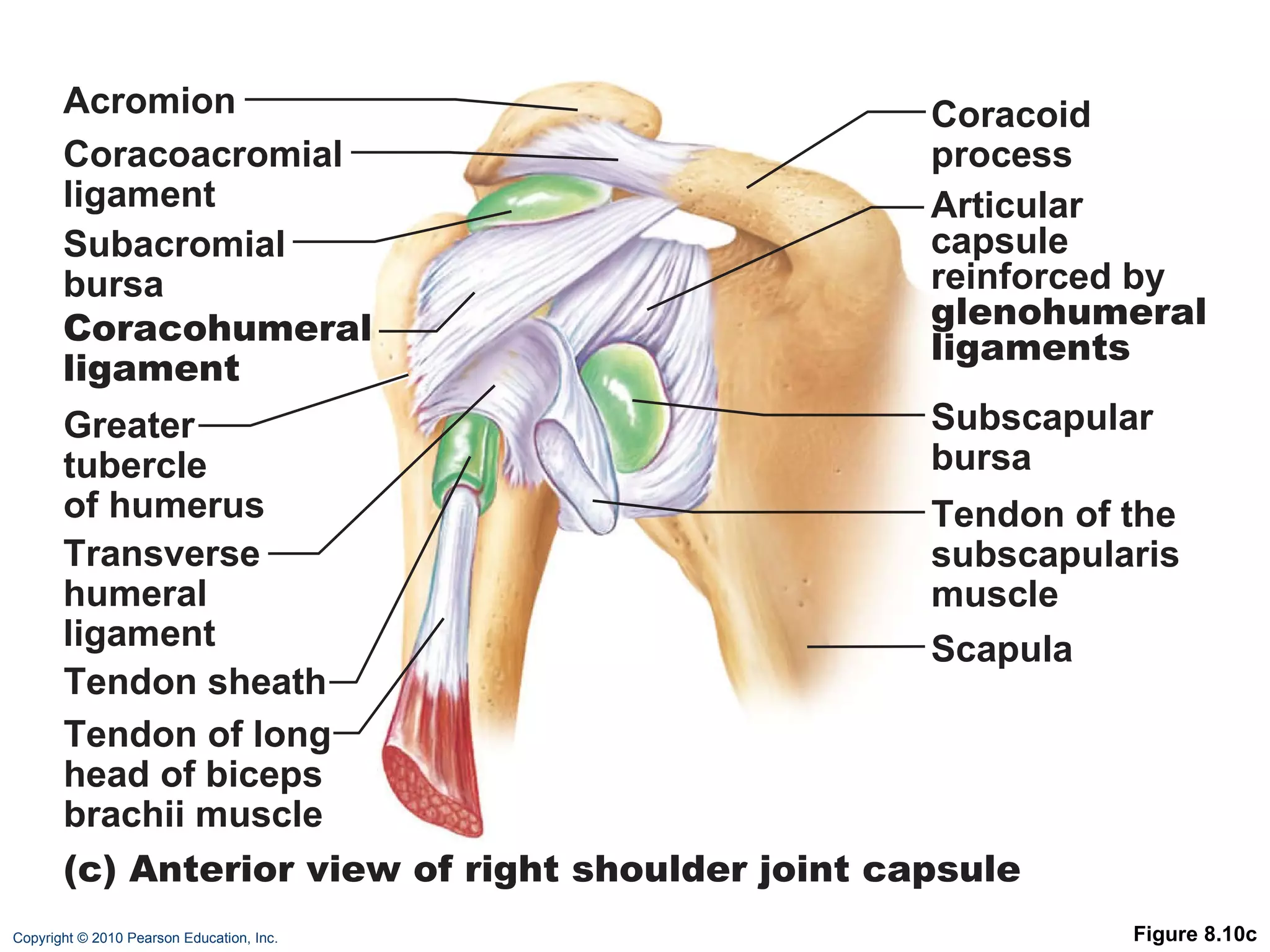
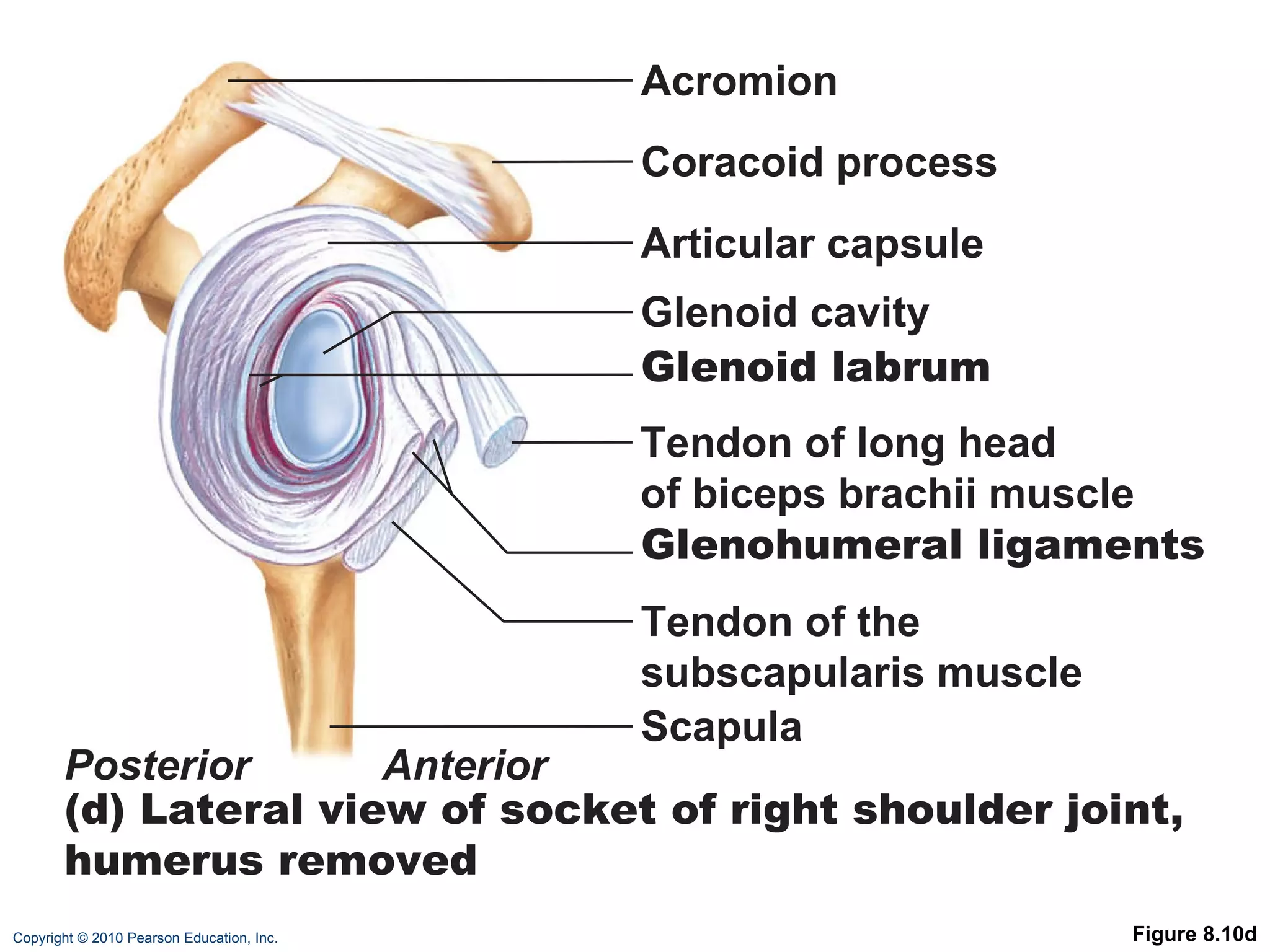
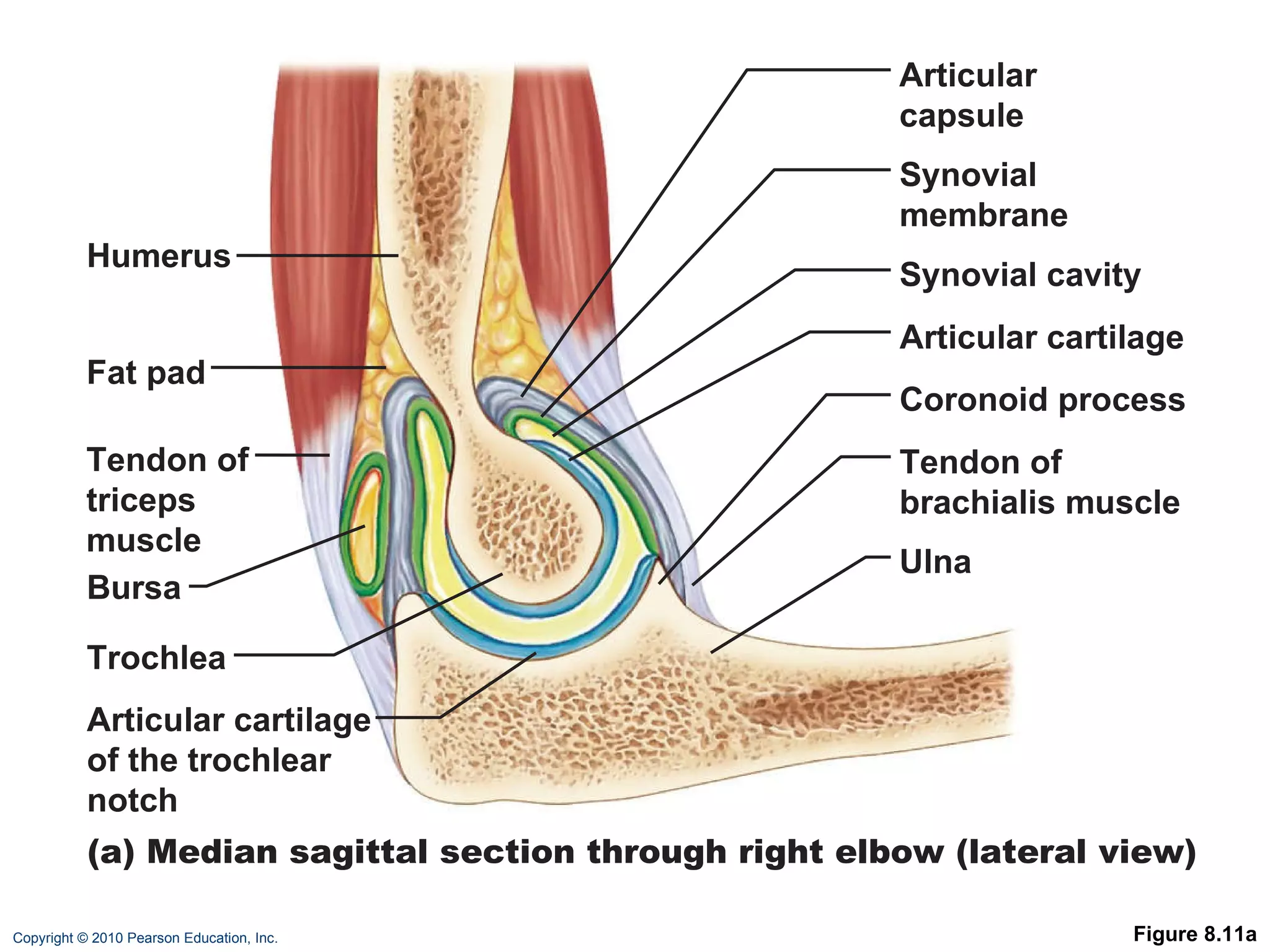
