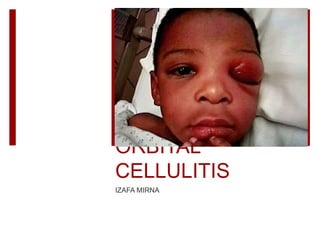
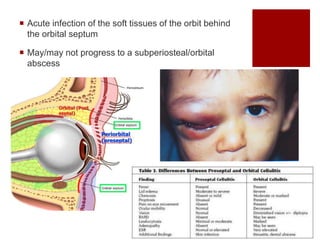
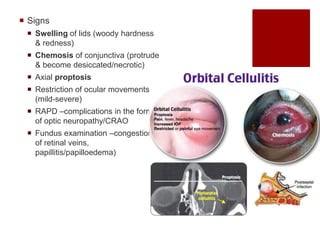
1. Orbital cellulitis is an acute infection of the soft tissues behind the orbital septum that may progress to a subperiosteal or orbital abscess.
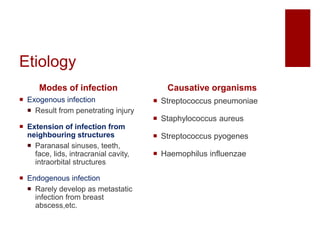
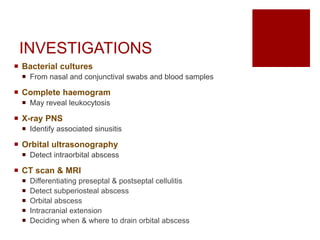
2. It is commonly caused by bacteria like Streptococcus pneumoniae, Staphylococcus aureus, and Streptococcus pyogenes entering through the sinuses, face, or eyes.
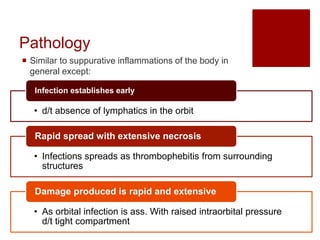
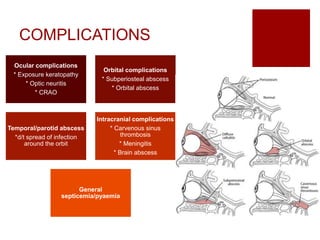
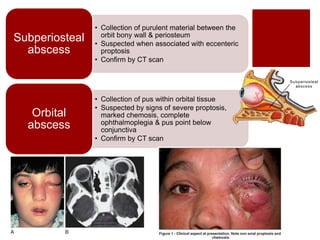
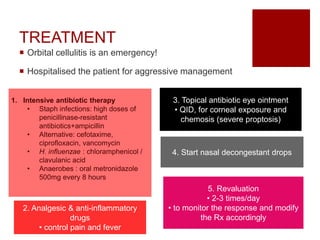
3. Symptoms include eye swelling, pain, and vision issues. Left untreated, it can lead to complications affecting the eye, orbit, sinuses, or brain.