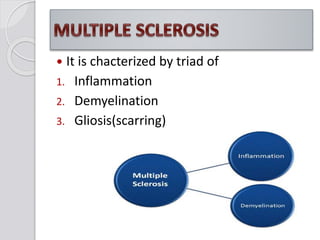
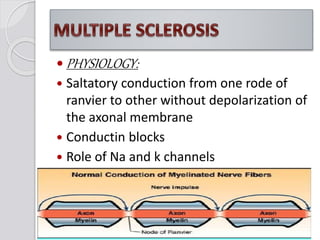
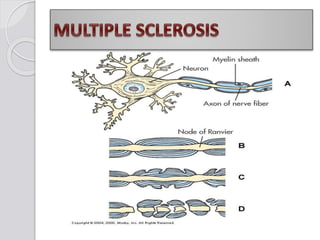
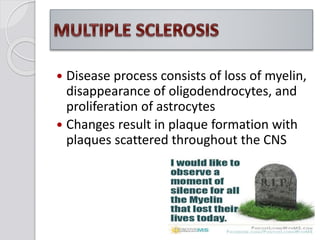
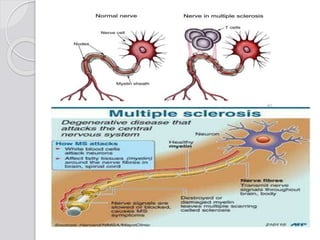
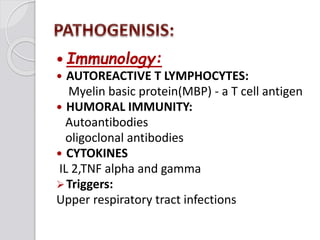
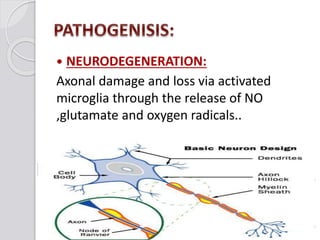
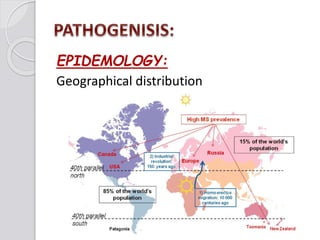
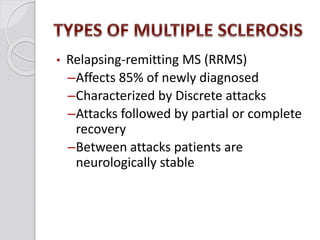
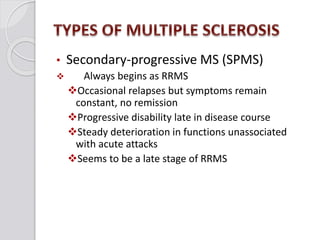
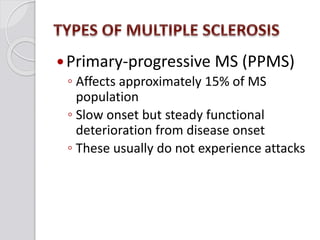
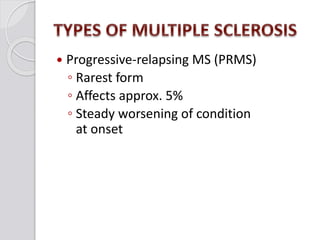
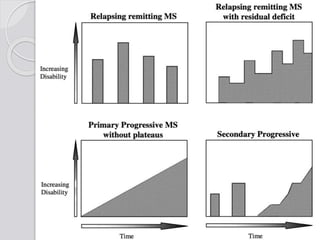
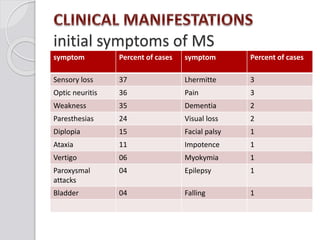
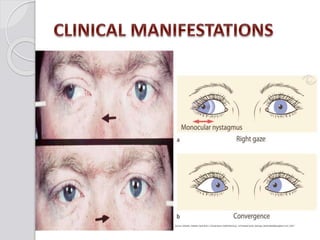
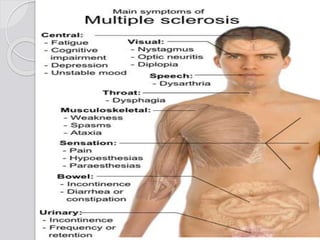
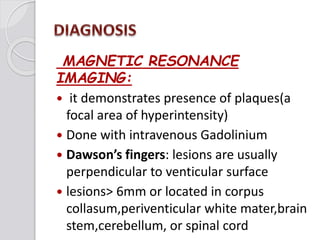
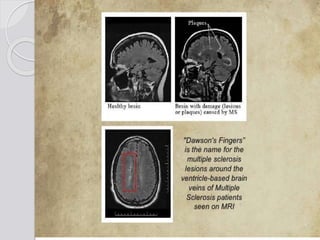
