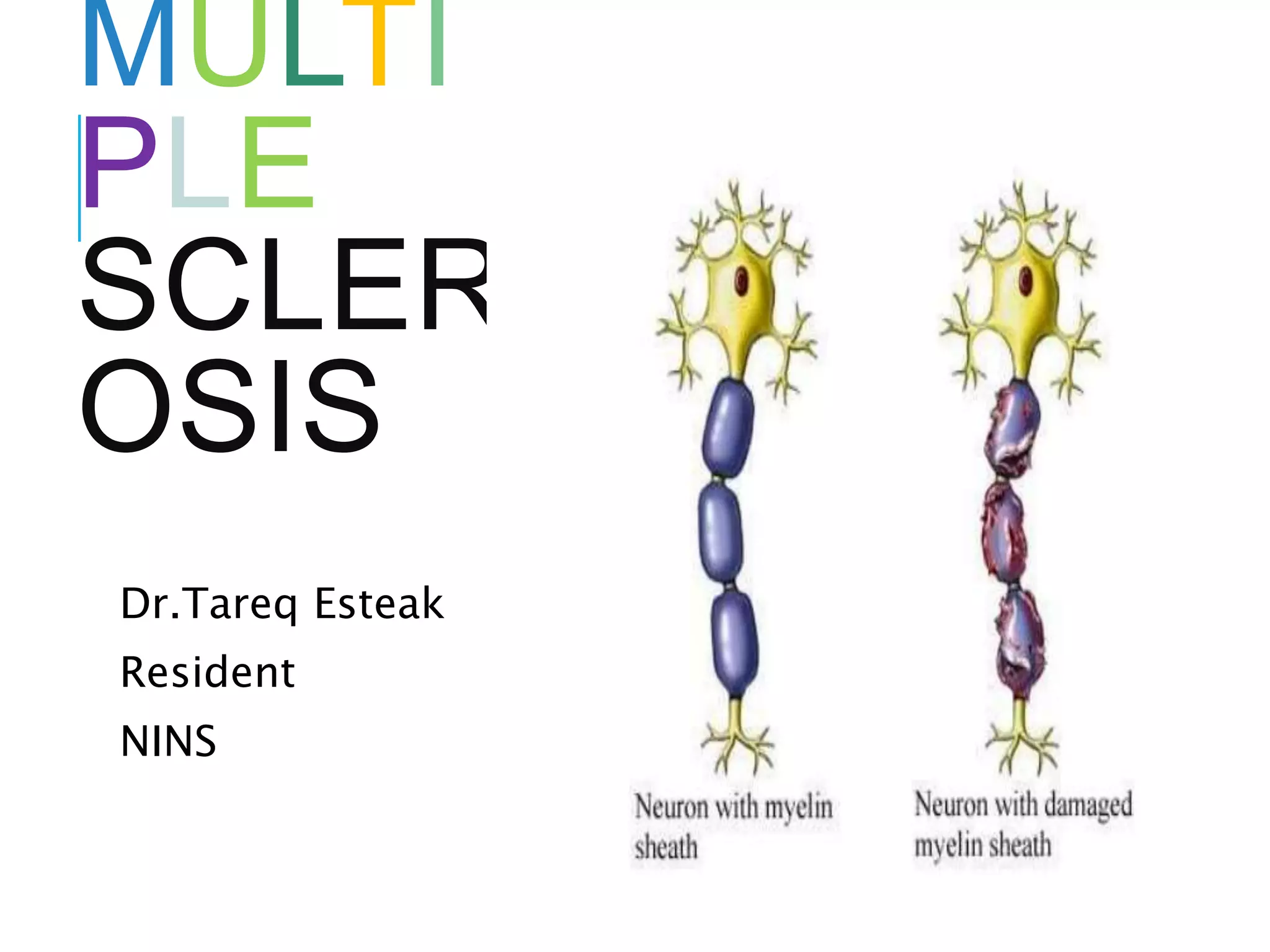
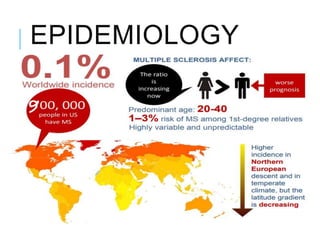
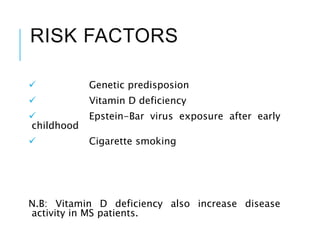
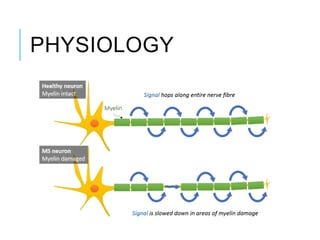
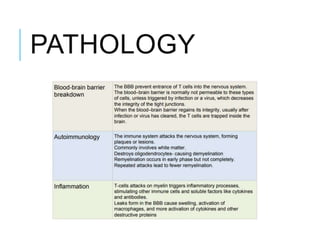
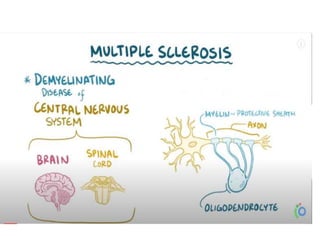
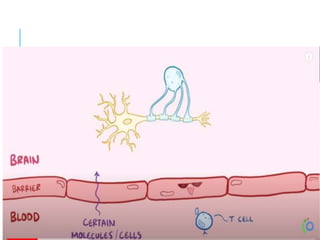
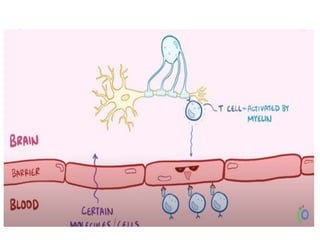
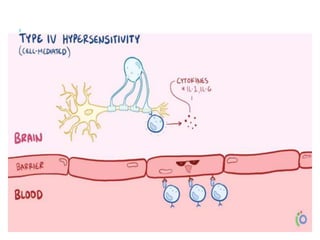
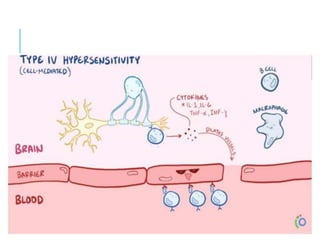
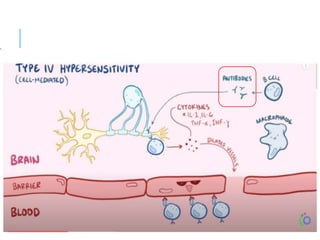
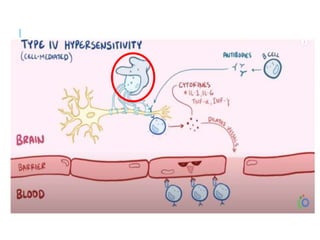
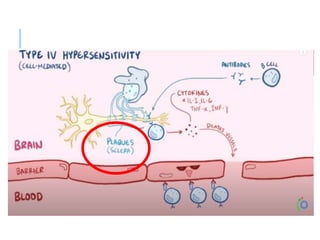
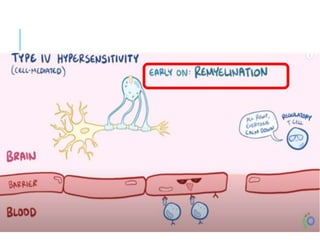
