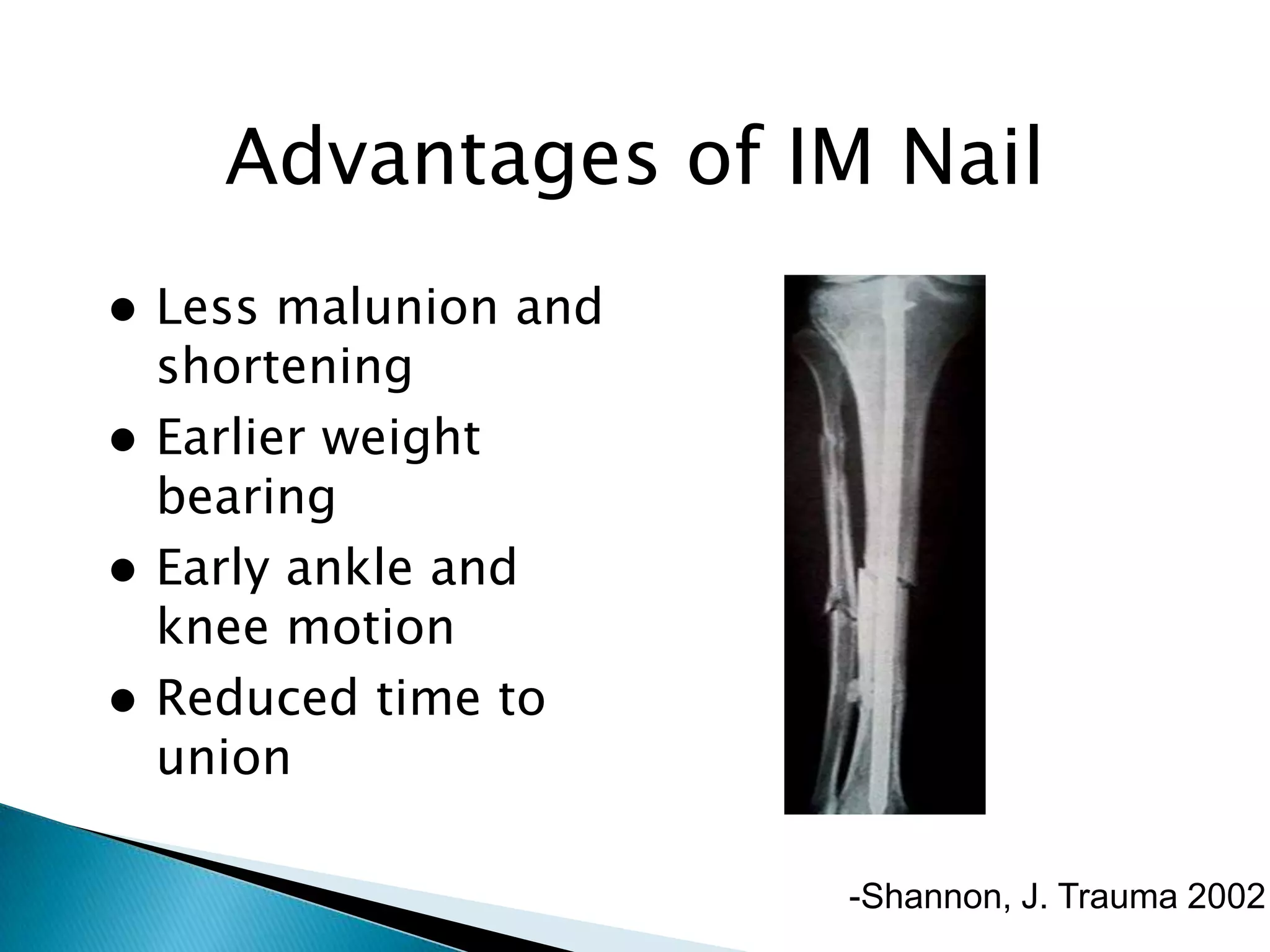
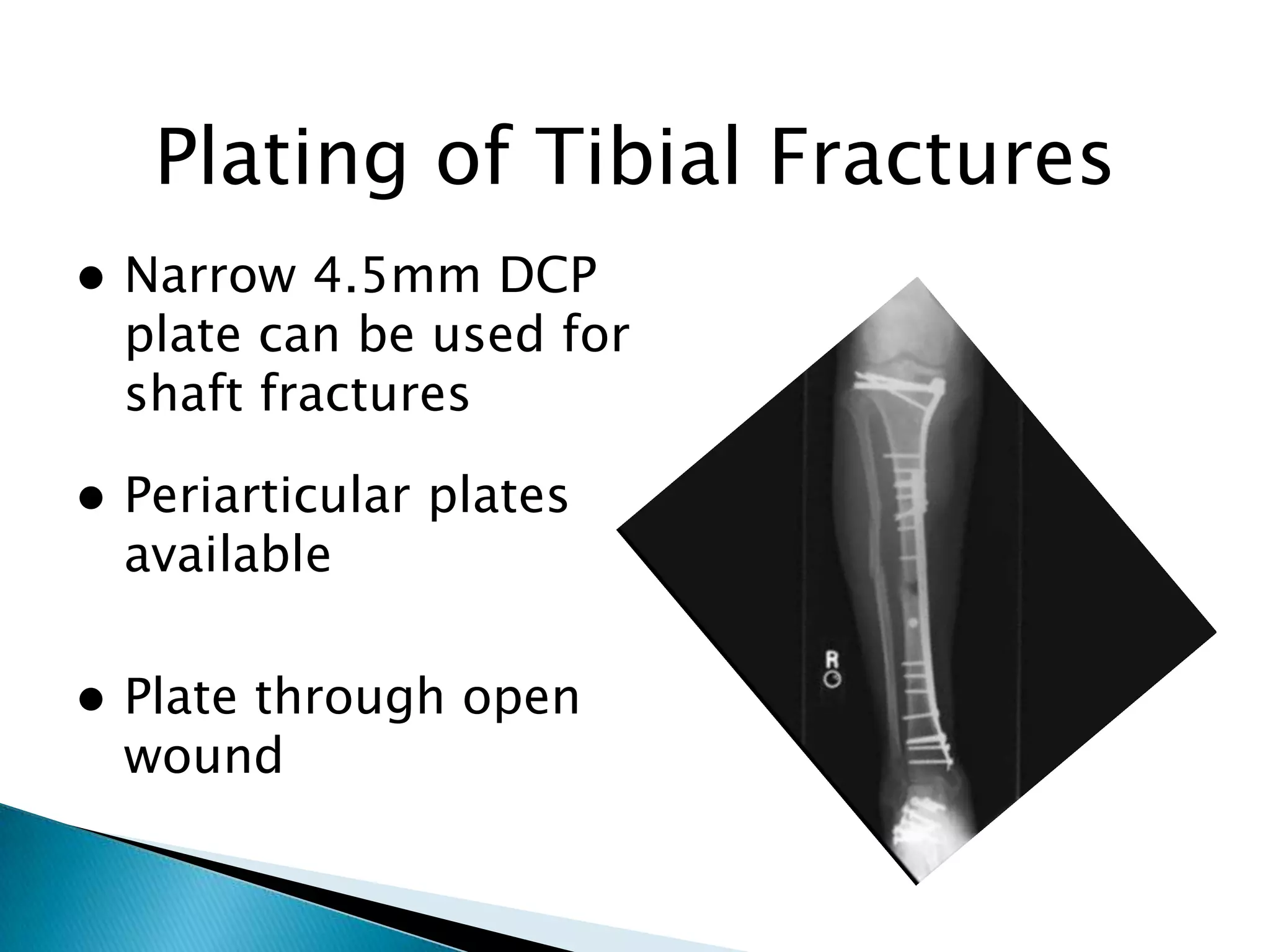
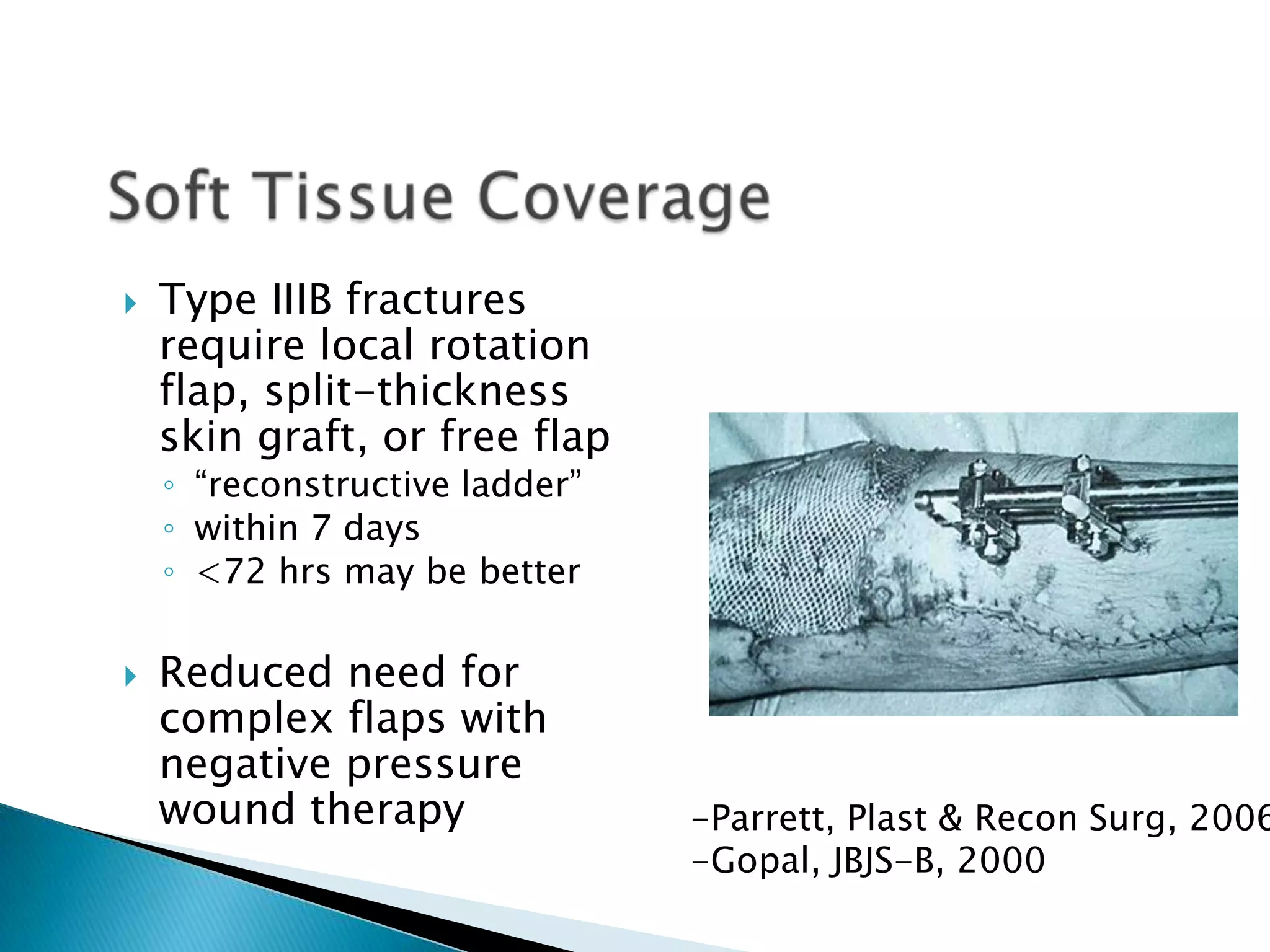
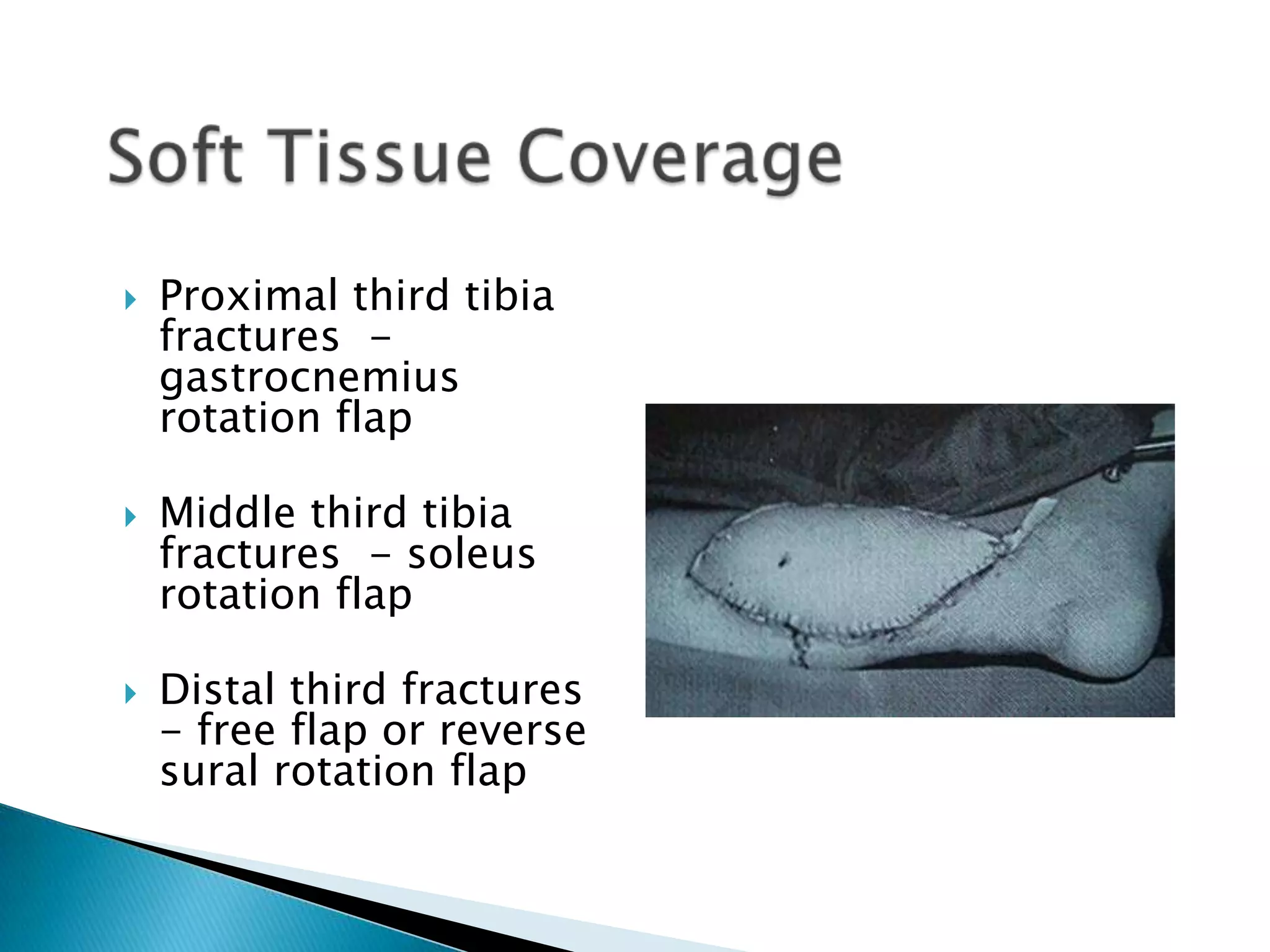
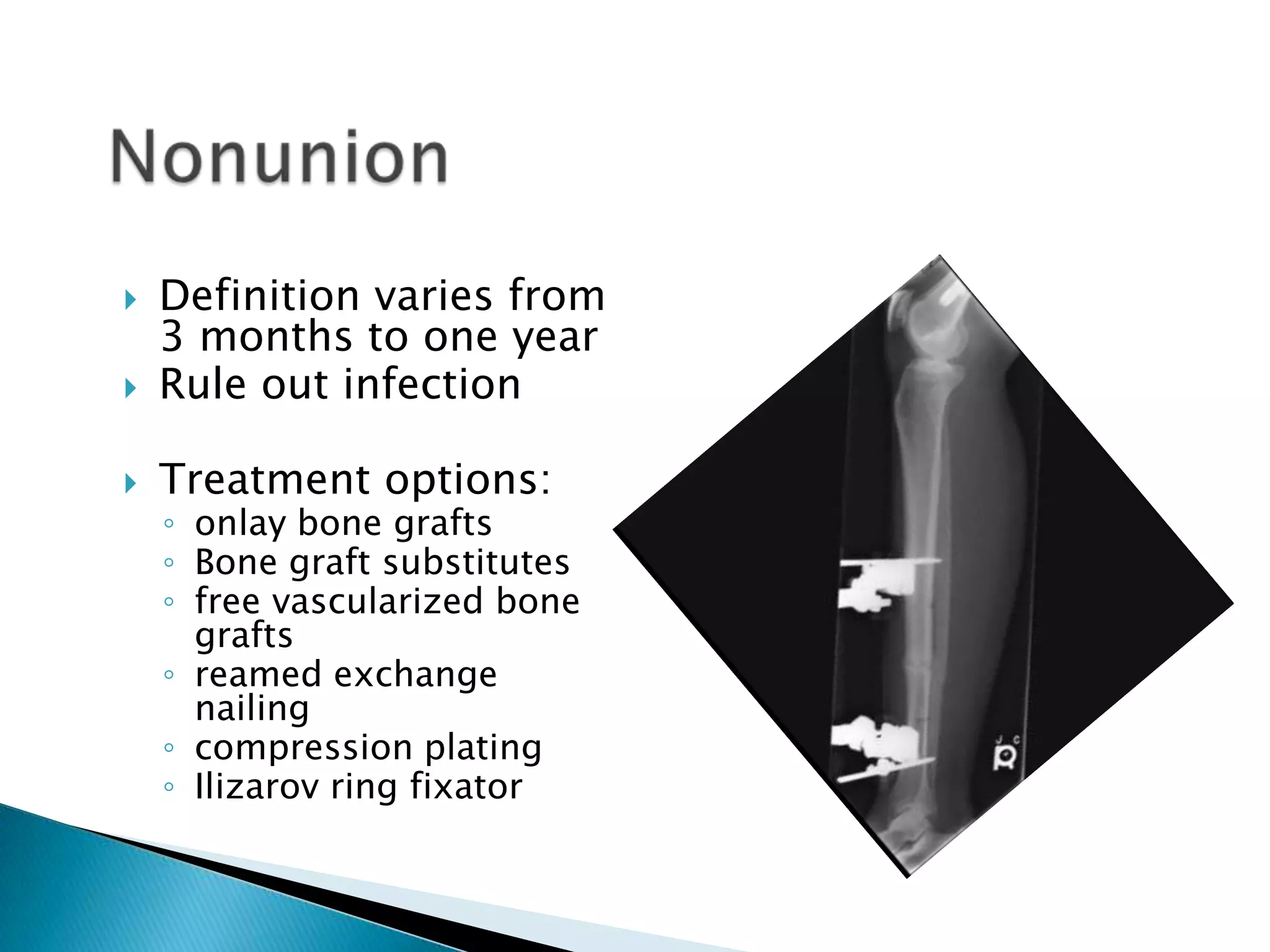
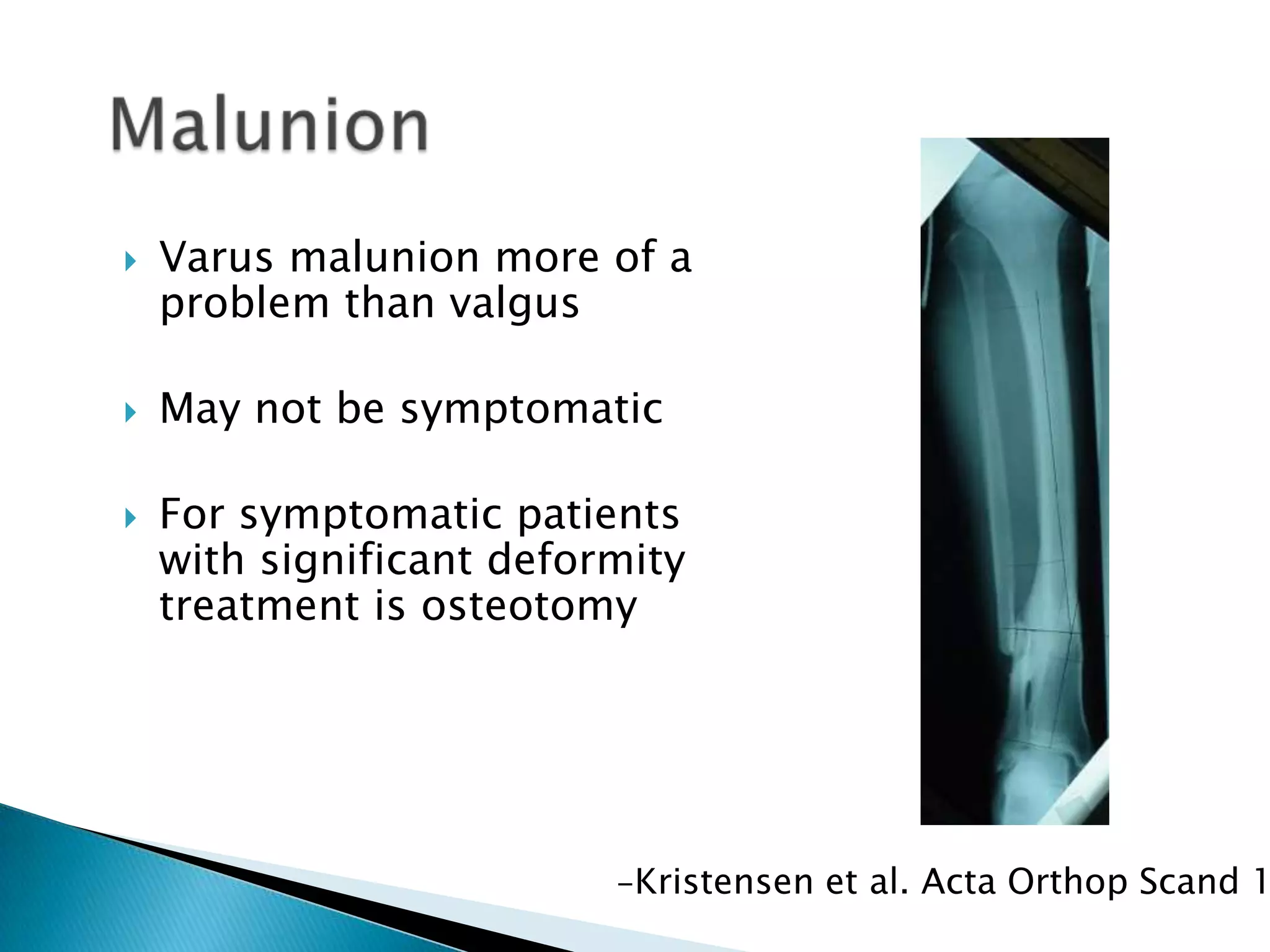
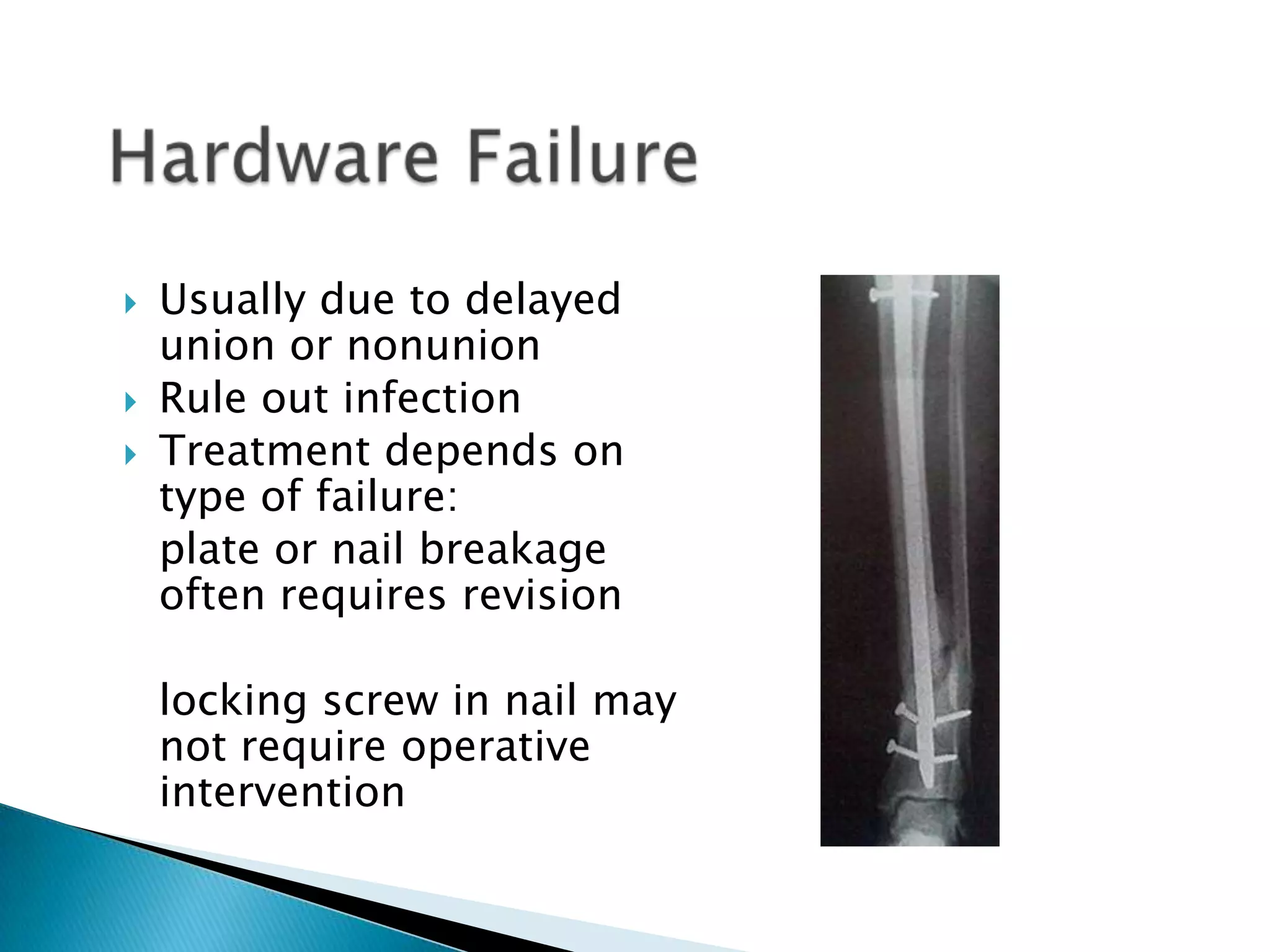
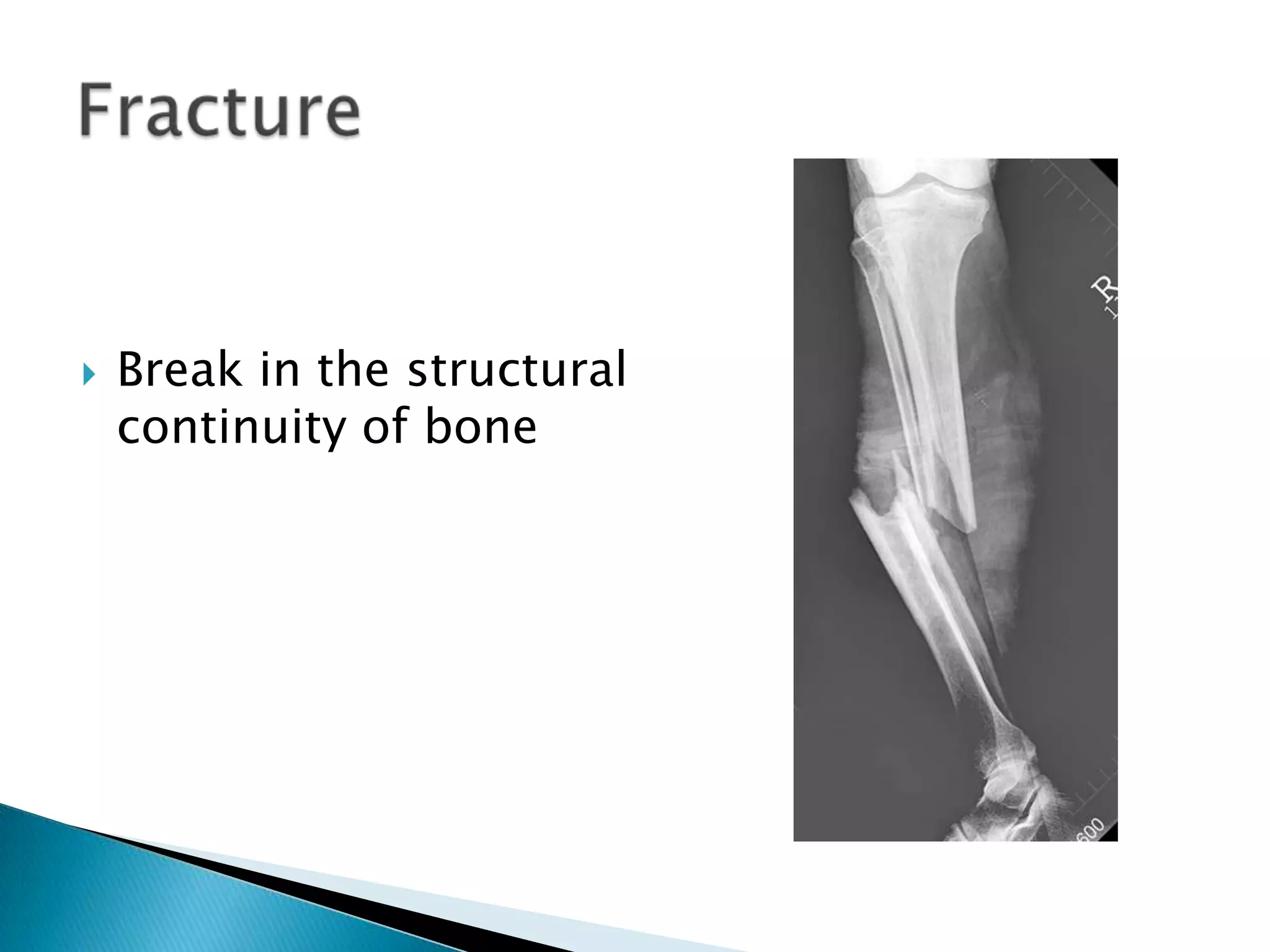
