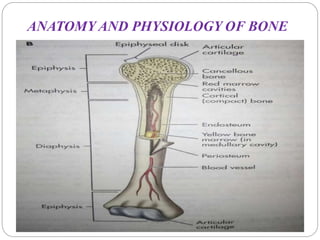
A fracture is a break or disruption in the continuity of bone. Fractures occur when stress placed on a bone exceeds its strength, and can be caused by direct impact, twisting, compression or muscle contraction. There are many types of fractures classified by the bone location and nature of the break. Treatment depends on the type and severity of fracture, and may involve casting, traction, closed or open reduction, internal or external fixation to realign and immobilize the bone while it heals. Nursing care focuses on pain management, preventing complications like infection, and helping the patient regain mobility and function.