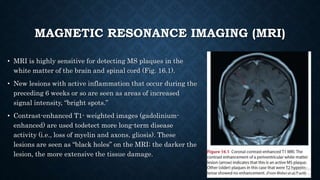
This document provides an overview of multiple sclerosis (MS). It describes MS as an autoimmune disease characterized by inflammation and damage to the protective myelin sheath surrounding nerves. The document discusses that MS most commonly affects people between the ages of 20-40, is more prevalent in women than men, and is more common in white populations. Genetic and environmental factors like viral infections are thought to contribute to MS risk. Magnetic resonance imaging, evoked potentials, and cerebrospinal fluid analysis are used to diagnose MS by detecting lesions in the brain and spinal cord. Available treatment options aim to reduce inflammation and prevent relapses.