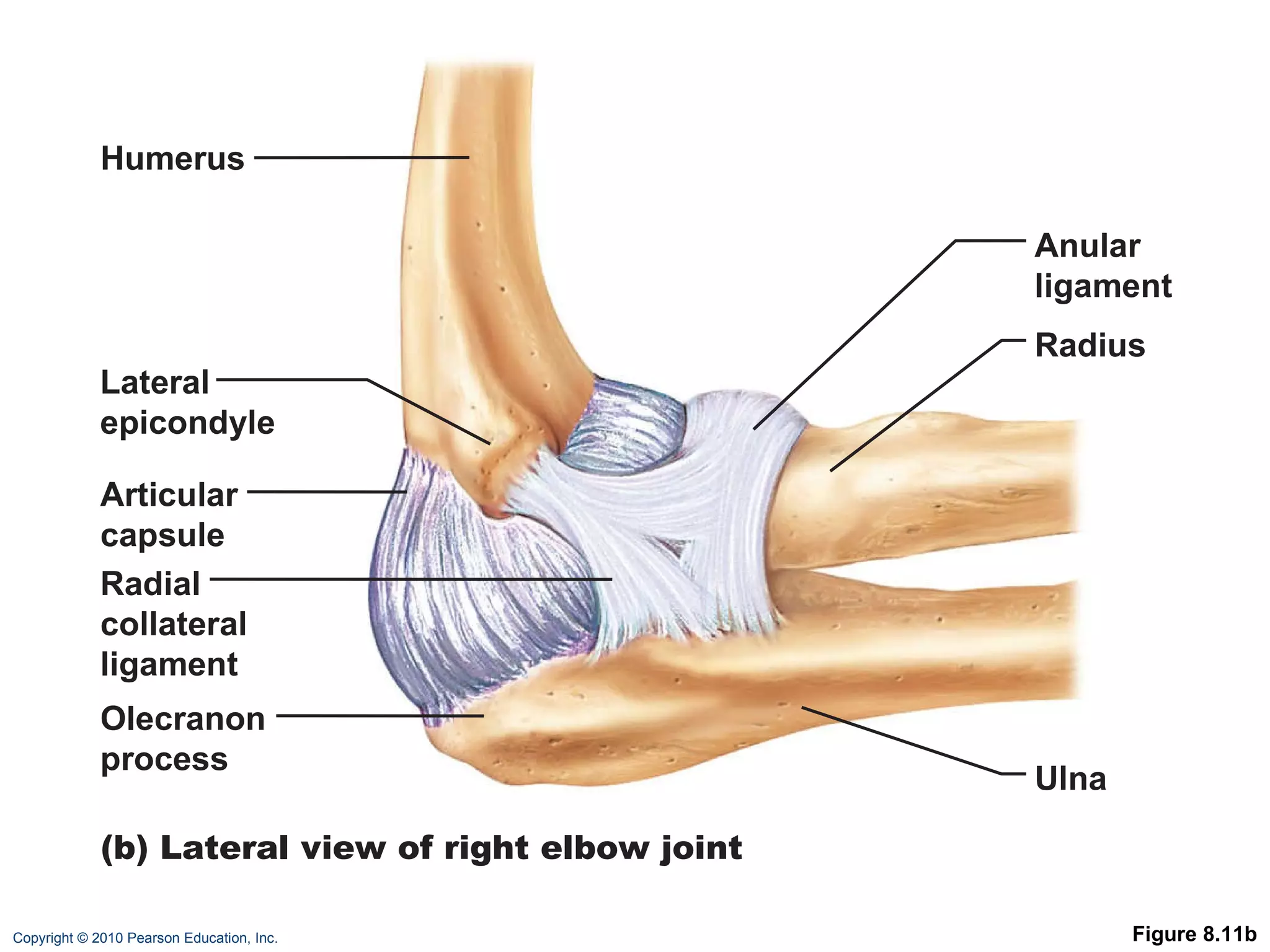
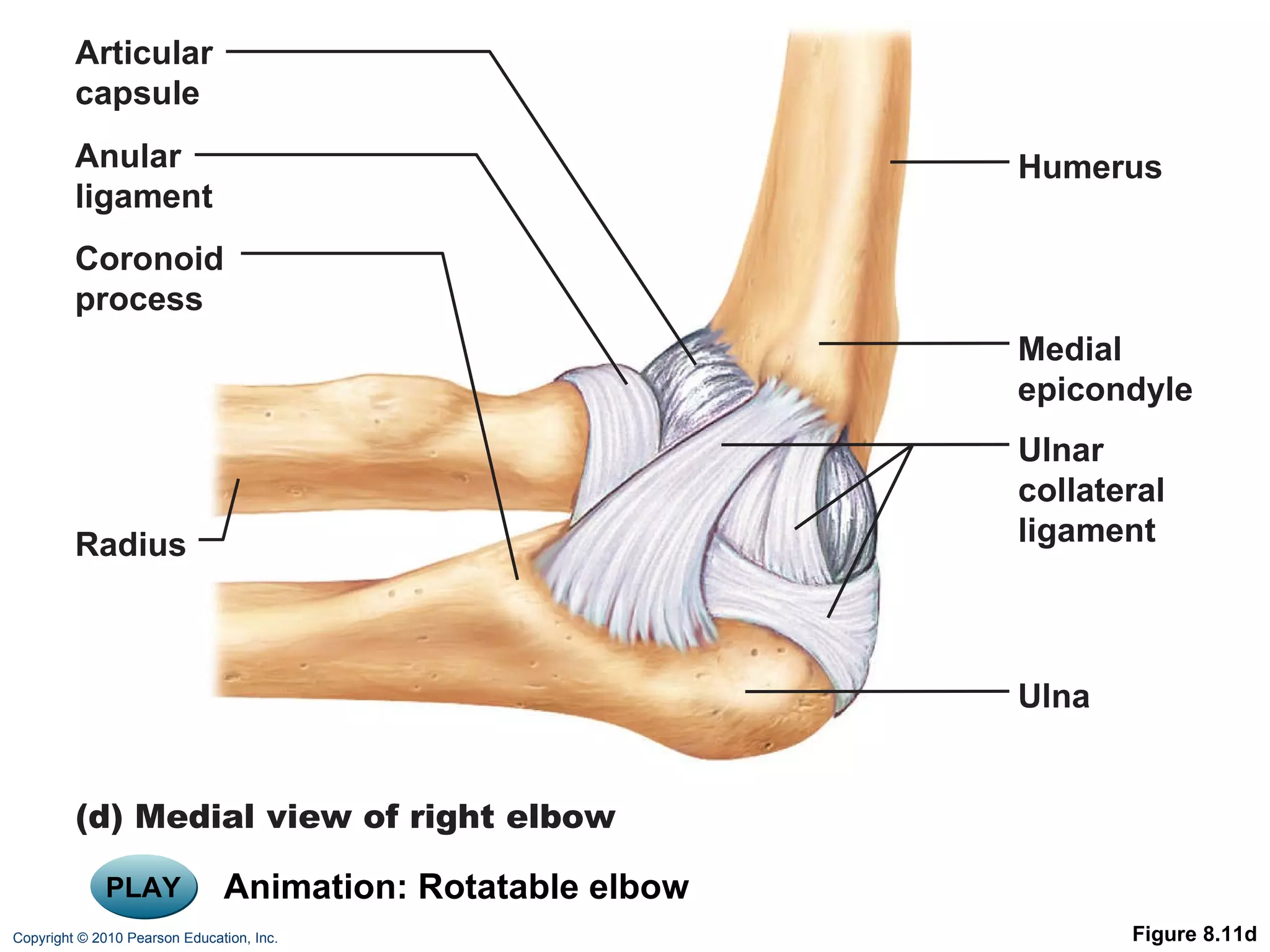
