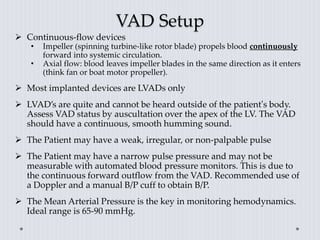
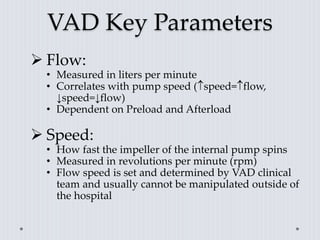
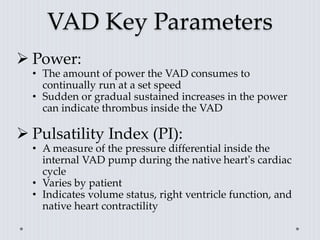
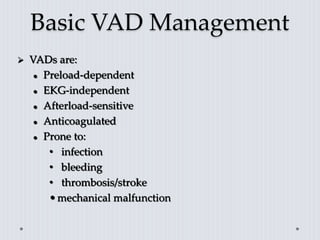
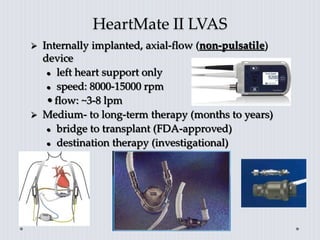
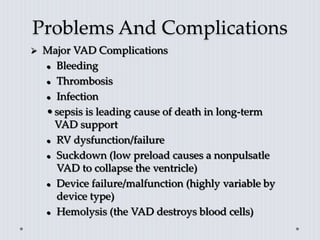
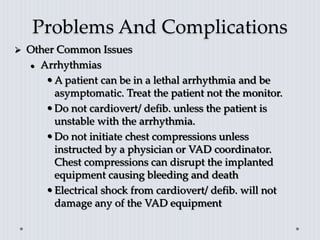
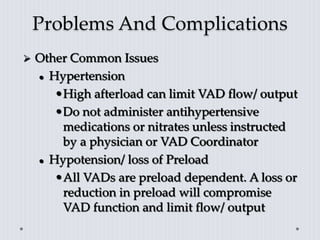
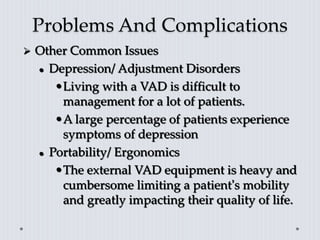
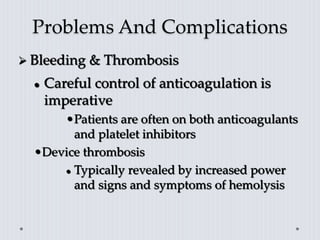
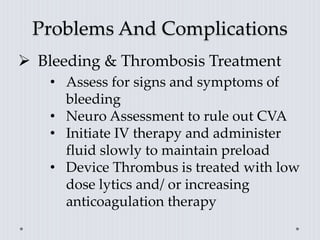
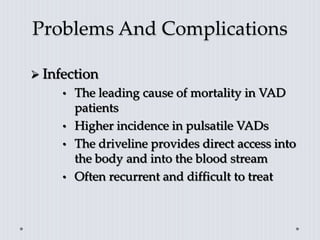
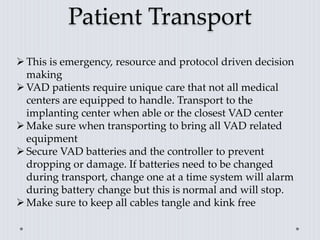
A ventricular assist device (VAD) is a mechanical pump that is surgically implanted to assist one or both failing ventricles of the heart. It helps pump blood to the body when the heart is too weak. Complications can include bleeding, infection, device malfunction. Proper management focuses on maintaining adequate blood volume and flow through the device. Transporting VAD patients requires bringing all equipment and contacting the implanting center for guidance.