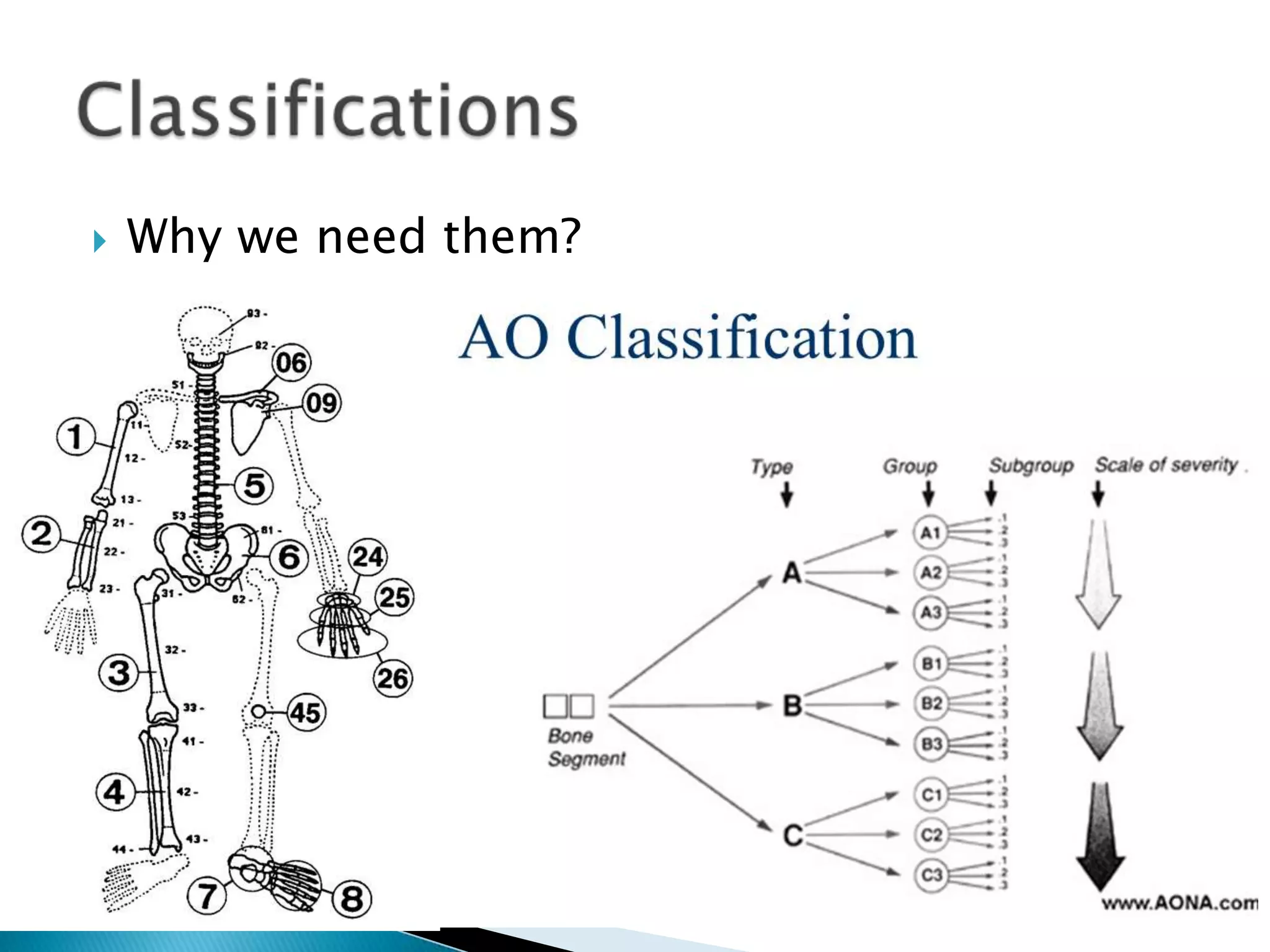
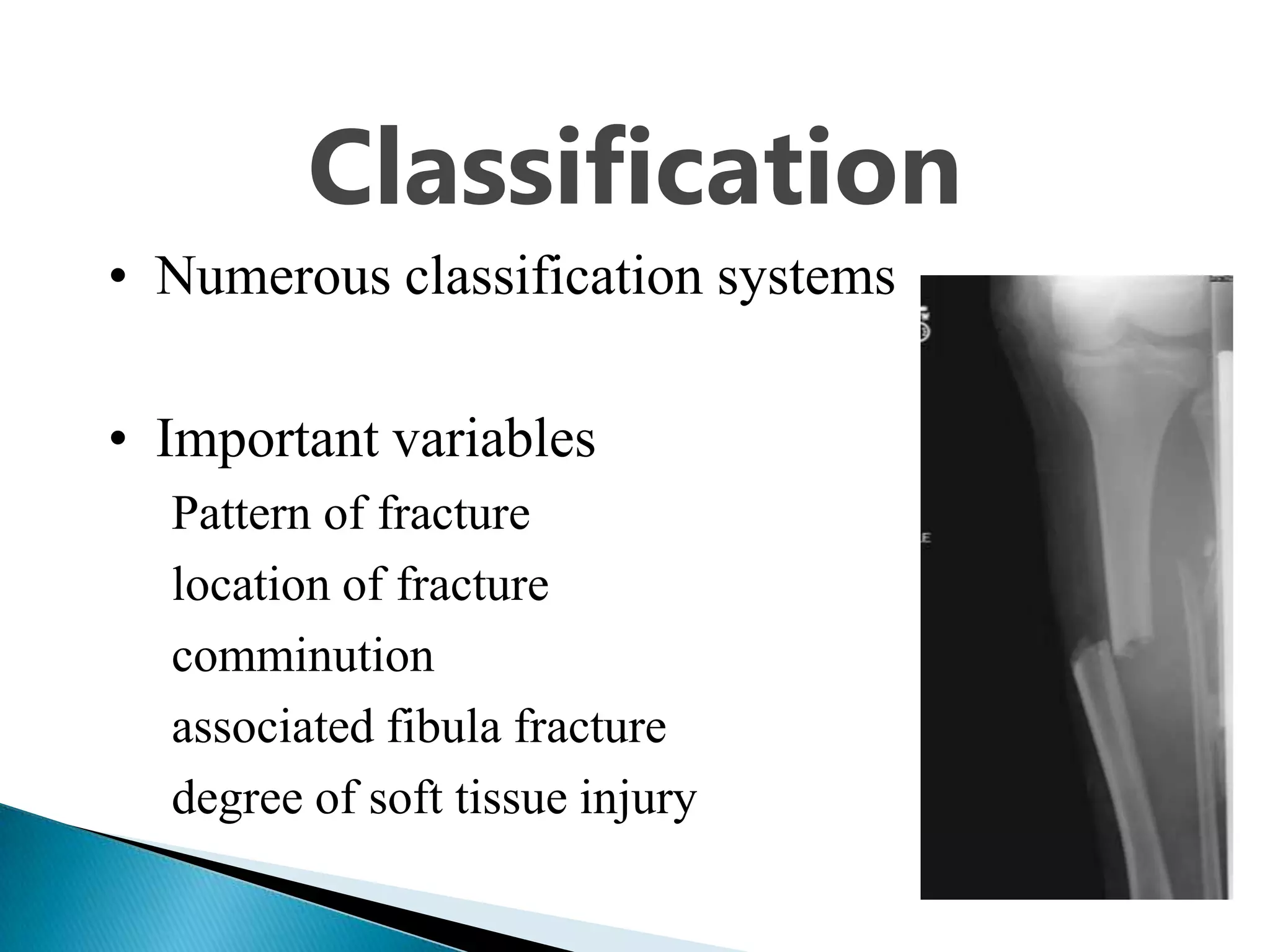
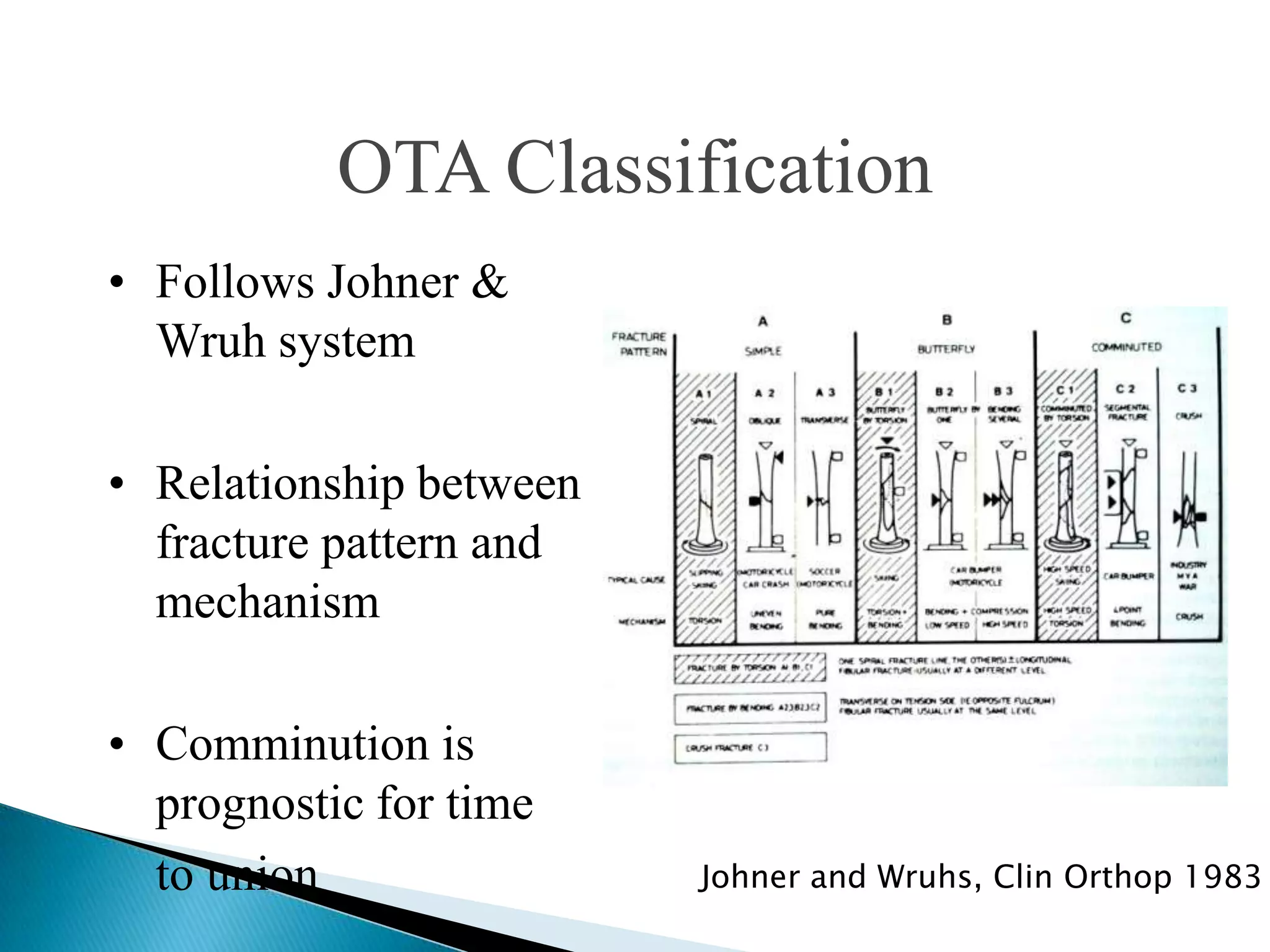
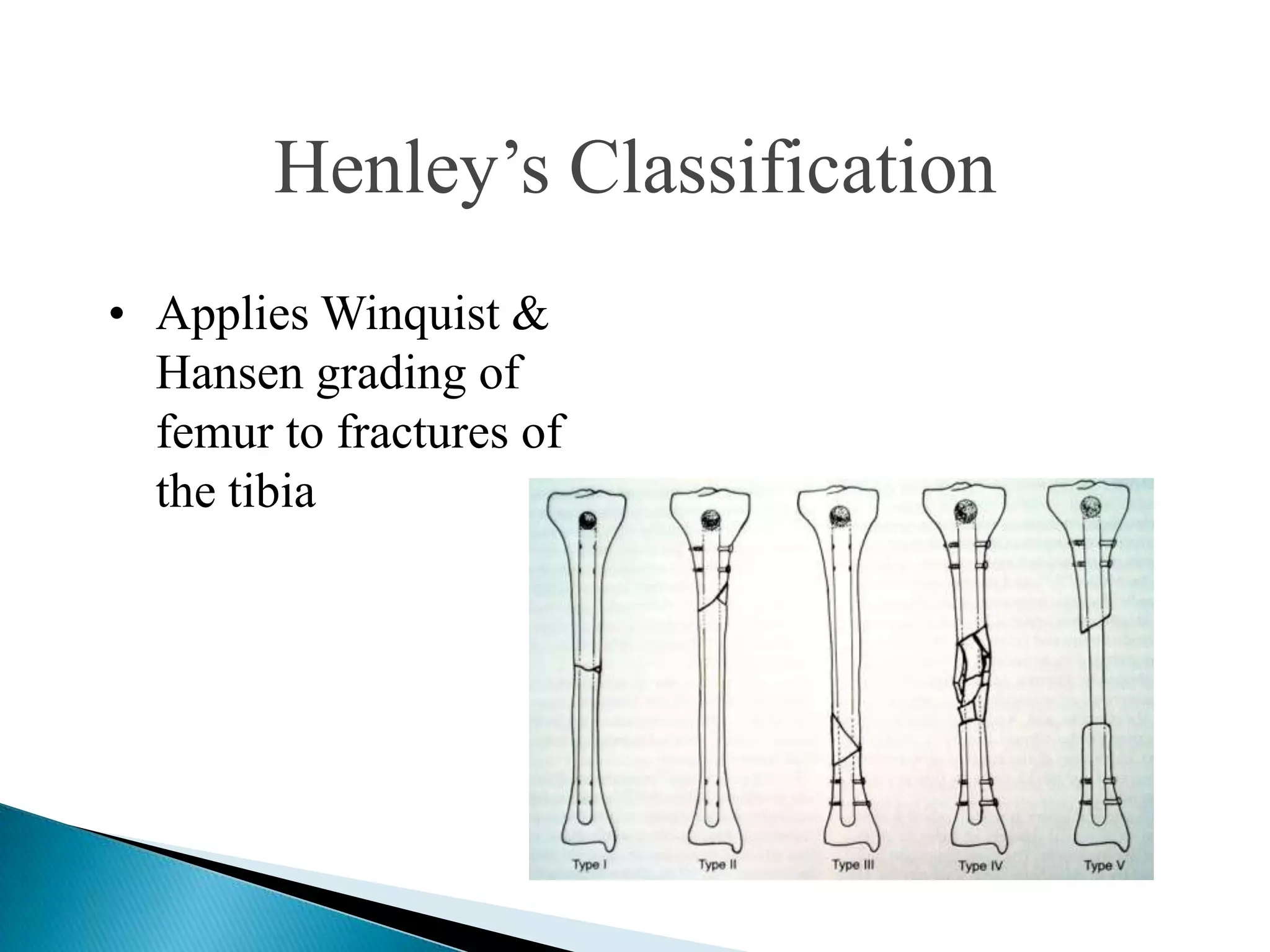
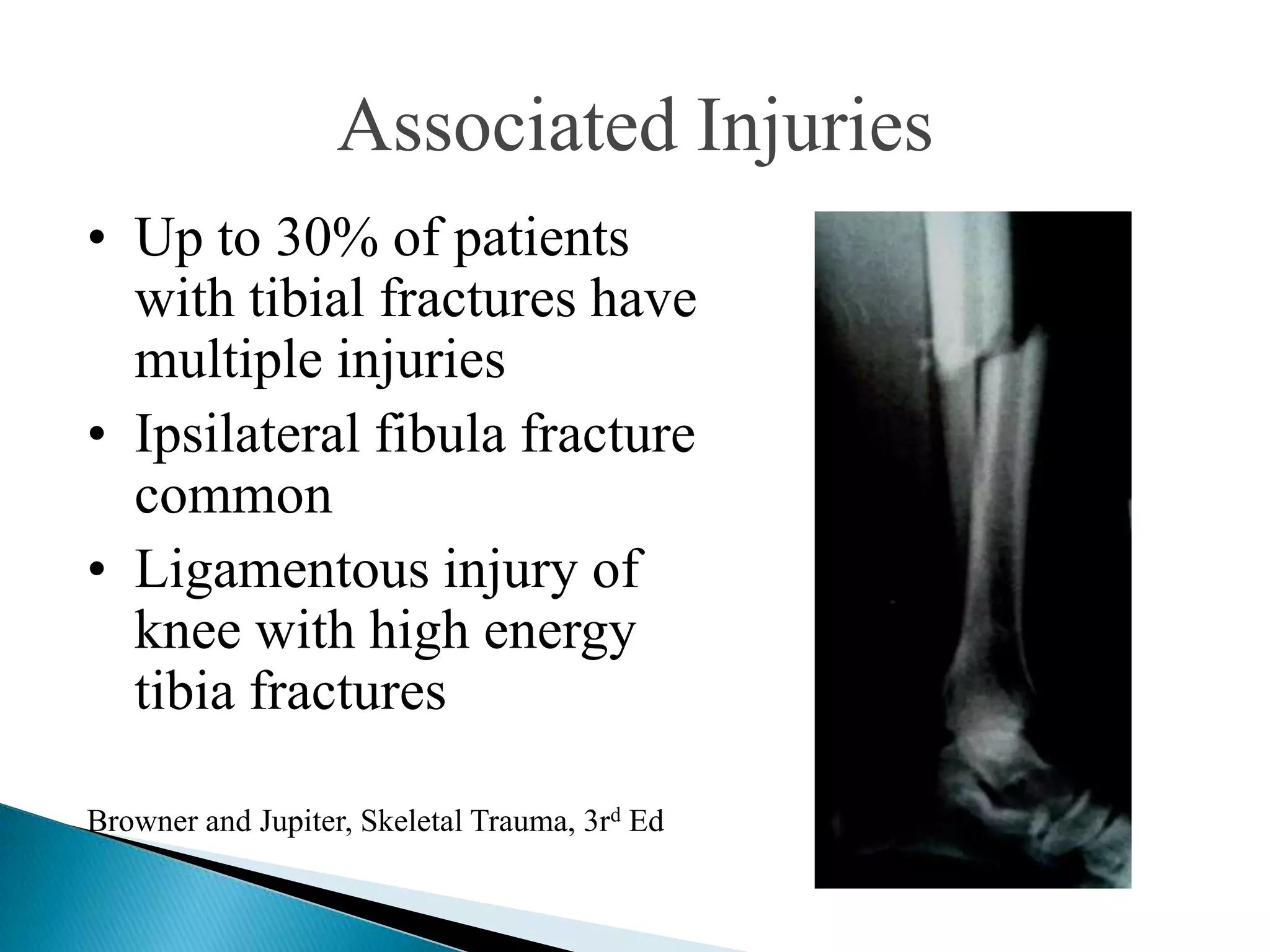
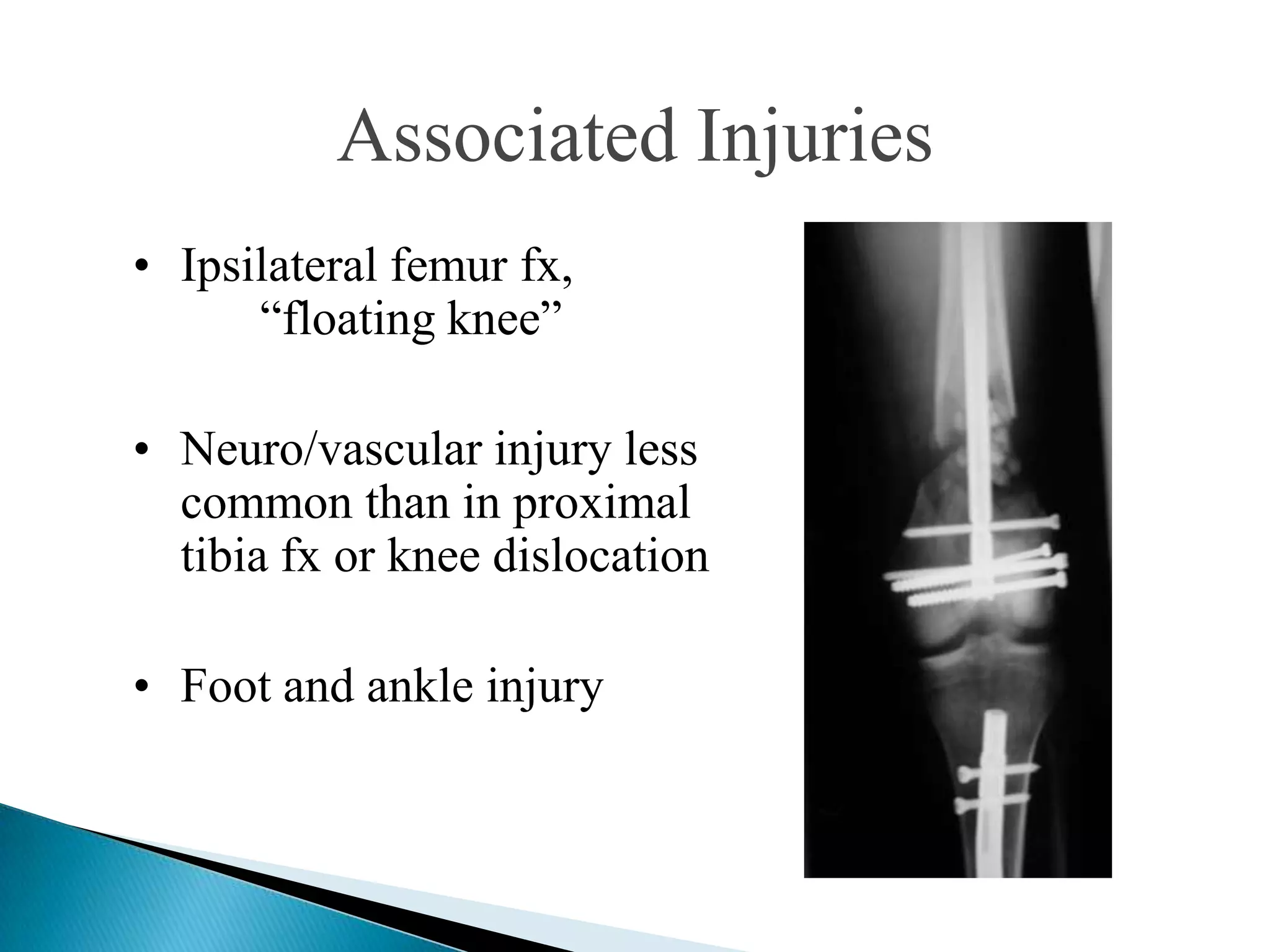
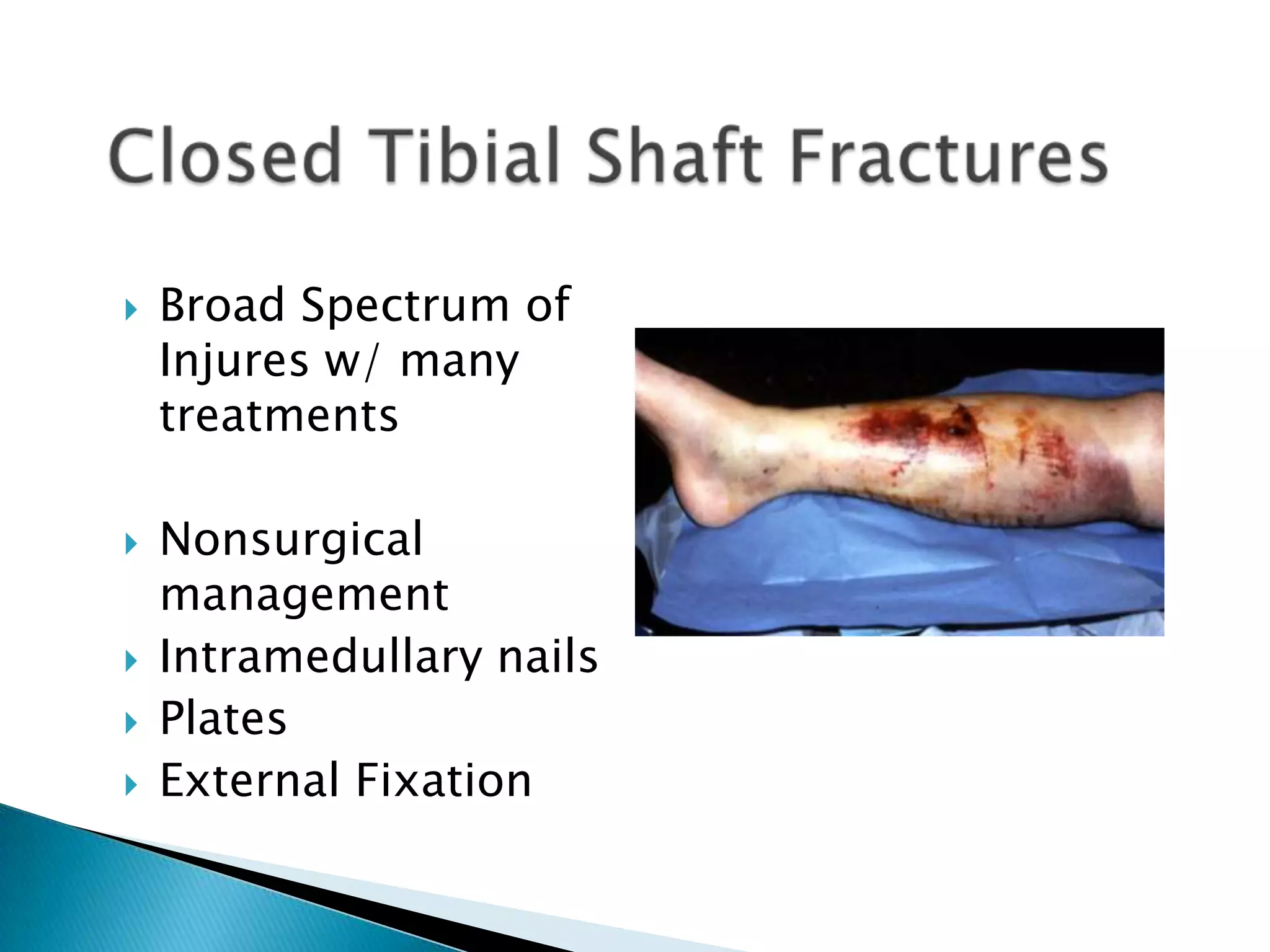
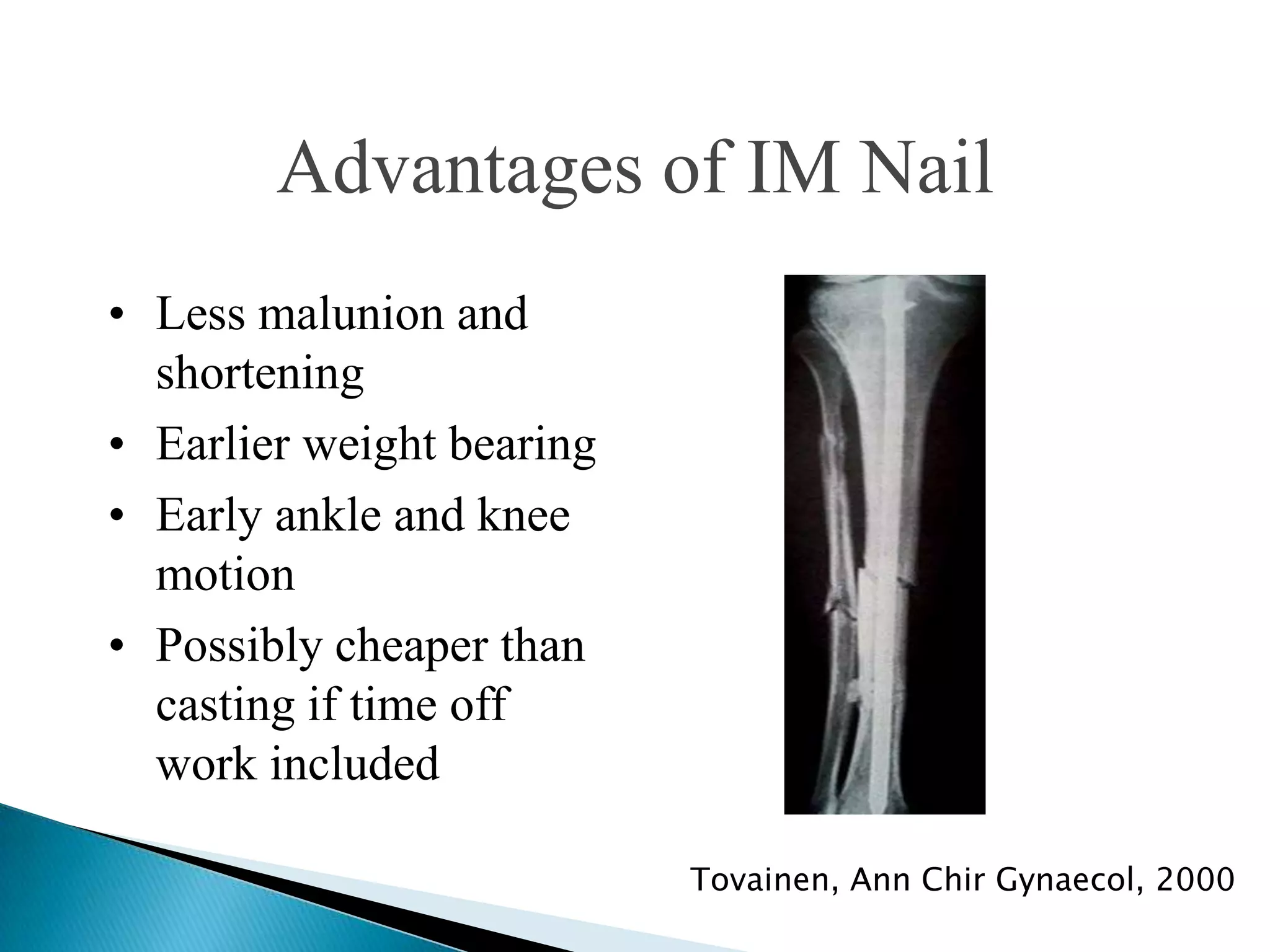
