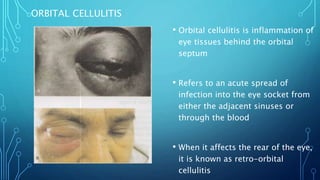
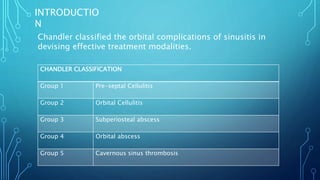
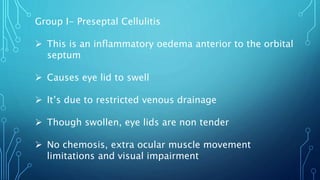
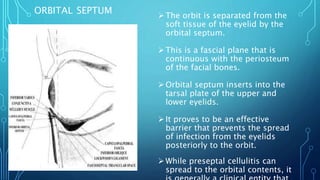
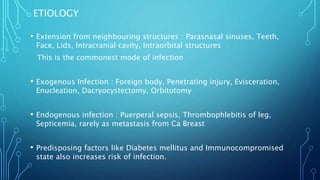
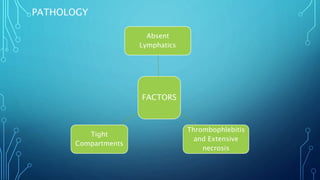
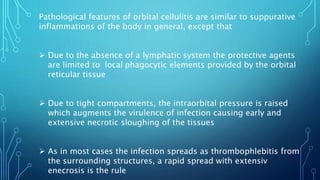
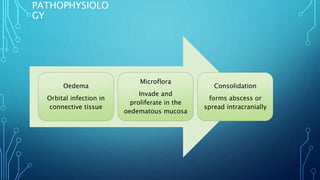
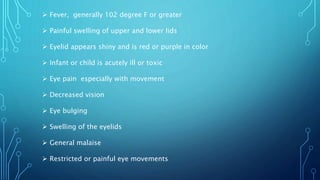
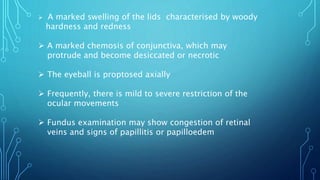
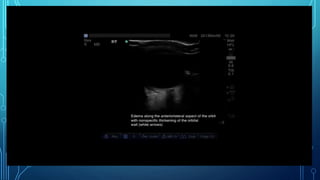
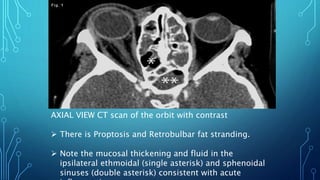
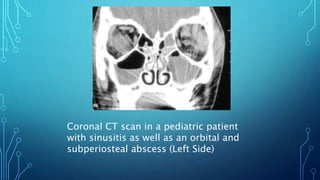
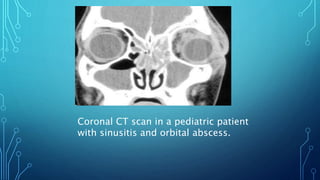
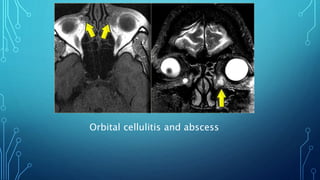
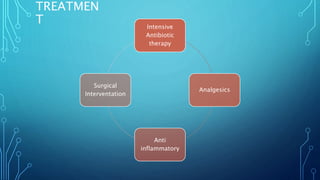
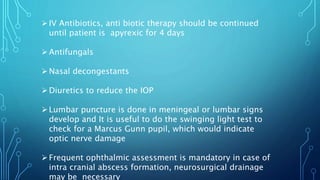
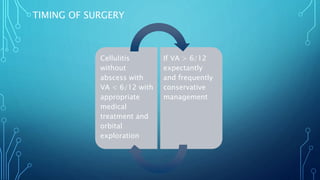
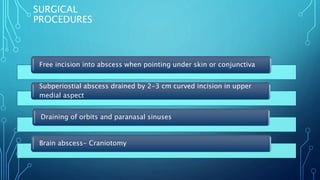
Orbital cellulitis is an infection behind the orbital septum that can spread from adjacent sinuses or bloodstream. It is classified by Chandler into 5 groups based on location and severity. Group 1 is preseptal cellulitis anterior to the septum. Group 2 is orbital cellulitis within the orbit. Group 3 is a subperiosteal abscess between the bone and periosteum. Group 4 is an orbital abscess within orbital contents. Group 5 is cavernous sinus thrombosis spreading bilaterally. Symptoms include eyelid swelling, pain, and vision issues. Imaging helps locate the infection and guide treatment which involves intravenous antibiotics, analgesics, and sometimes surgery.