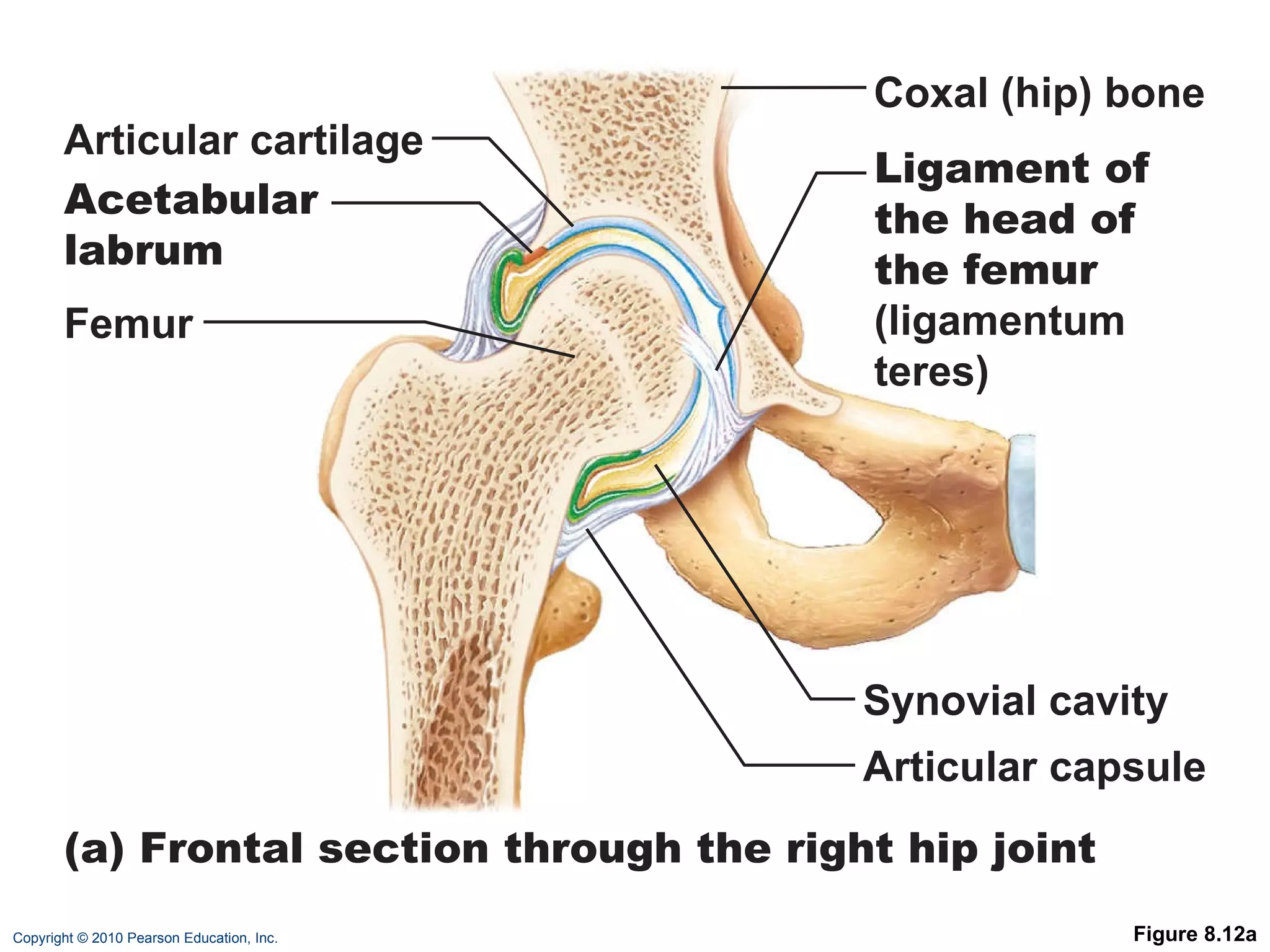
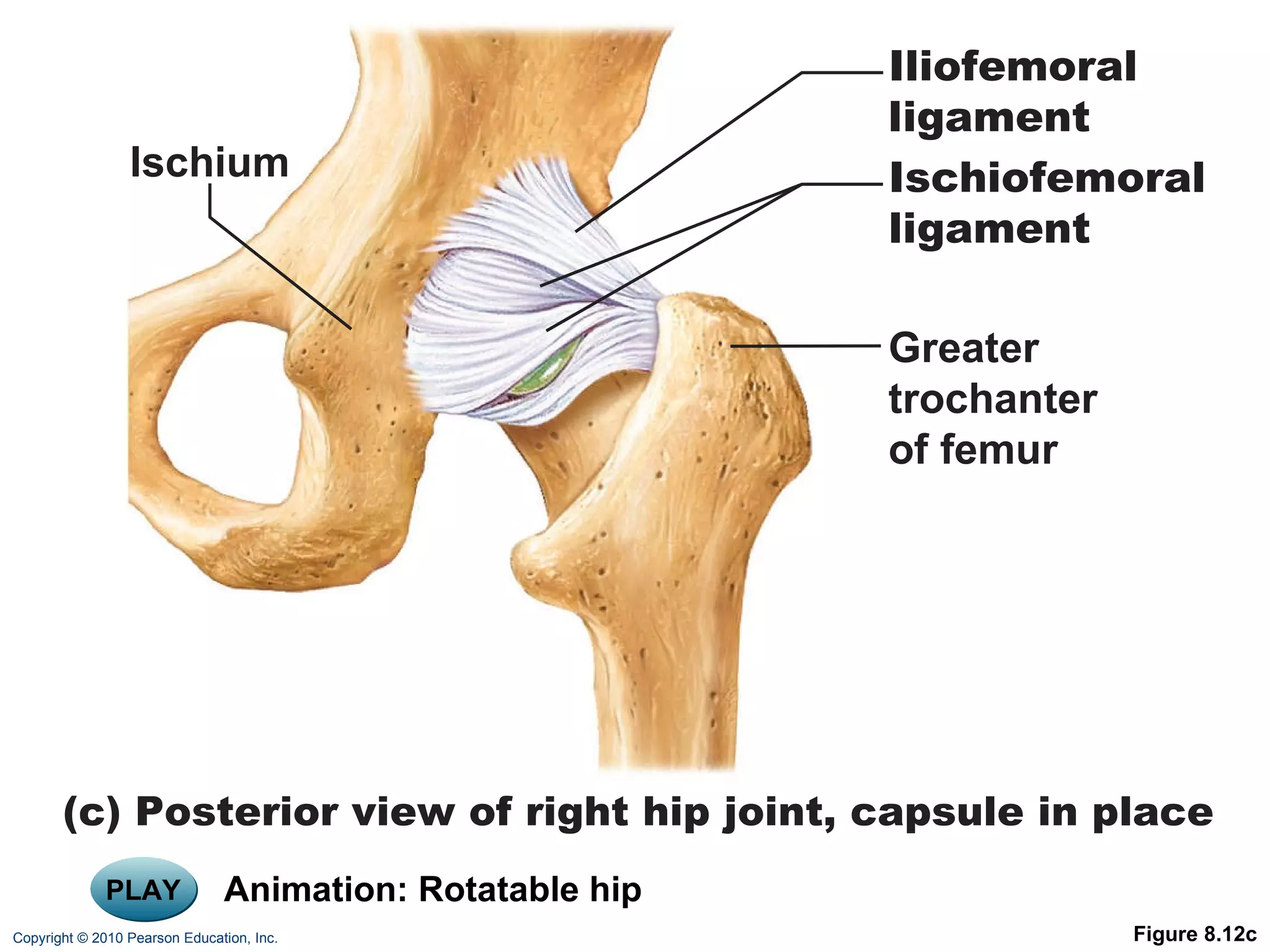
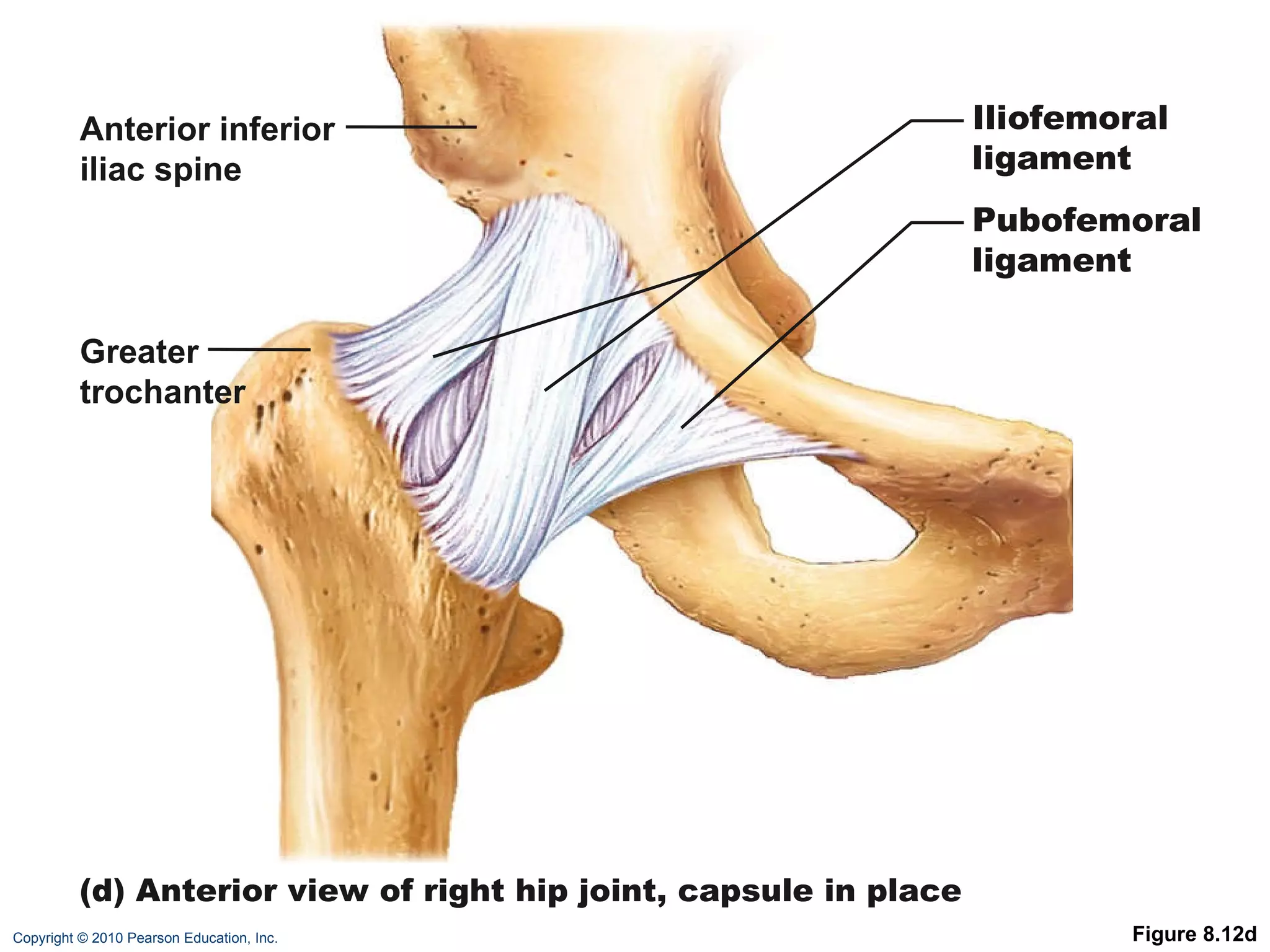