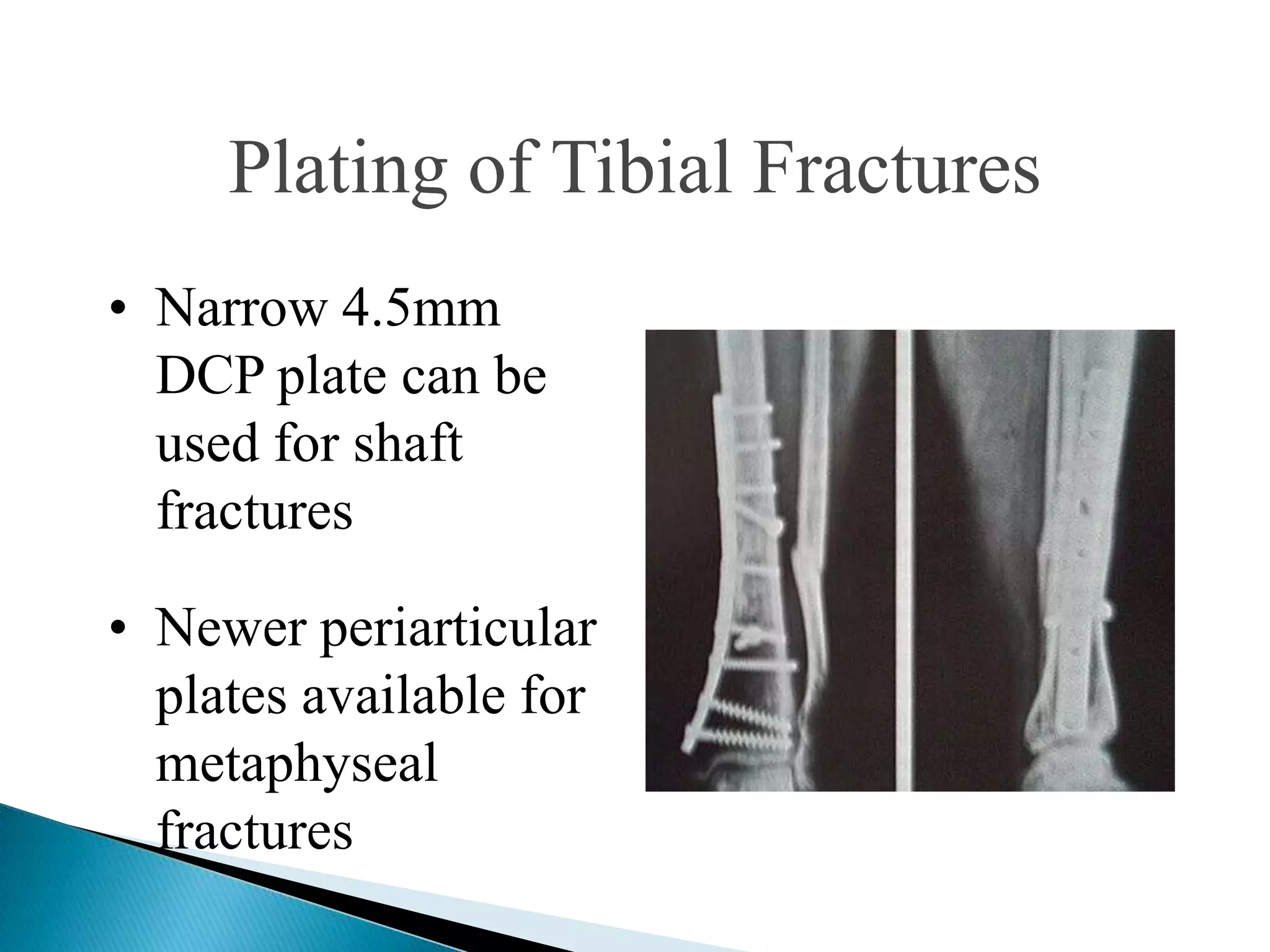
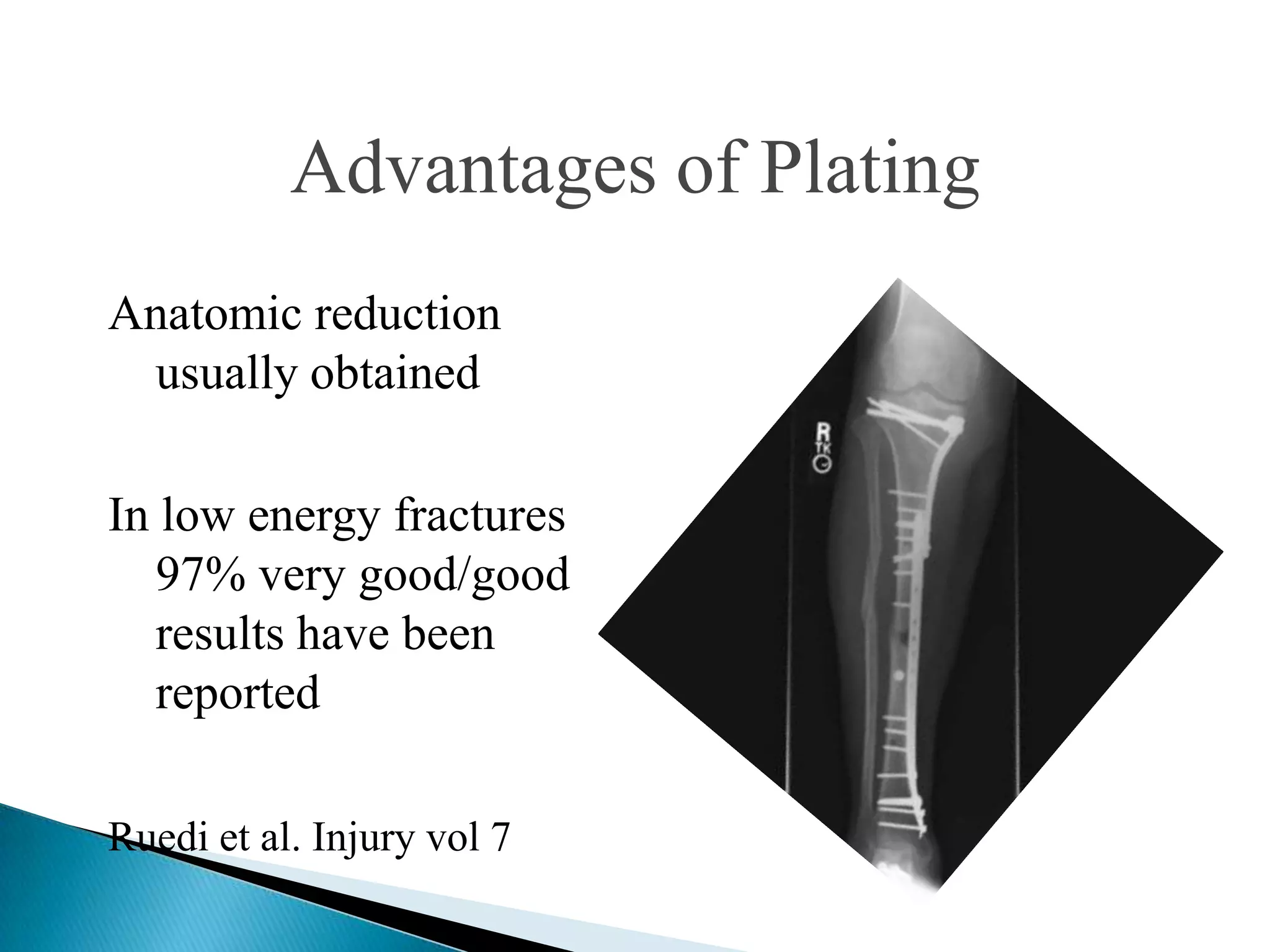
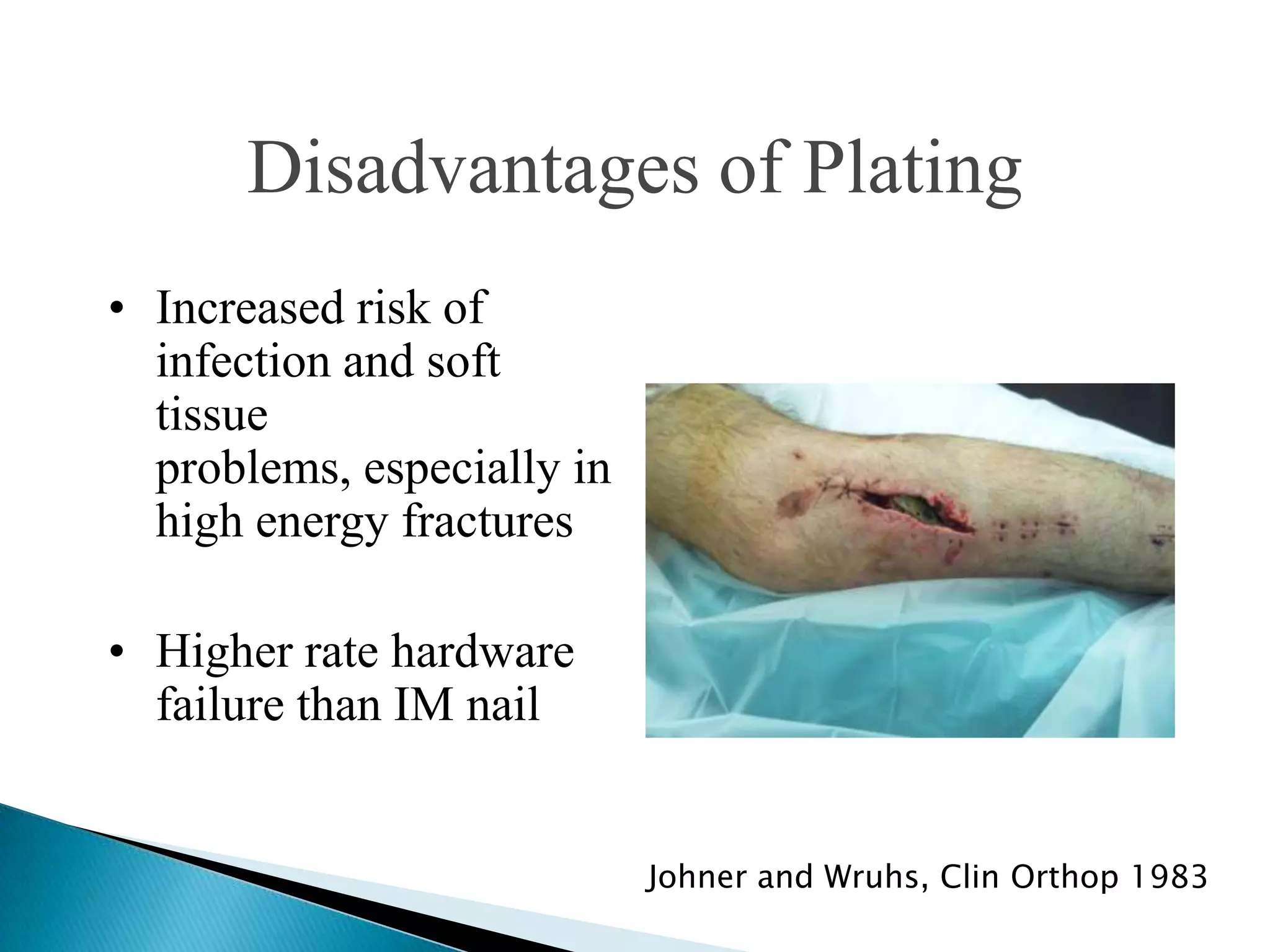
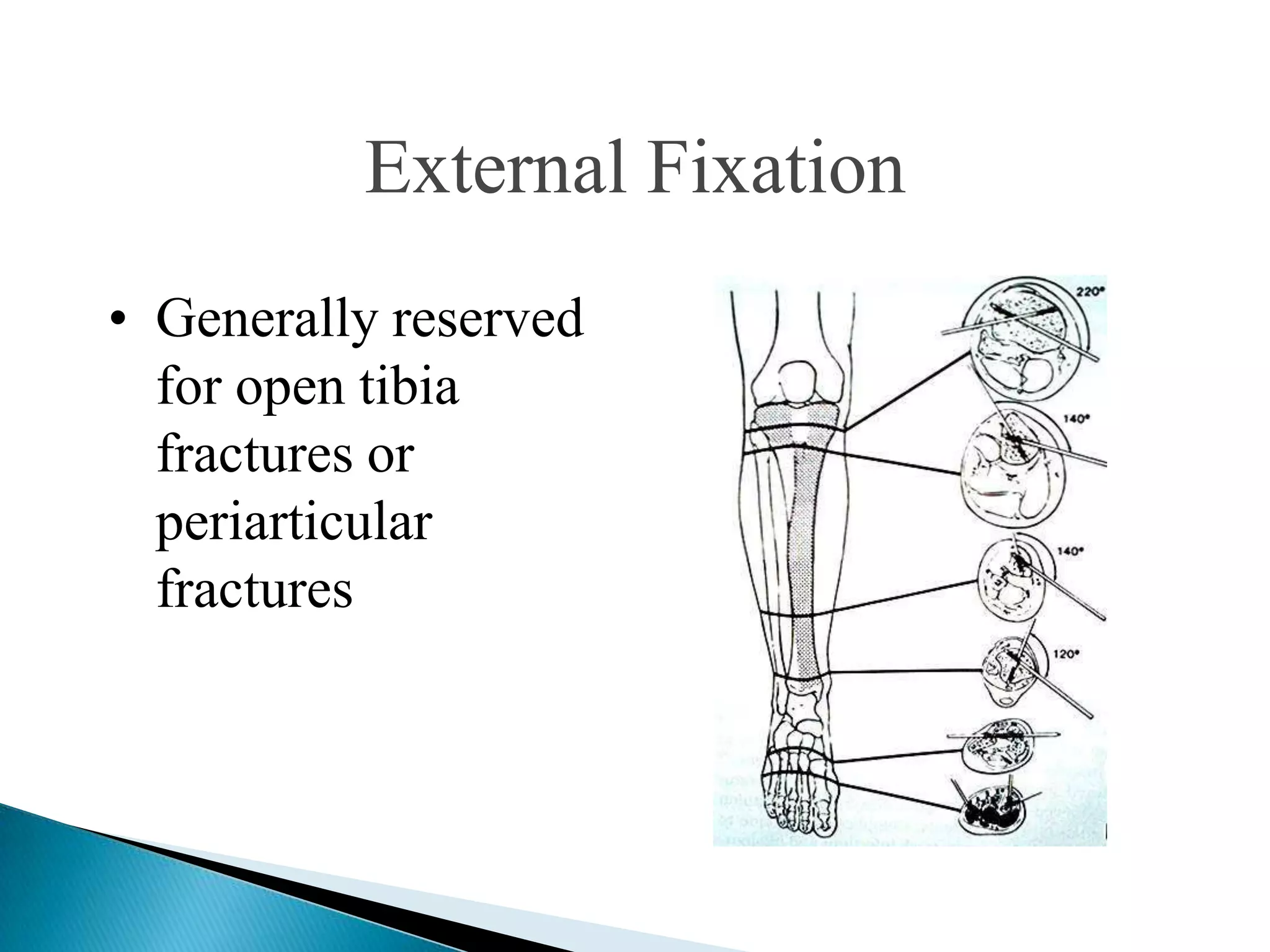
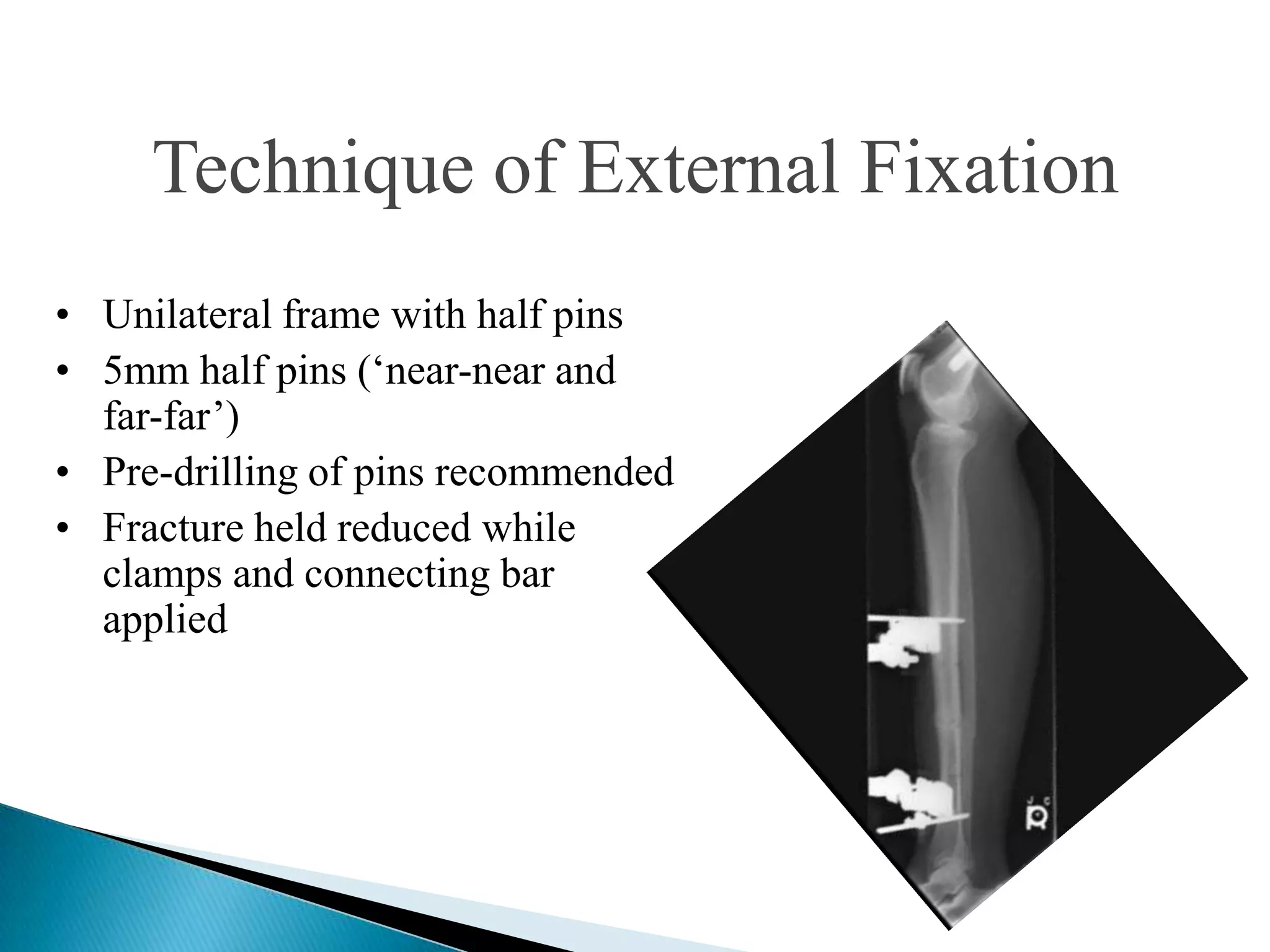
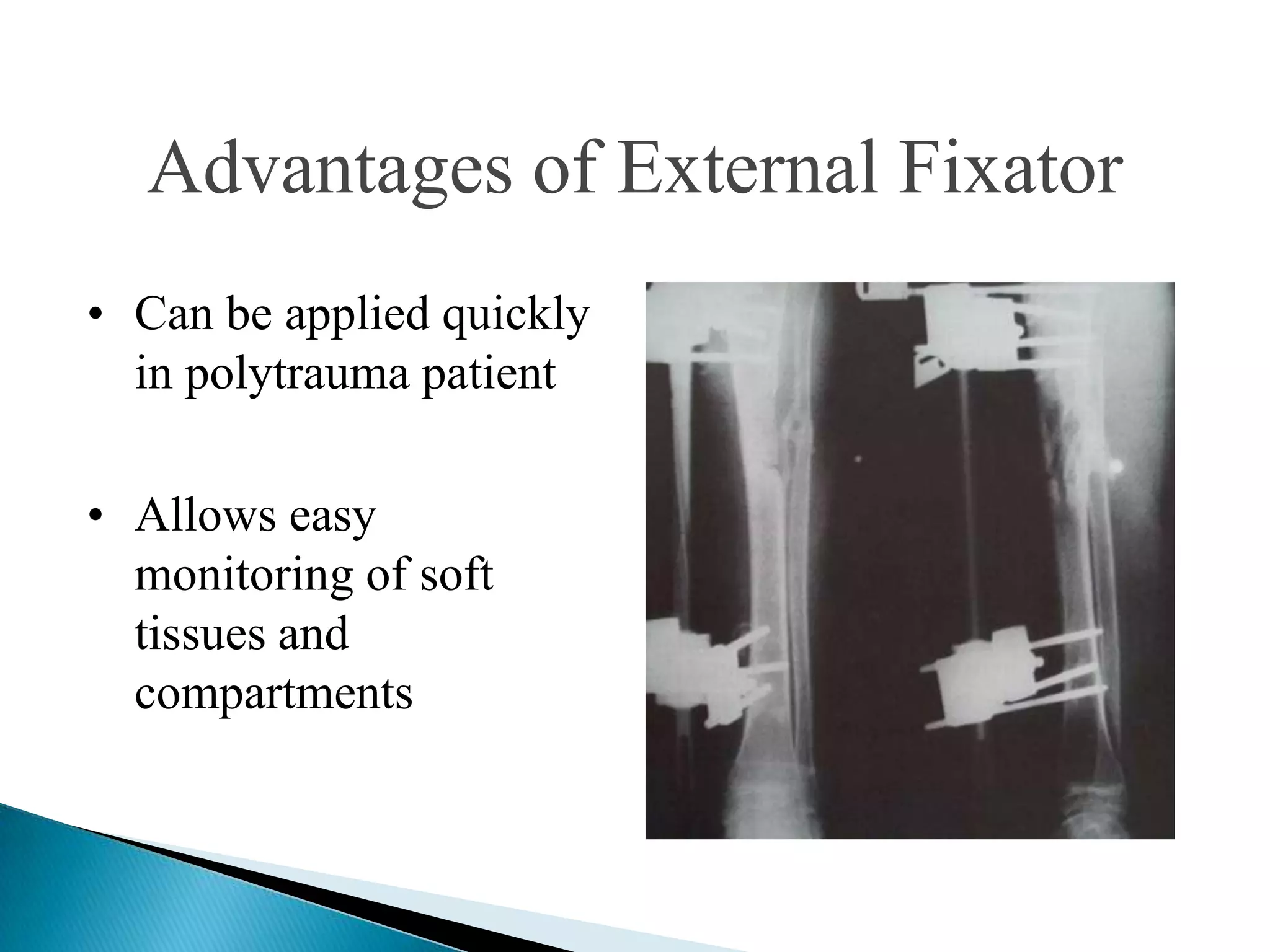
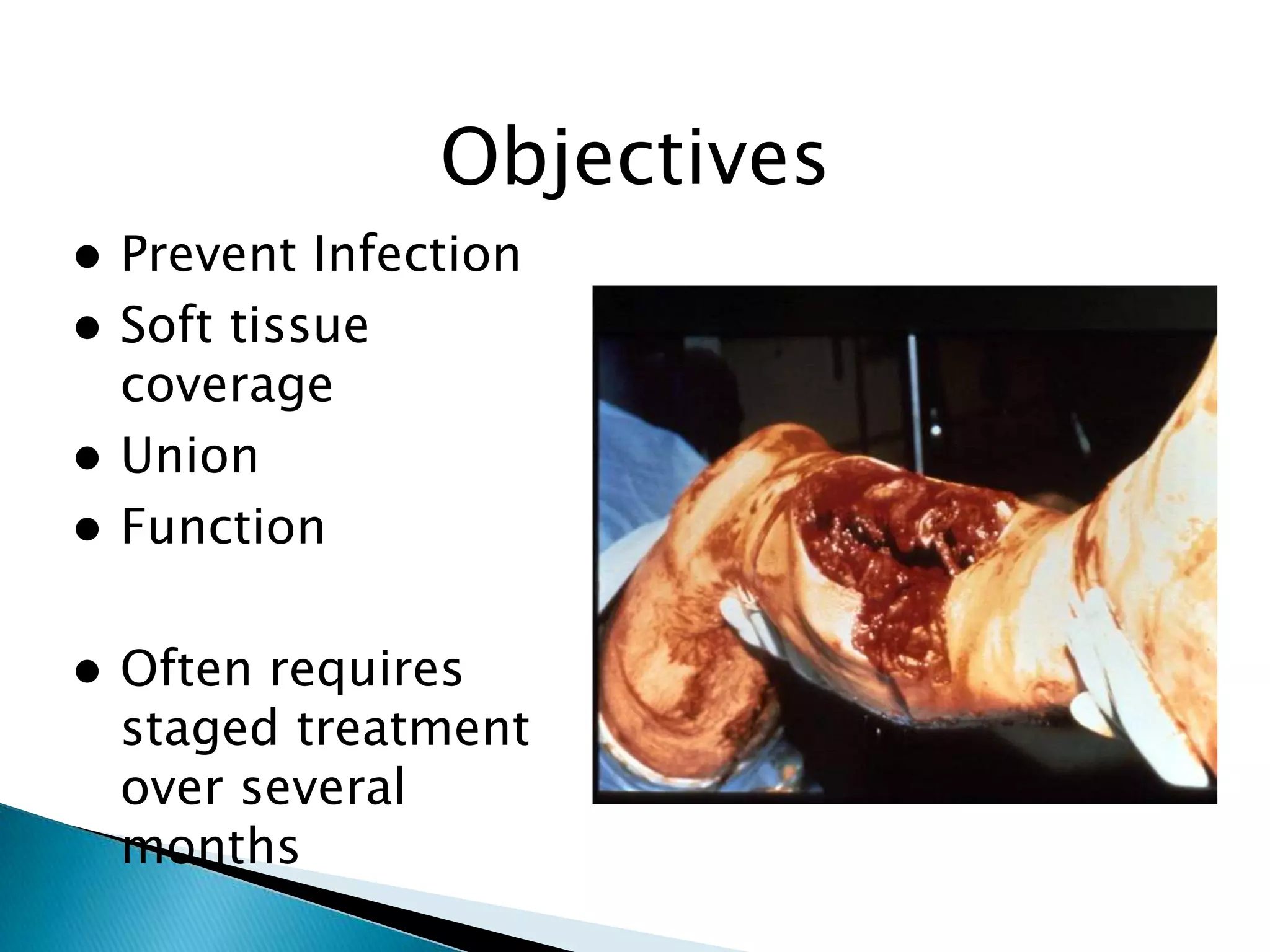
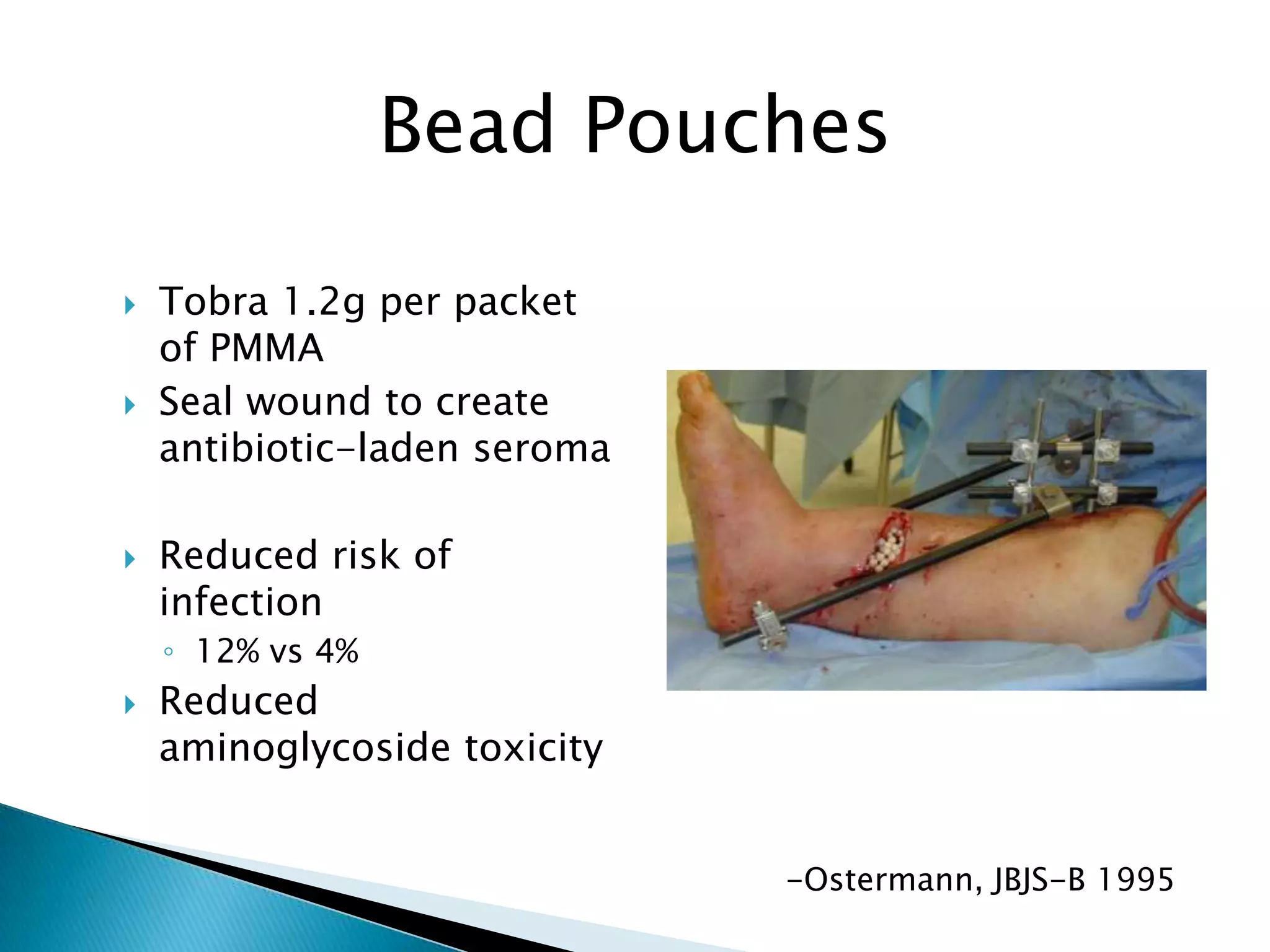