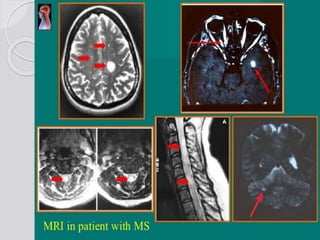
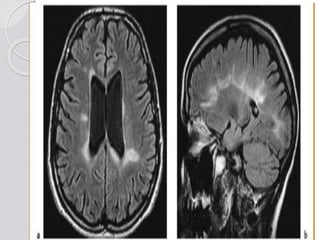
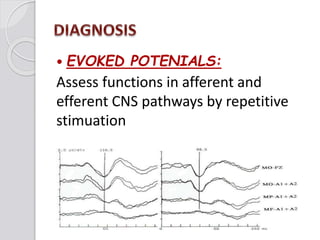
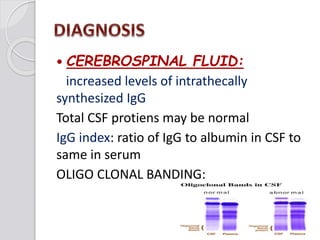
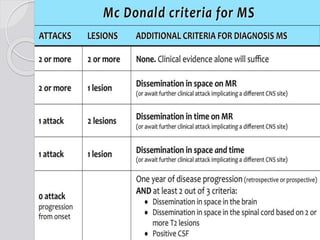
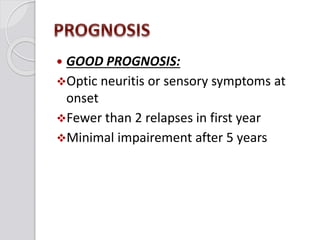
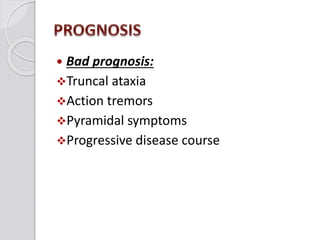
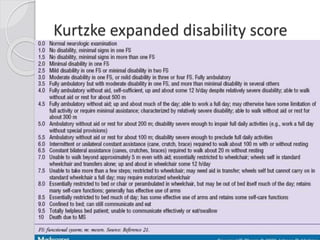
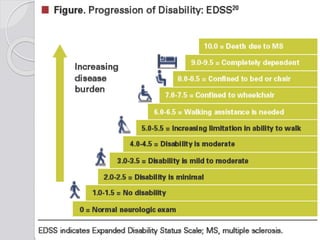
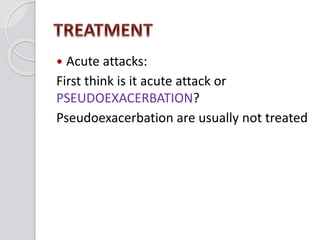
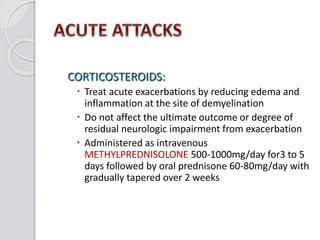
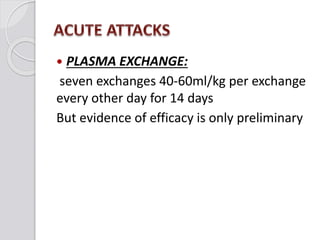
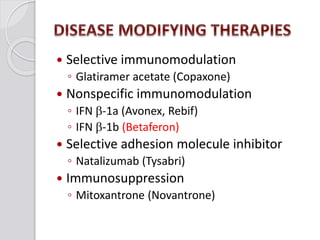
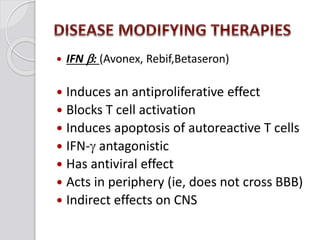
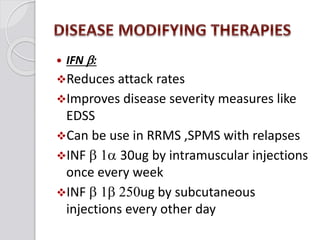
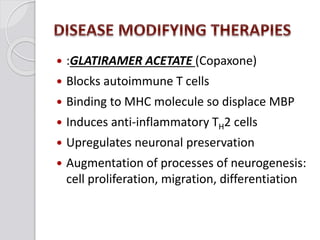
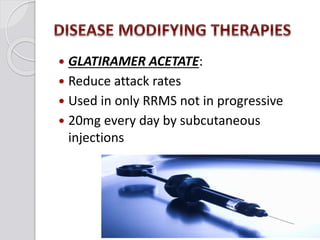
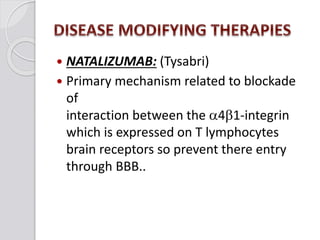