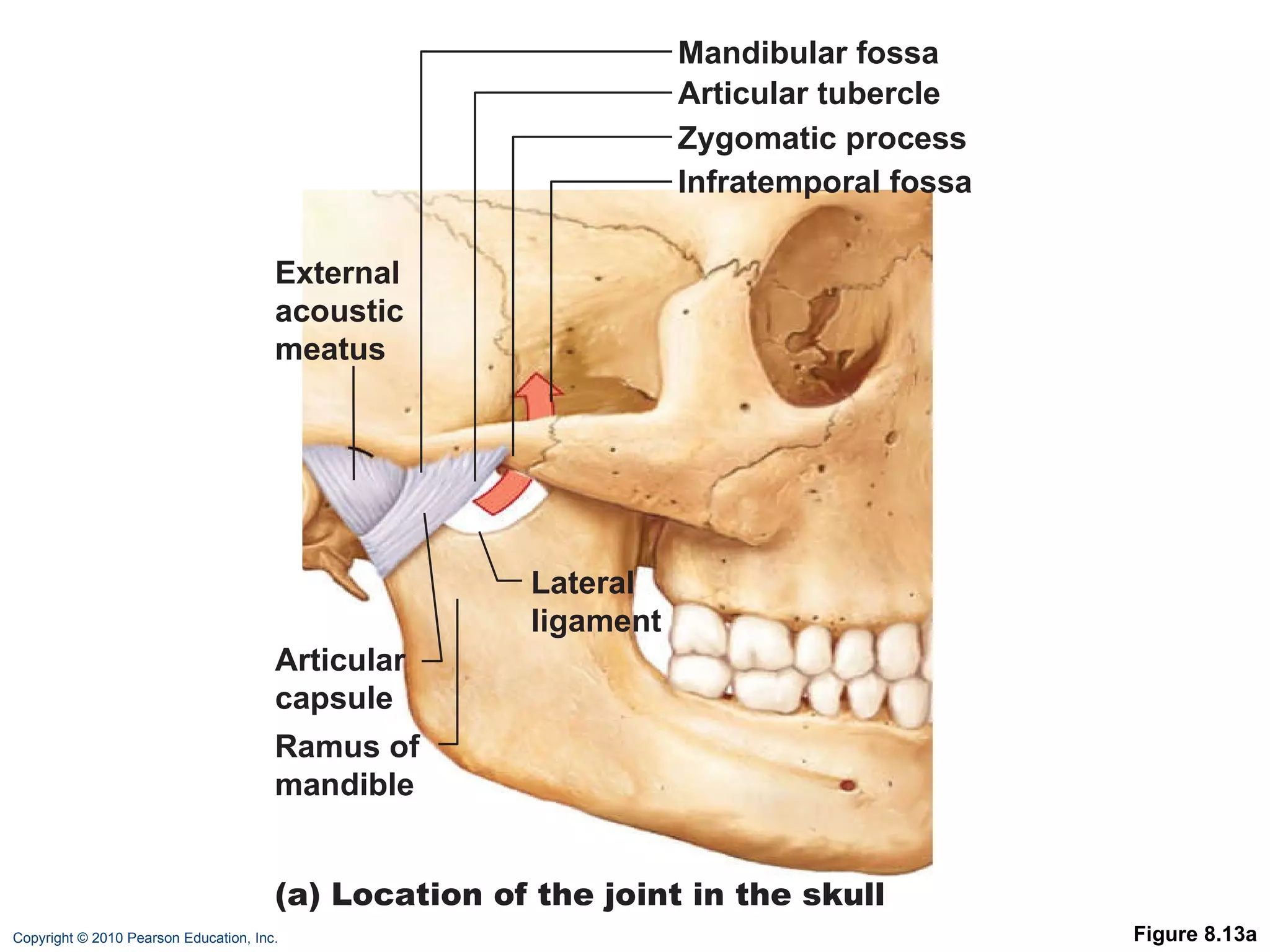
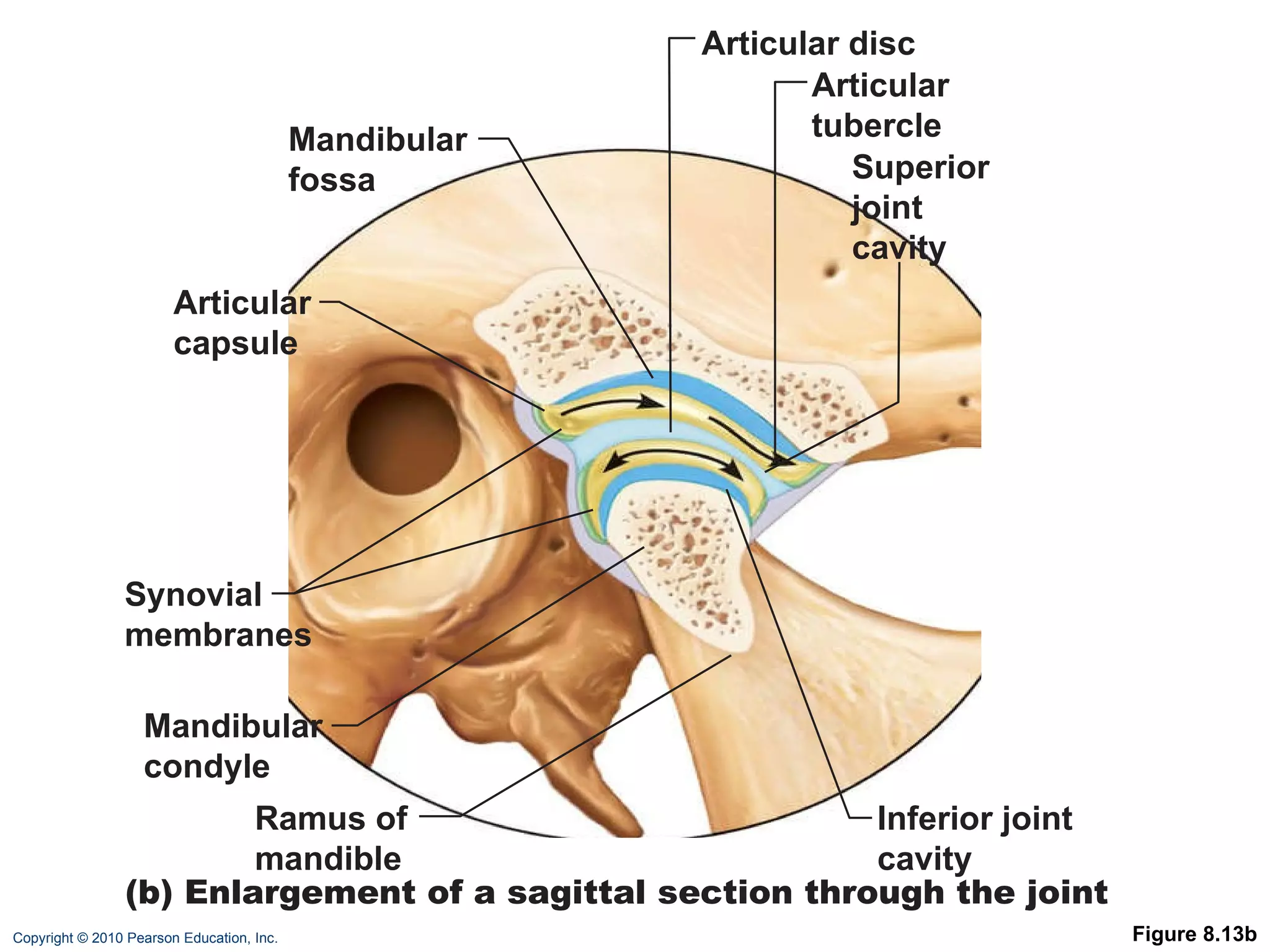