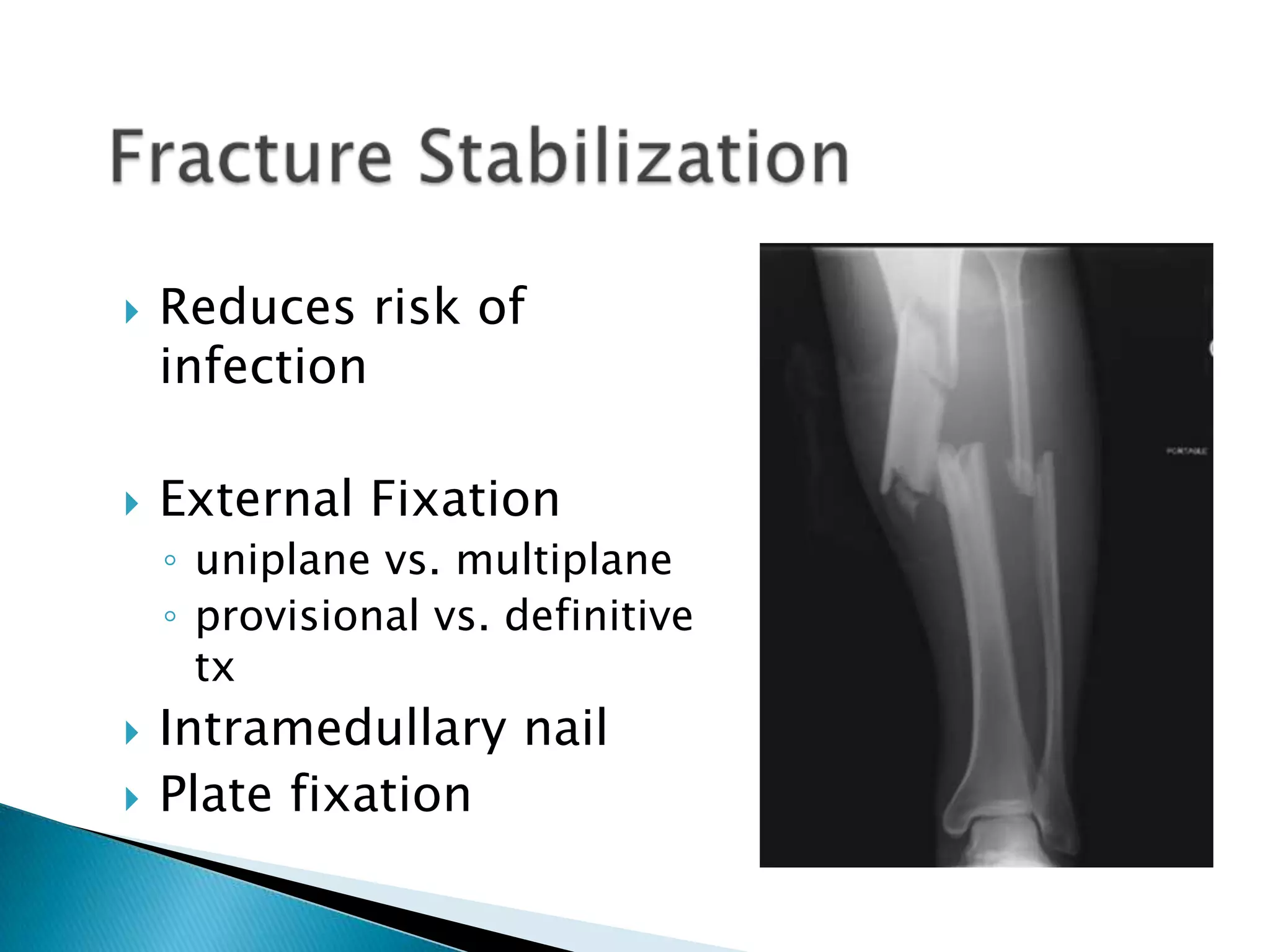
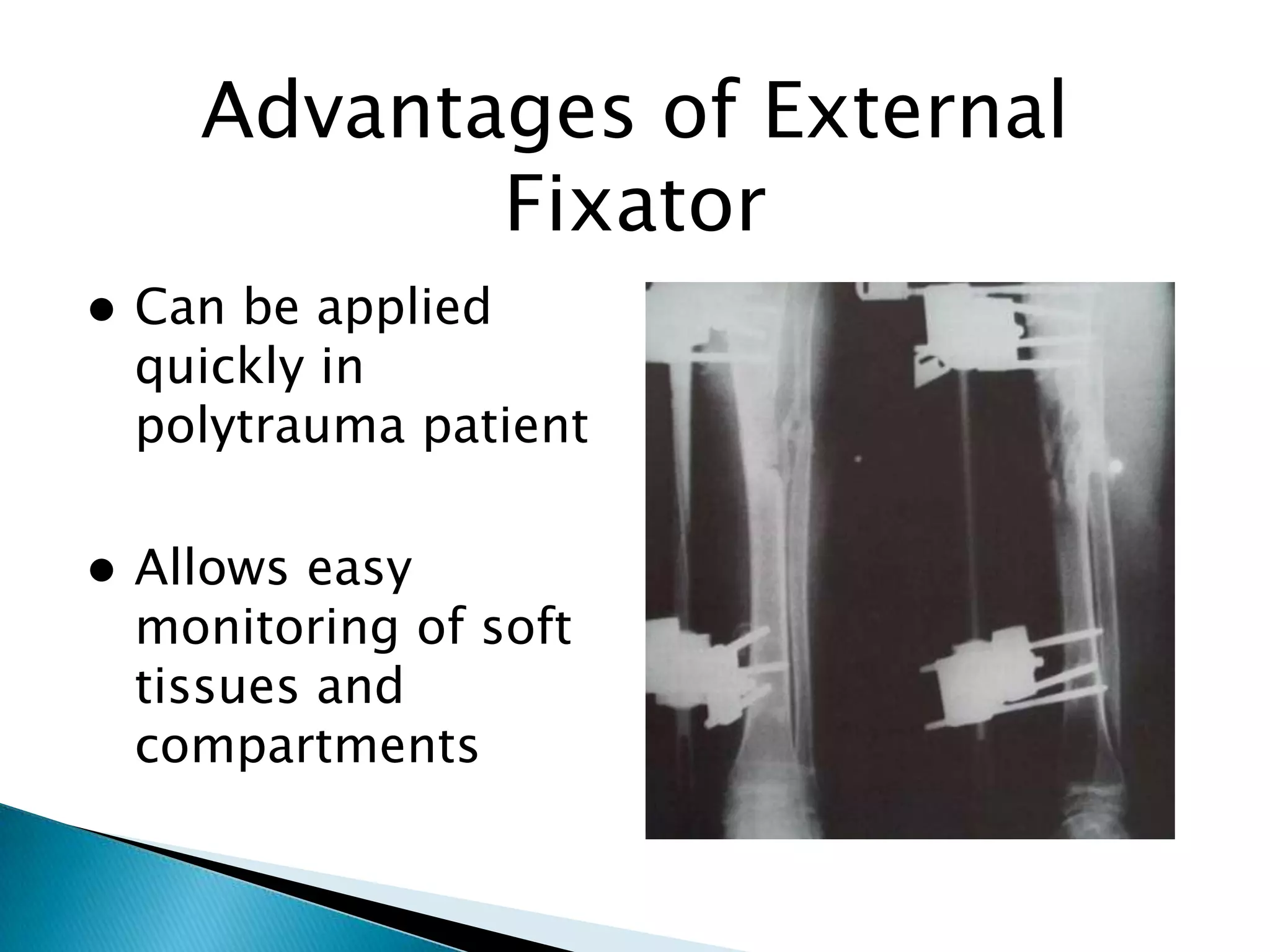
This document provides information on fractures of the tibia. It begins with definitions of fractures and their various classifications. The causes of tibial fractures include direct forces, indirect forces, twisting, bending, and