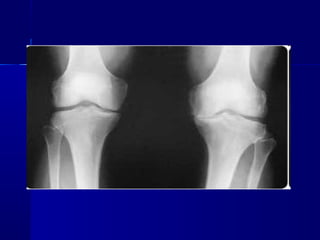
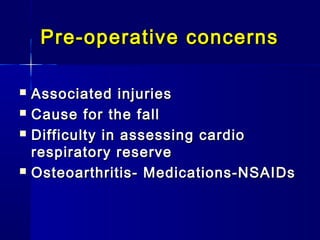
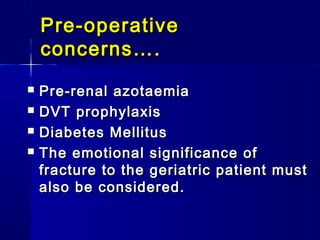
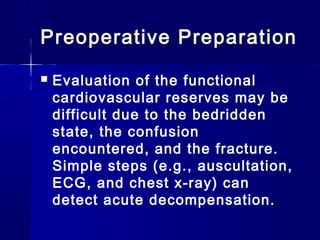
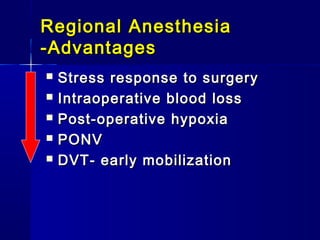
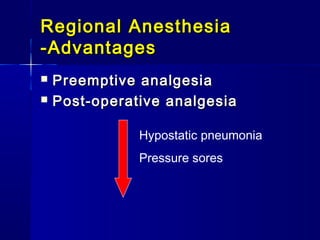
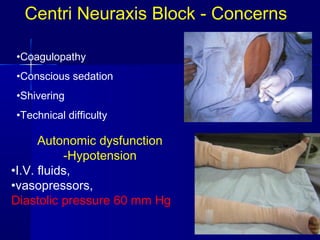
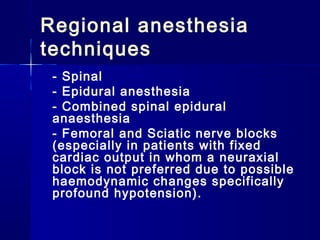
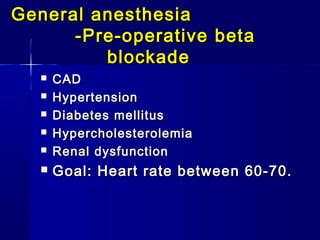
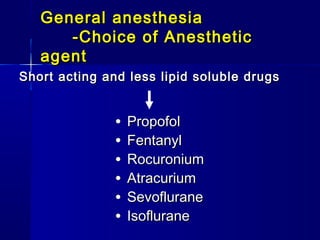
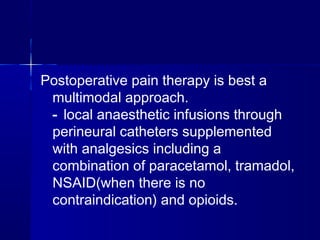
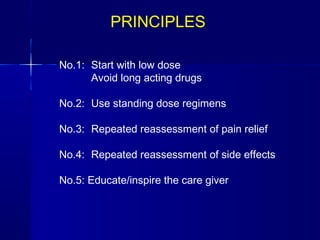
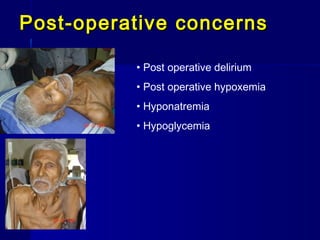
The document discusses anesthesia considerations for orthopedic joint replacement surgeries, which are commonly performed in elderly patients. It outlines various challenges in caring for geriatric patients including co-morbidities and decreased organ function. However, improvements in monitoring, techniques, analgesia, and early mobilization have led to better outcomes. The document compares regional versus general anesthesia and discusses intraoperative concerns like blood loss, hypotension from bone cement, and fat embolism. Postoperative concerns include pain, delirium, hypoxemia, and infection risk, emphasizing the need for multimodal pain control and early mobilization.