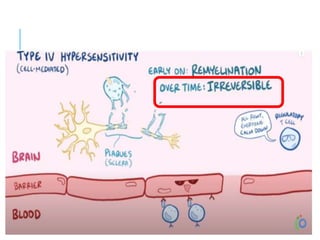
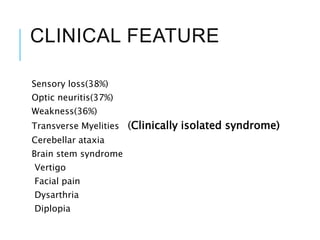
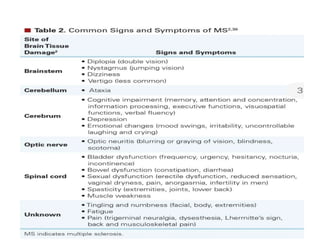
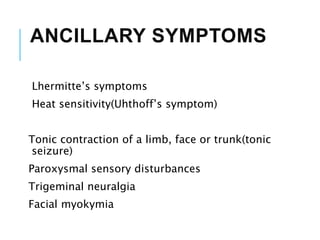
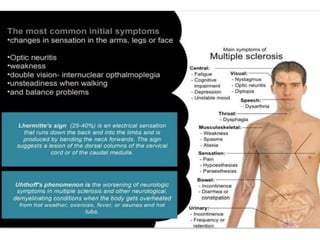
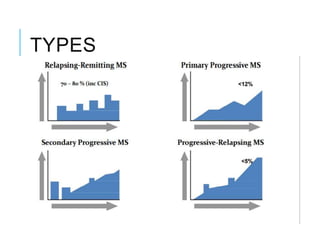
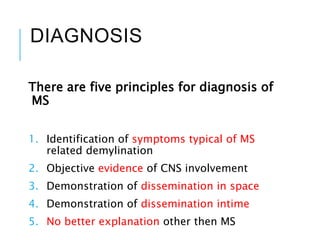
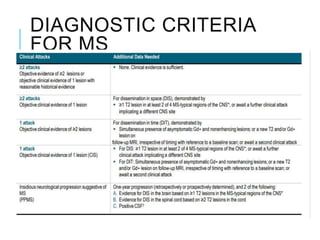
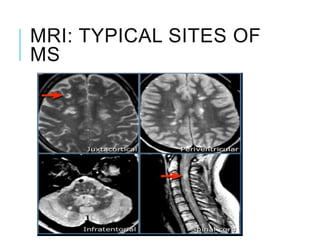
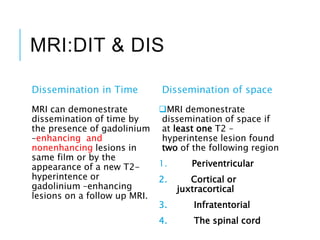
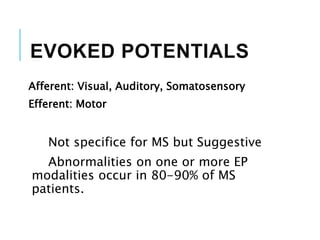
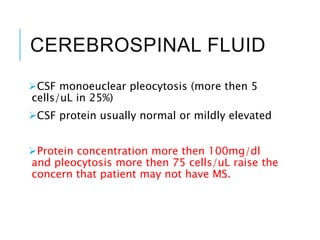
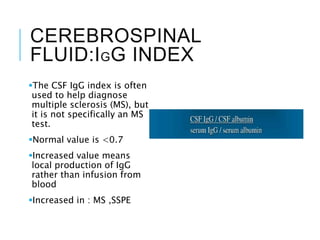
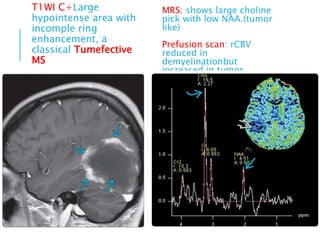