pathological fractures. Fracture patterns include transverse, oblique, spiral, impacted, comminuted, and compression fractures. Treatment options for tibial fractures depend on the fracture type and include casting, intramedullary nailing, plating, and external fixation. Complications can include nonunion, malunion, infection, and hardware failure. Open fractures require urgent debridement and antibiotics to prevent infection.


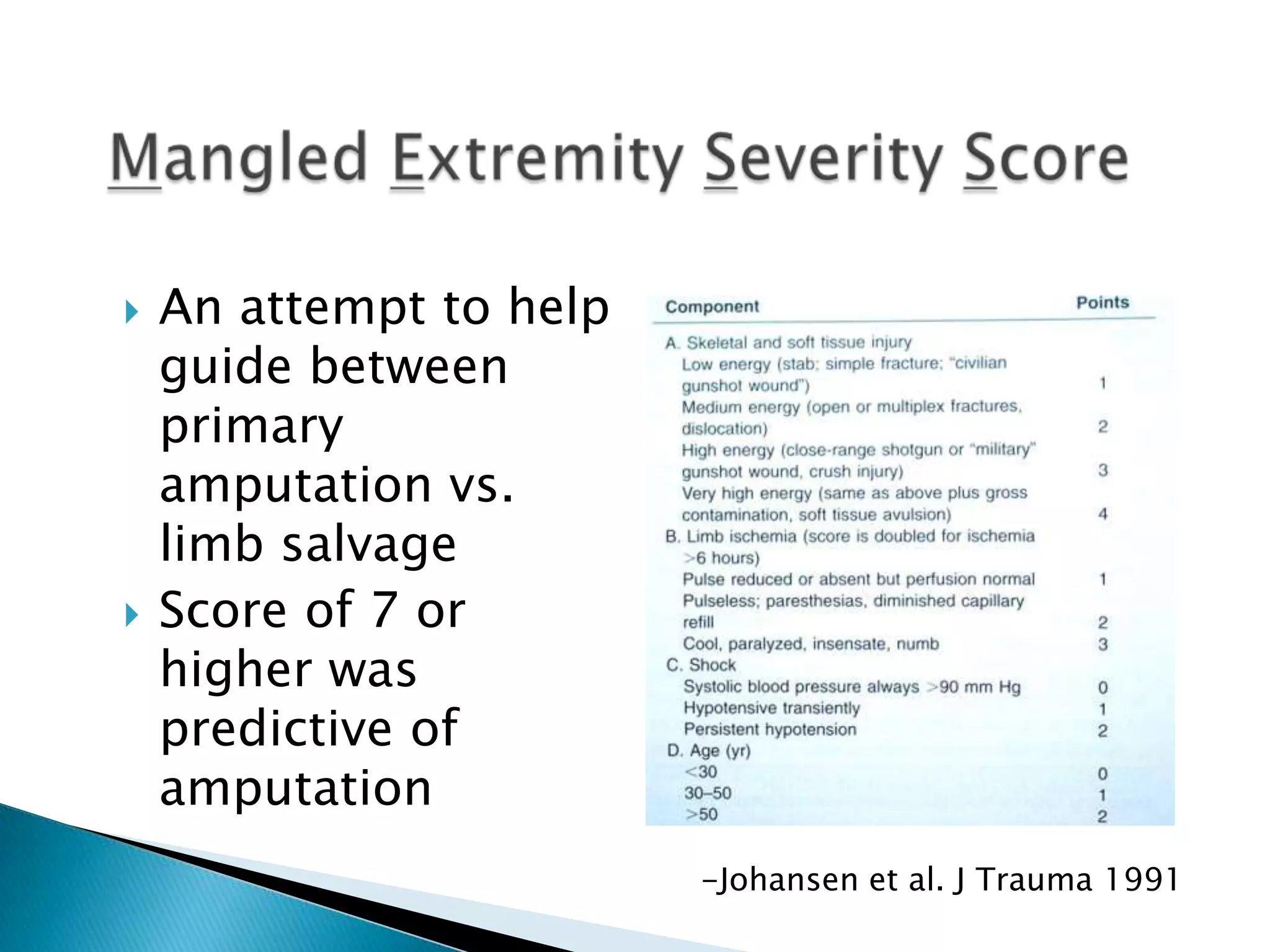
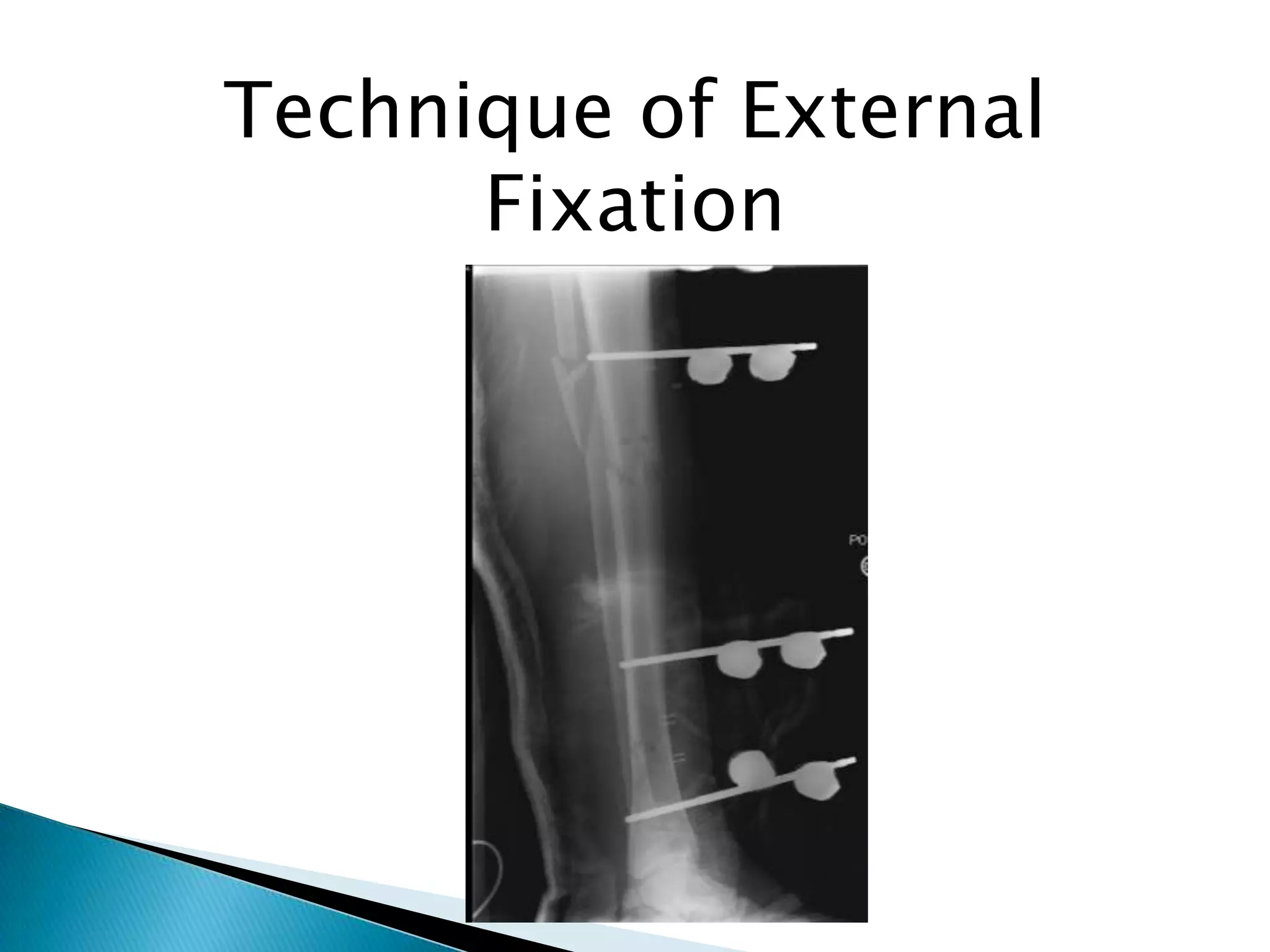
![Outcomes of External Fixation
95% union rate for
group of closed and
open tibia fractures
20% malunion rate
Loss of reduction
associated with
removing frame prior to
union
Risk of pin track
infection
Anderson et al. Clin Orthop 1974
Edge and Denham JBJS[Br] 1981](https://image.slidesharecdn.com/fracturebothboneslegclassug-131204140940-phpapp01/75/Fracture-both-bones-leg-class-ug-52-2048.jpg)
![Outcomes of External
Fixation
95% union rate for
group of closed and
open tibia fractures
20% malunion rate
Loss of reduction
associated with
removing frame
prior to union
Risk of pin track
infection
Anderson et al. Clin Orthop 1974
Edge and Denham JBJS[Br] 1981](https://image.slidesharecdn.com/fracturebothboneslegclassug-131204140940-phpapp01/75/Fracture-both-bones-leg-class-ug-63-2048.jpg)