Embed presentation
Downloaded 216 times
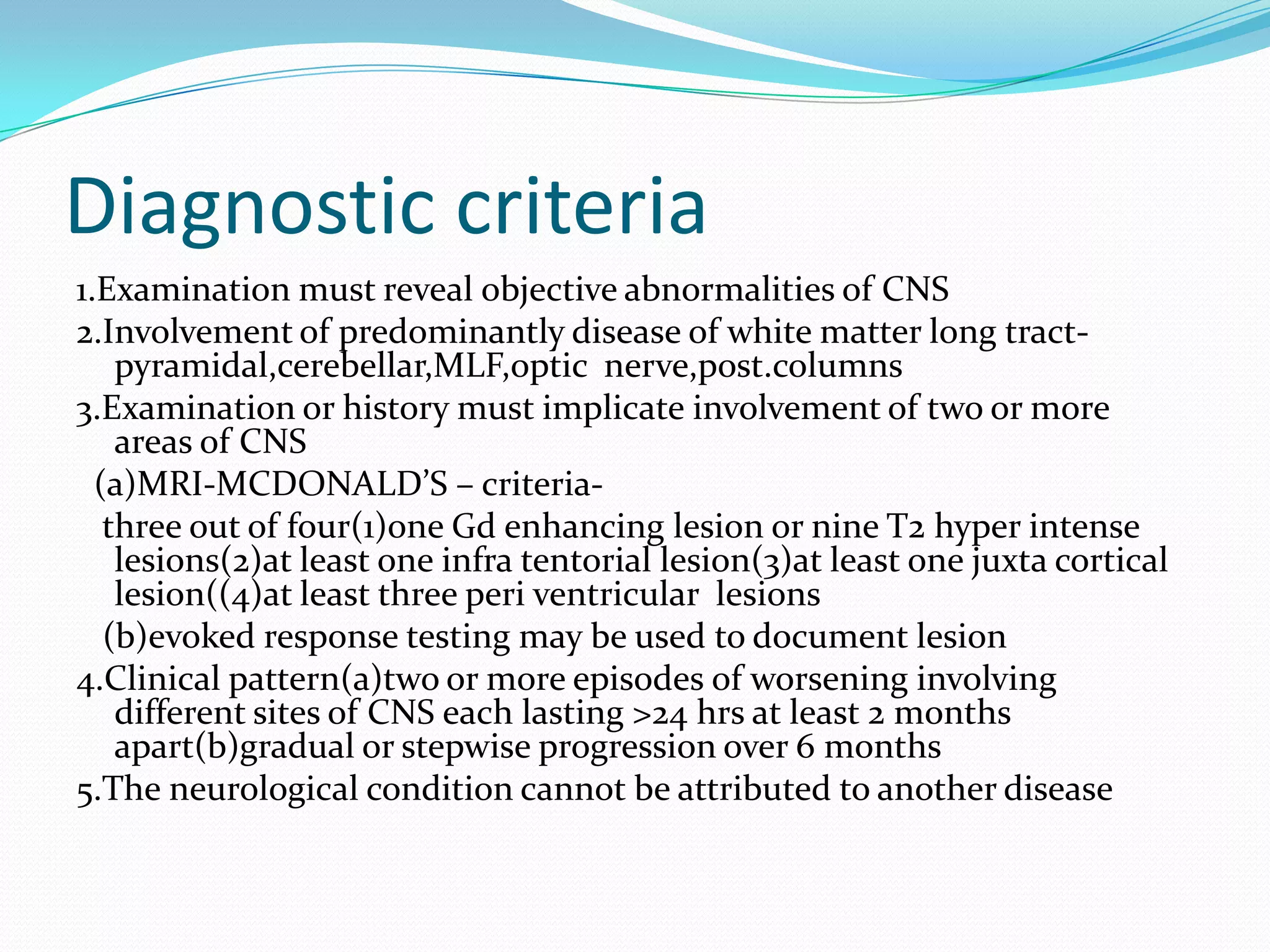
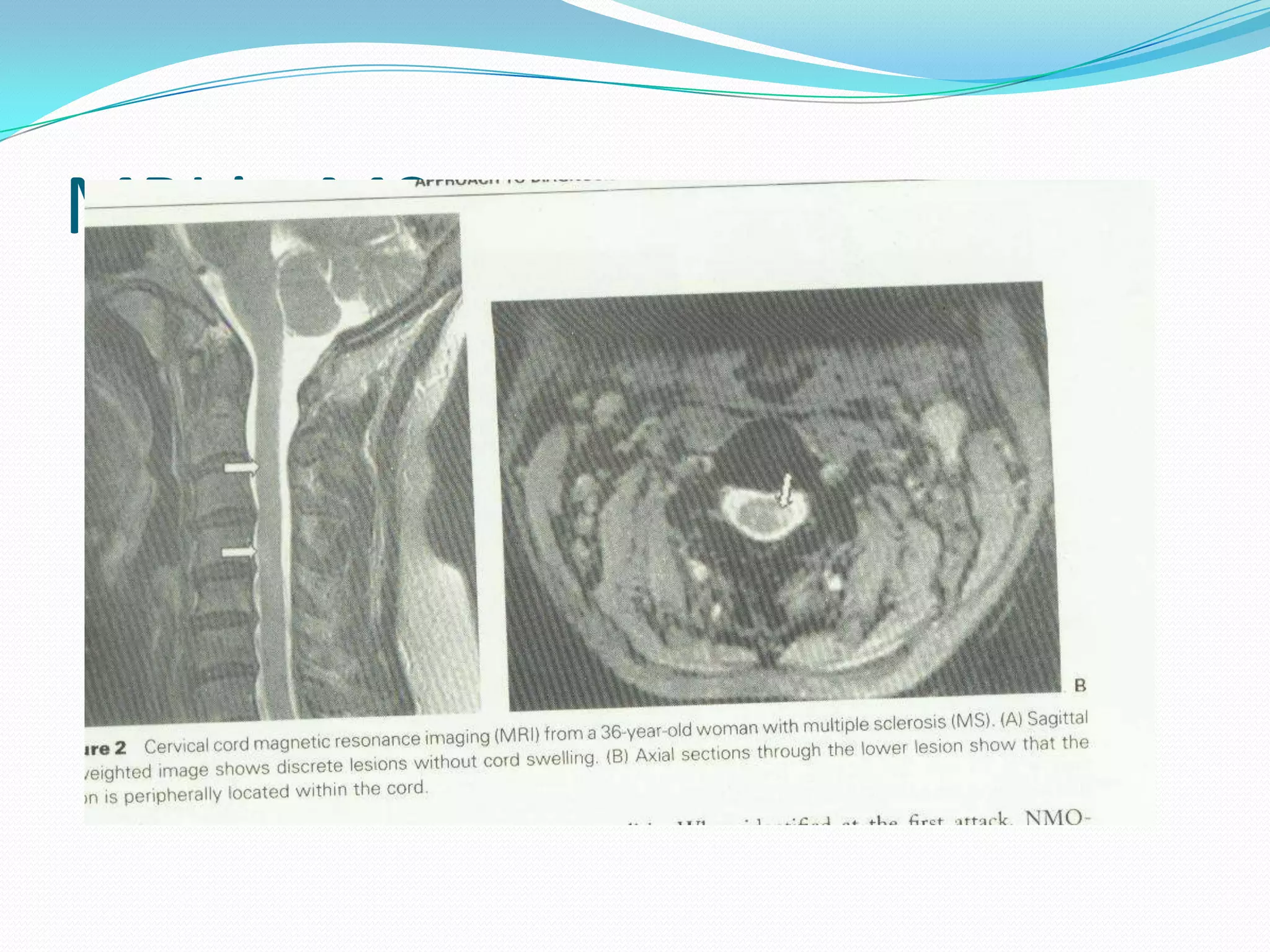
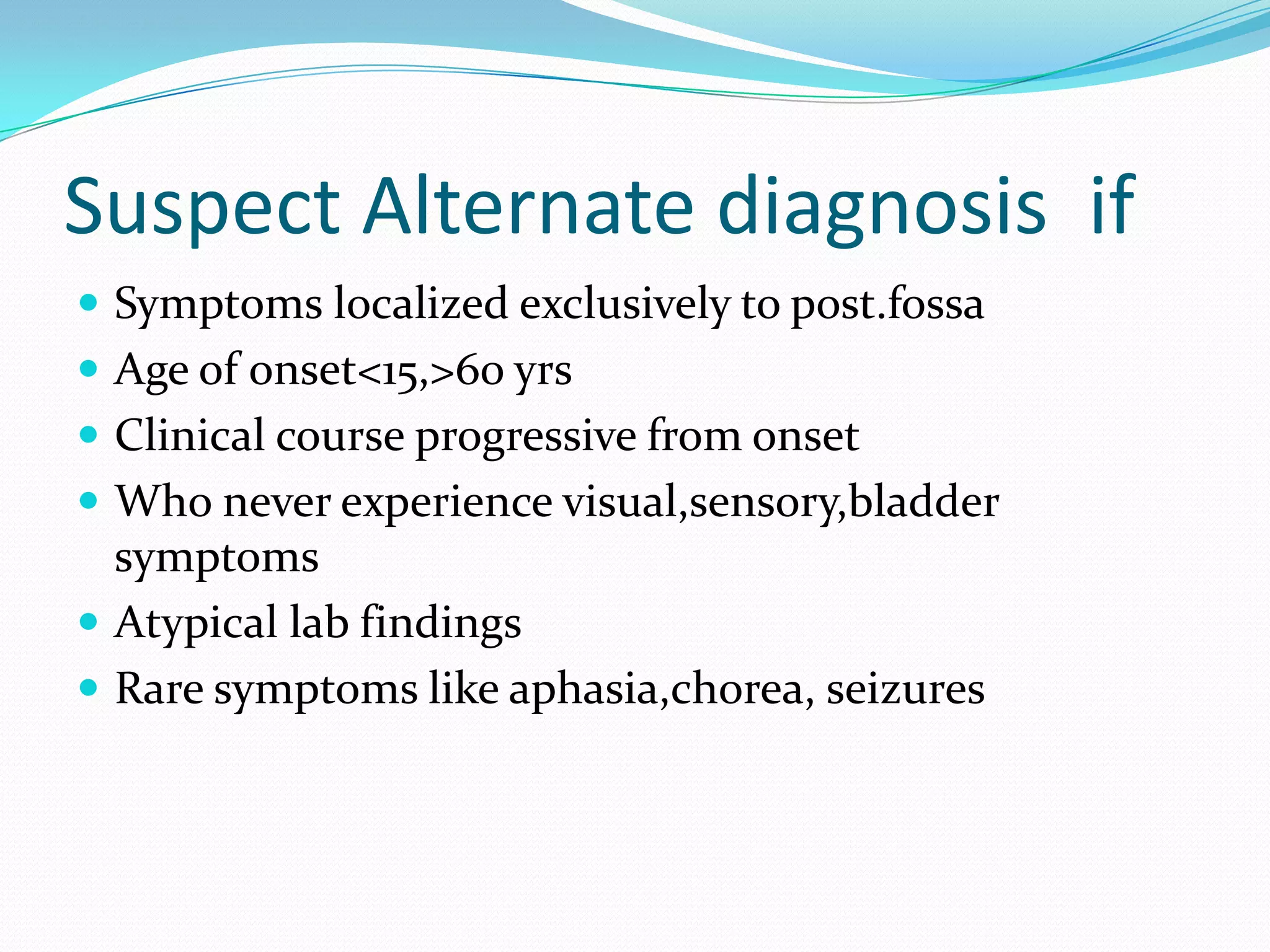