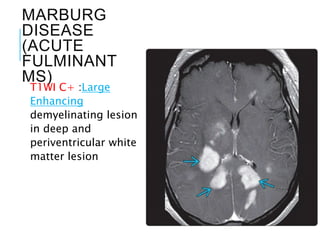
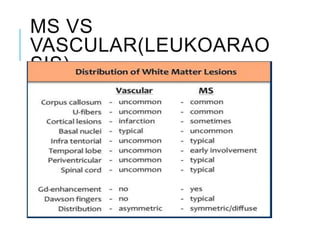
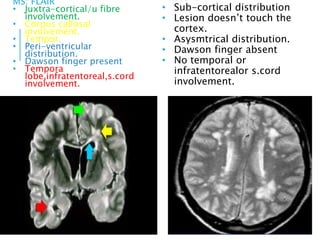
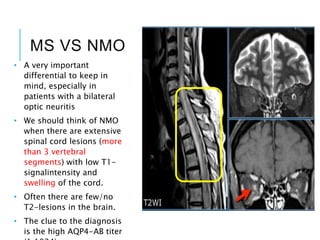
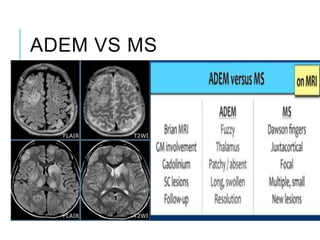
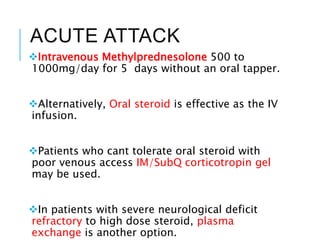
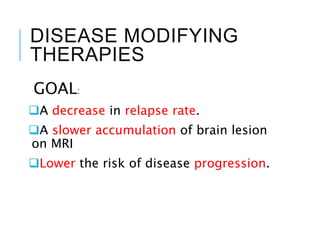
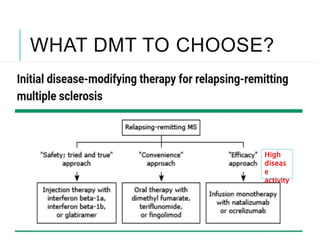
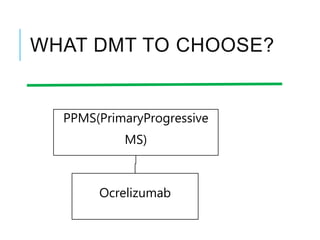
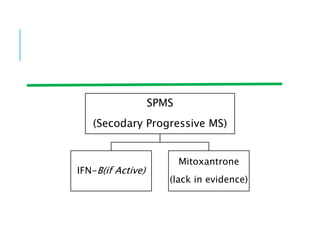
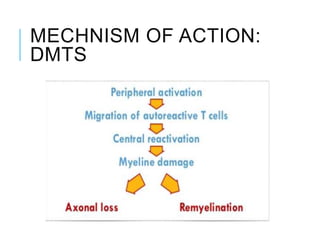
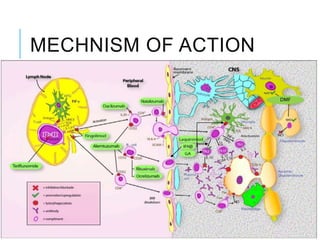
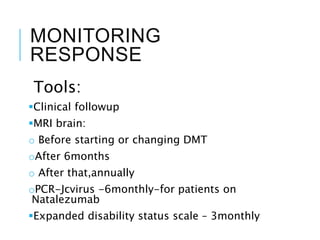
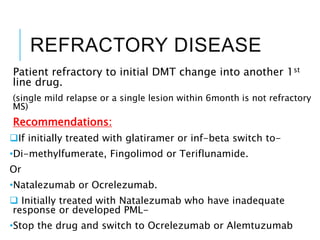
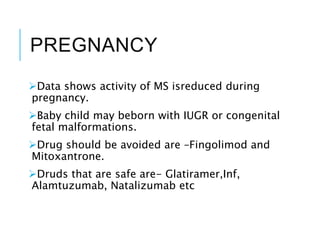
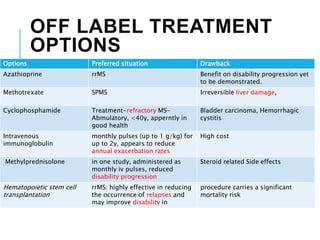
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system characterized by chronic inflammation and demyelination, more prevalent in females aged 20-40. Diagnosis involves identifying symptoms, objective evidence of CNS involvement, and MRI characteristics showing lesions, among other diagnostic tools. Treatment options include acute therapies like intravenous steroids and disease-modifying therapies tailored based on disease activity, with special considerations for pregnancy and COVID-19.