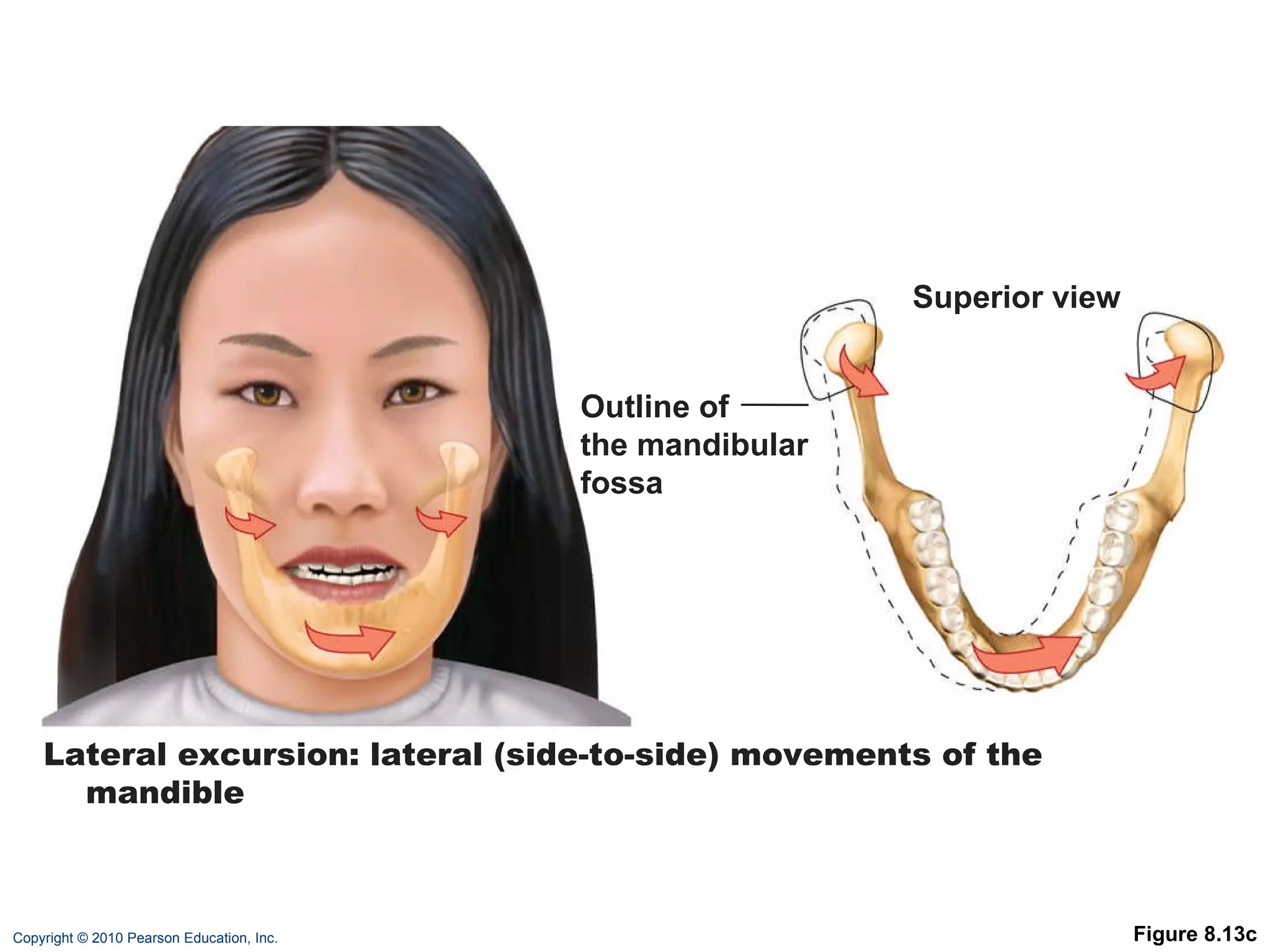
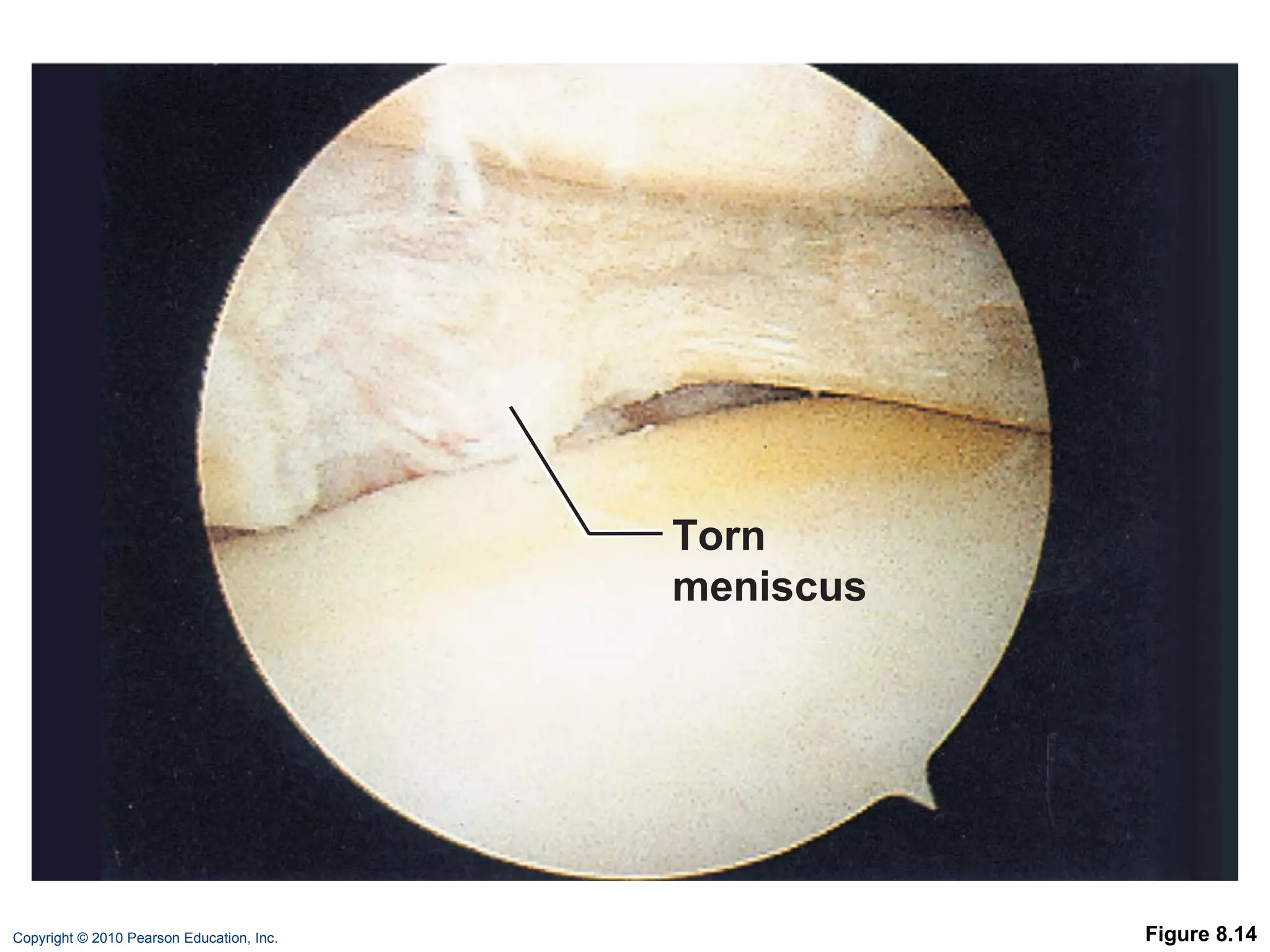
The document describes the six main types of synovial joints classified based on the shape of their articular surfaces: plane, hinge, pivot, condyloid, saddle, and ball-and-socket joints. It then provides more details on specific joints like the knee, shoulder, elbow, hip, temporomandibular, and common joint injuries and conditions like arthritis.