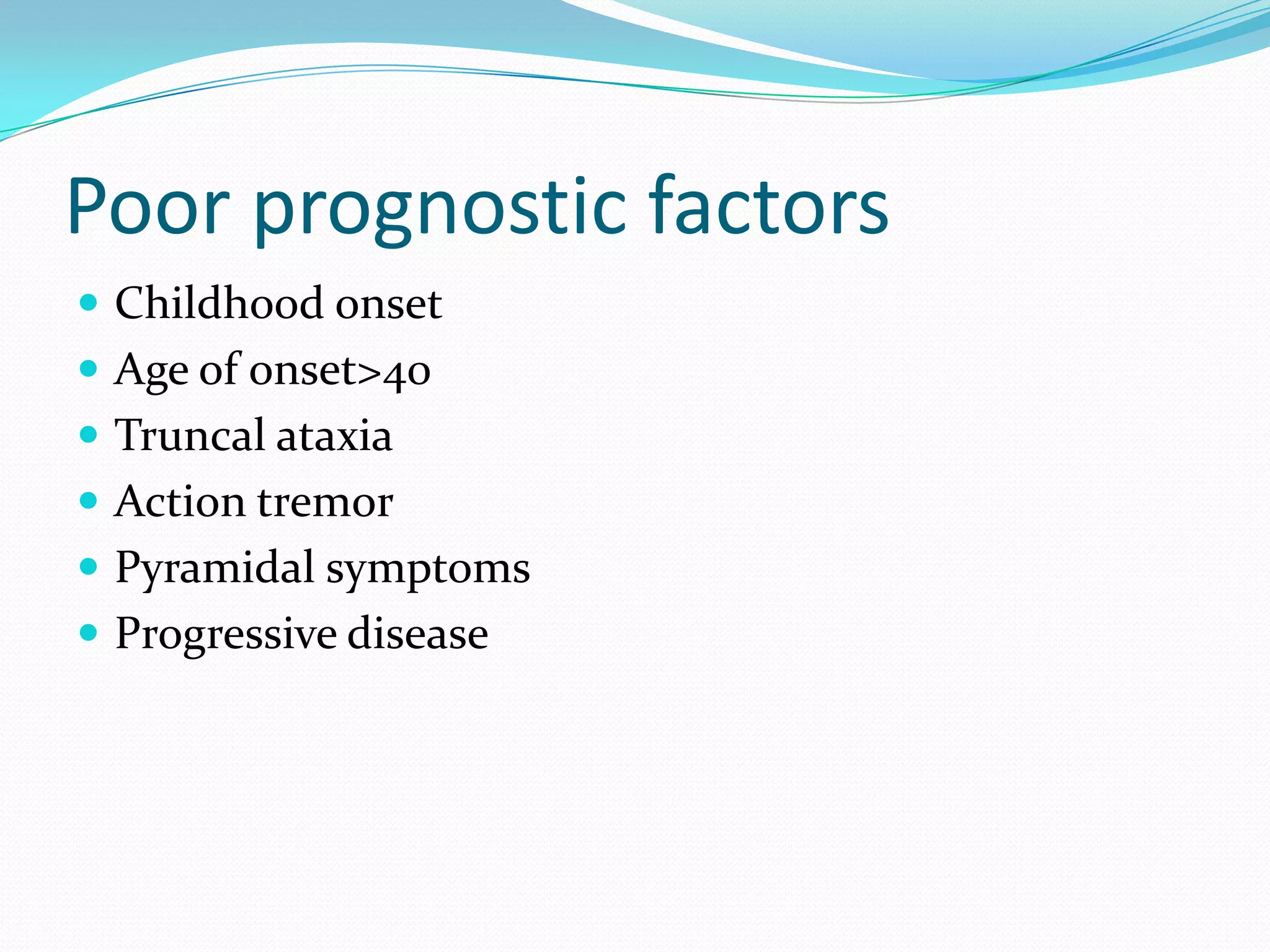
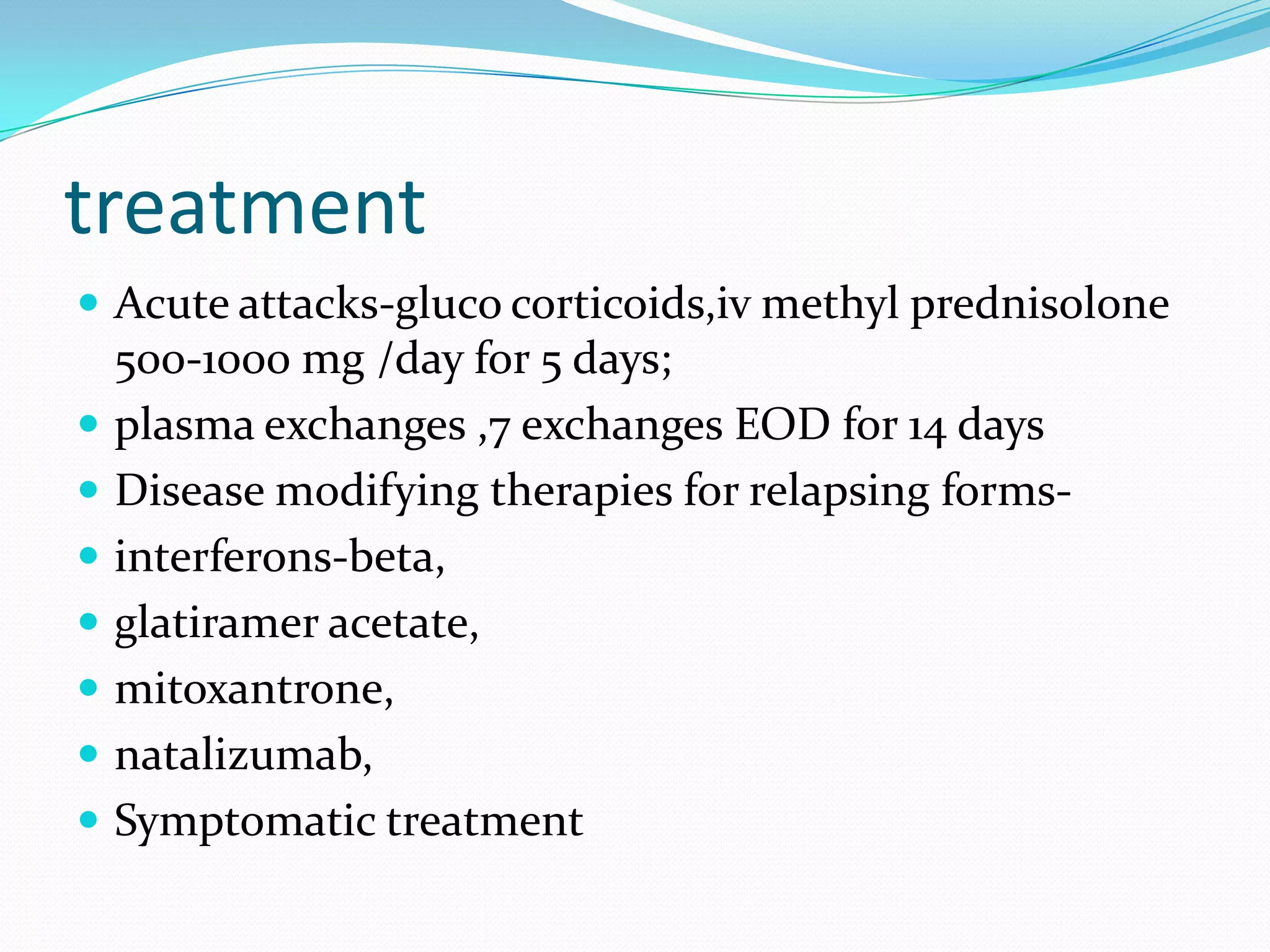

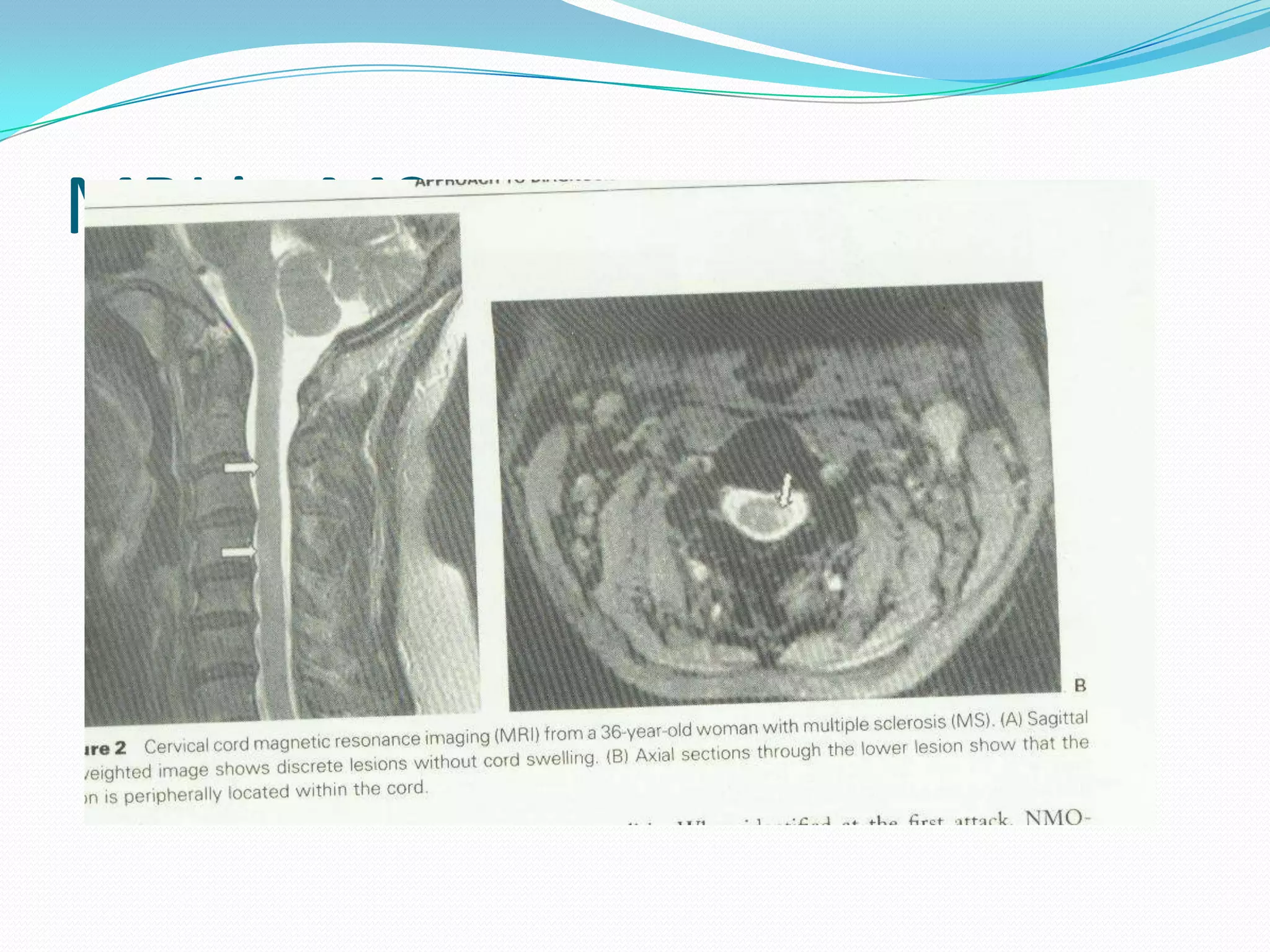
Multiple sclerosis is a demyelinating disease of the central nervous system characterized by inflammation, demyelination, and scarring of the nervous tissue. It can present as either relapsing-remitting or progressive forms. Lesions vary in size and are typically disseminated throughout the white matter of the brain and spinal cord. Diagnosis involves demonstrating dissemination of lesions in time and space through clinical examination, evoked potentials, MRI, and CSF analysis. Treatment involves steroids for acute attacks and disease-modifying therapies such as interferons or glatiramer acetate for relapsing forms.