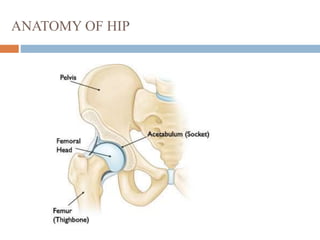
This document provides information about total hip replacement surgery. It discusses the anatomy of the hip joint, common causes of hip damage requiring replacement such as osteoarthritis and rheumatoid arthritis, and the types of surgeries and materials used including cementless fixation and metals, plastics, or ceramics. The procedure is described along with potential complications. Precautions to prevent implant failure like wound care, diet, activity restrictions and infection prevention are outlined. Regulations for hip implants in India are discussed.