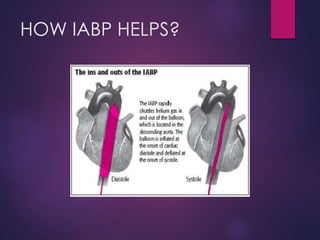
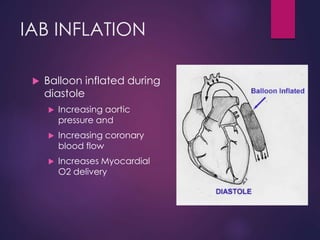
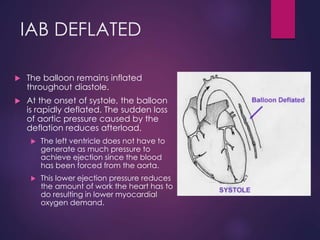
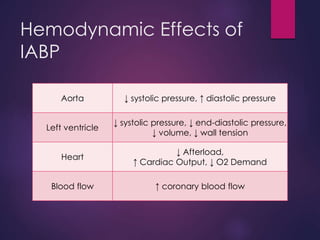
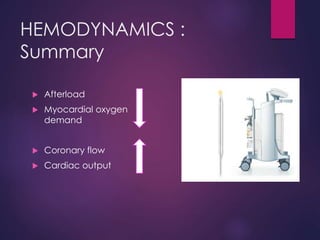
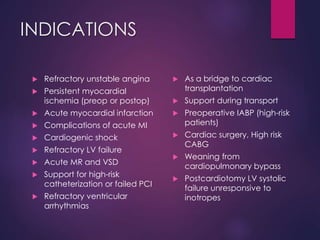
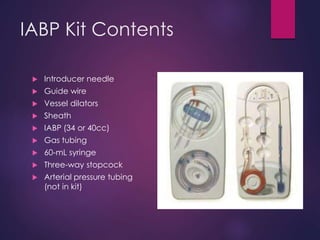
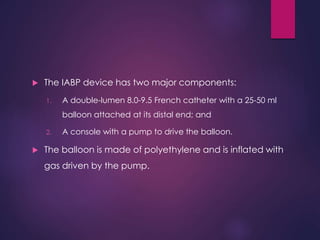
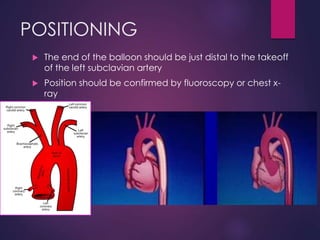
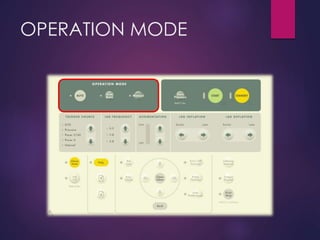
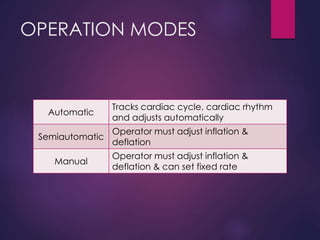
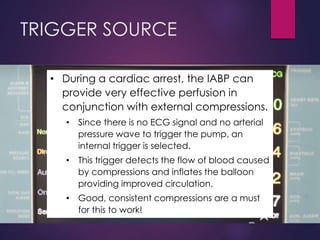
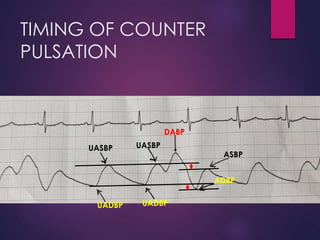
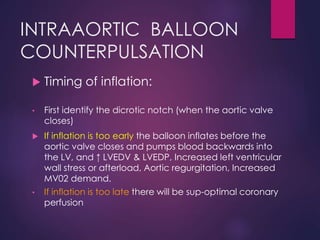
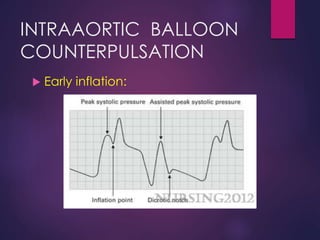
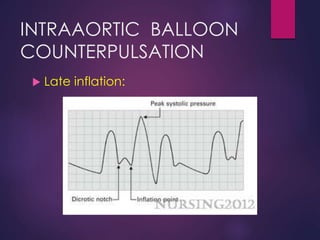
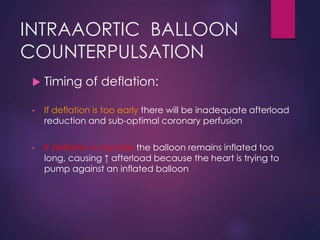
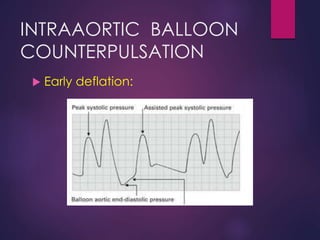
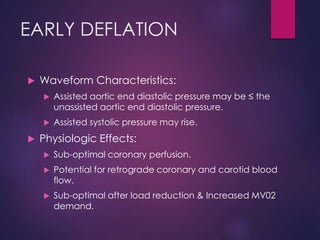
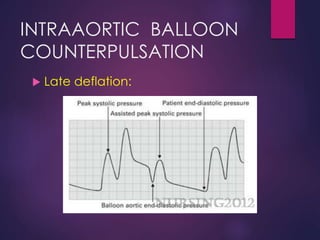
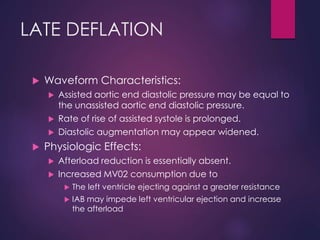
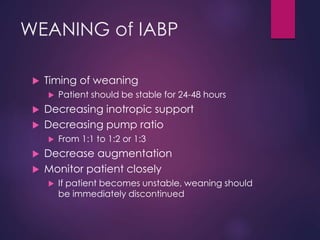
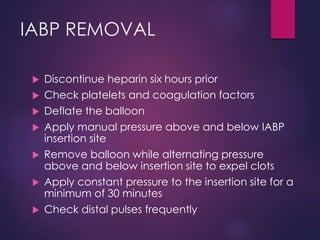
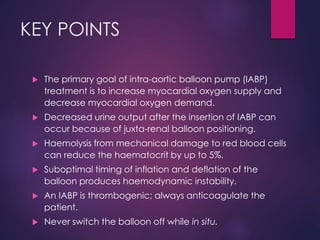
The document provides a comprehensive overview of intra-aortic balloon counterpulsation (IABP), detailing its historical development, physiological principles, mechanisms of action, indications, contraindications, and potential complications. It explains how IABP enhances coronary blood flow and decreases myocardial oxygen demand through precisely timed inflation and deflation of a balloon catheter positioned in the aorta. The document also outlines operational techniques, maintenance care, and weaning procedures for the effective and safe use of IABP in clinical settings.