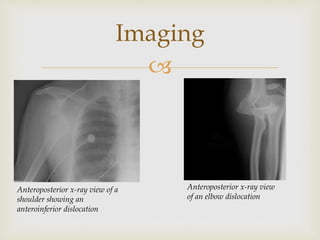
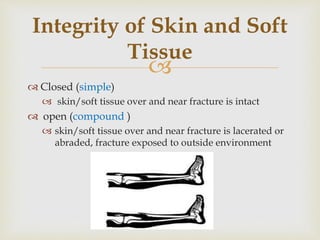
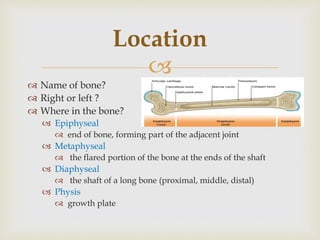
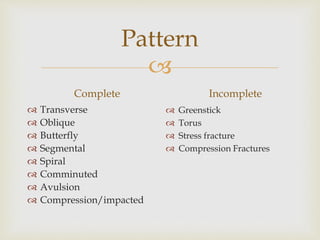
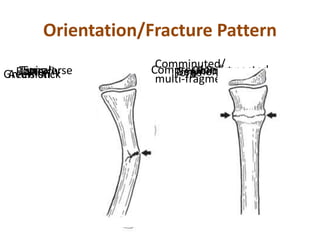
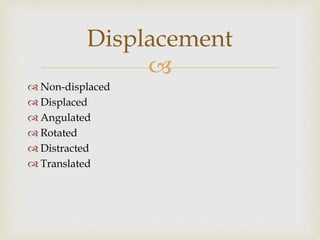
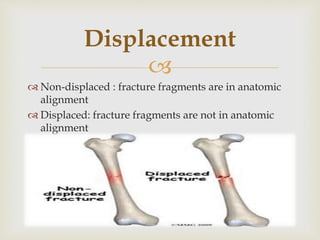
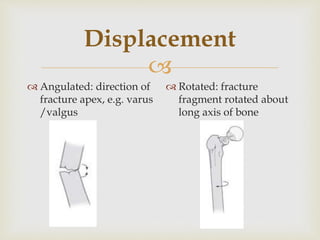
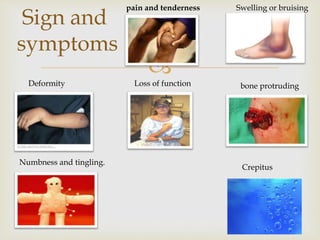
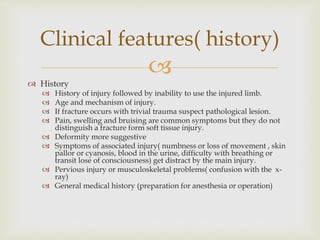
This document provides an outline on fractures and dislocations. It begins with definitions of fractures and dislocations. It then discusses causes of fractures and a classification system that considers displacement, pattern, location, and integrity of skin/soft tissue. Clinical features of fractures like pain, swelling, deformity are outlined. Methods of pain control and typical treatment approaches like reduction, immobilization, and exercise are summarized. Common sites of dislocations and their diagnosis involving history, examination, and imaging are briefly covered. References used are listed at the end.




![
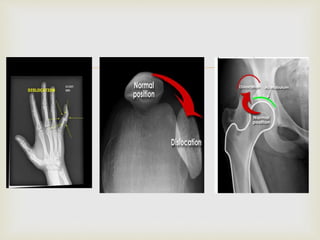
Common site of
dislocations
The most commonly
dislocated is the shoulder
joint.[13]
Elbow: Posterior dislocation,
90% of all elbow
dislocations[14]
Wrist: Lunate and Perilunate
dislocation most common[15]
Finger: Interphalangeal (IP)
or metacarpophalangeal
(MCP) joint dislocations[16]
Hip: Posterior and anterior
dislocation of hip](https://image.slidesharecdn.com/fracturesanddislocations-150209152226-conversion-gate02/85/Fractures-and-dislocations-31-320.jpg)