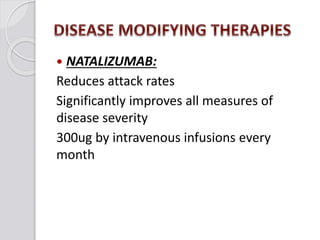
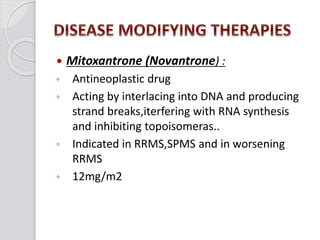
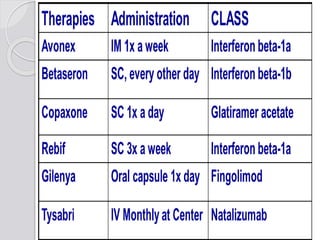
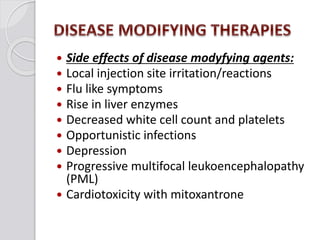
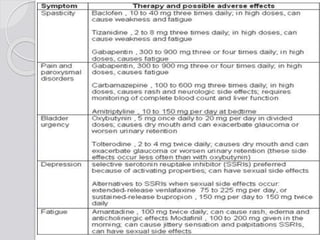
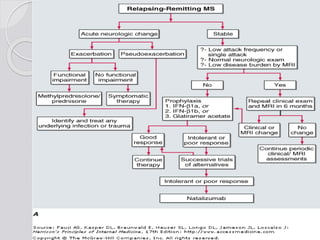
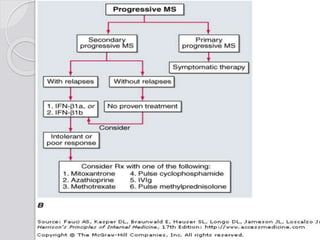
This document discusses multiple sclerosis (MS), a demyelinating disease of the central nervous system. It begins by defining MS and describing its characteristic features, including inflammation, demyelination, and scarring in the brain and spinal cord. It then covers the clinical manifestations of MS, diagnostic testing methods, treatment approaches including disease-modifying drugs, and potential side effects of treatments.