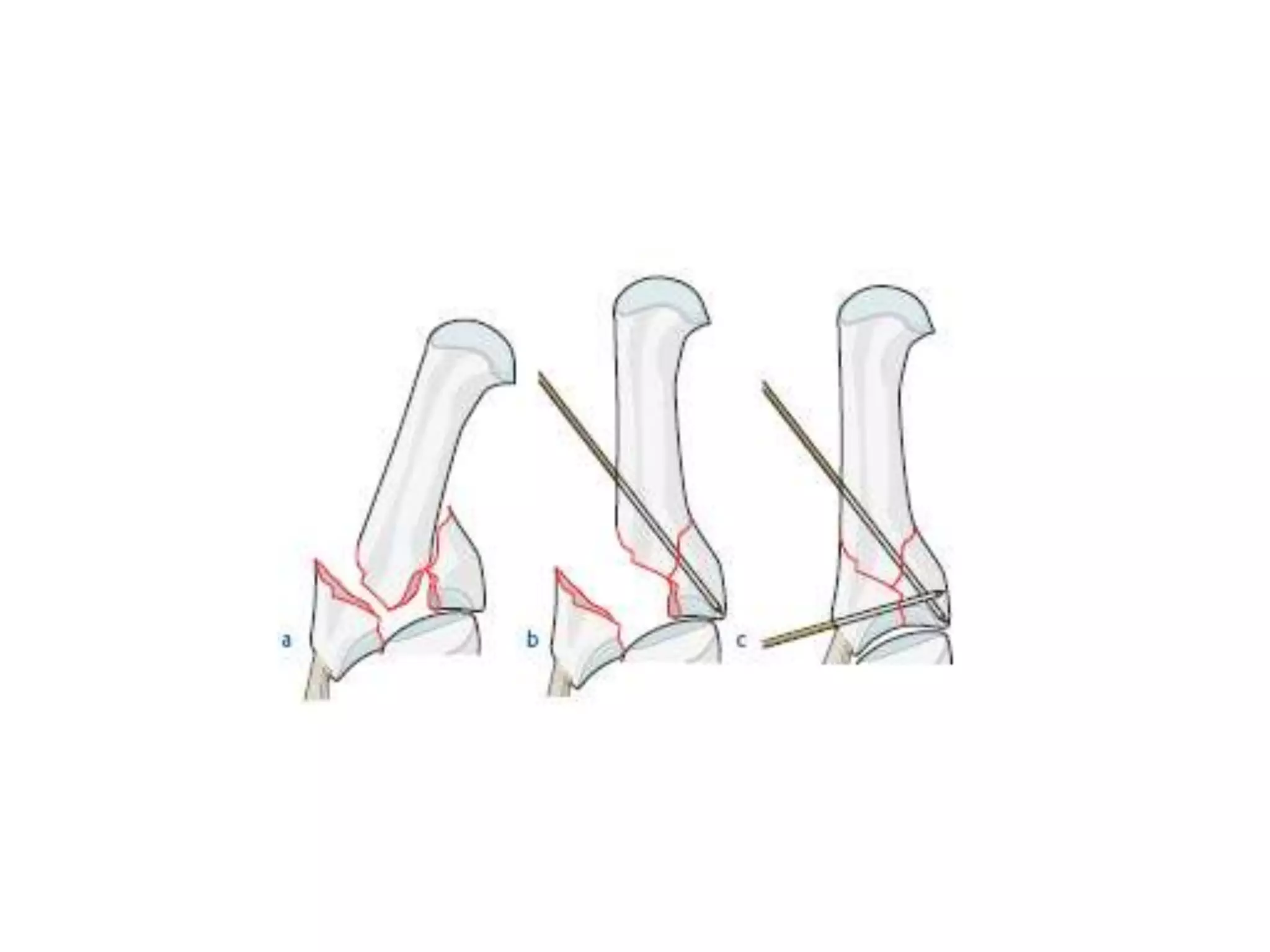
This document discusses fractures and dislocations of the hand. It begins with basic hand anatomy and principles of management for hand injuries. It then discusses specific injuries including Bennett's fracture of the thumb, Rolando fracture of the thumb base, and fractures of the thumb carpometacarpal joint. It also covers fractures of the finger metacarpophalangeal and interphalangeal joints. Treatment options including splinting, pinning, and plating are described for various injuries. The goal is to address the injury while maximizing joint mobility and function.