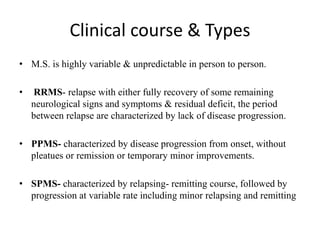
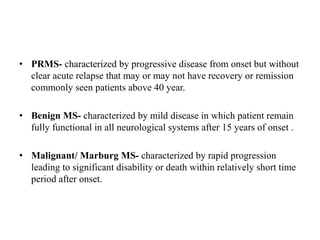
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease of the central nervous system that typically affects young adults between the ages of 20-40. It is characterized by immune-mediated damage to the myelin sheath and axons in the brain and spinal cord, leading to demyelination and potentially axonal loss. Symptoms vary depending on the location of lesions in the CNS but may include sensory and visual disturbances, motor impairments, cognitive issues, and others. The disease course is unpredictable and can be relapsing-remitting, primary progressive, secondary progressive, or progressive relapsing. There is no known cure for MS and treatment aims to manage symptoms and reduce disease progression.