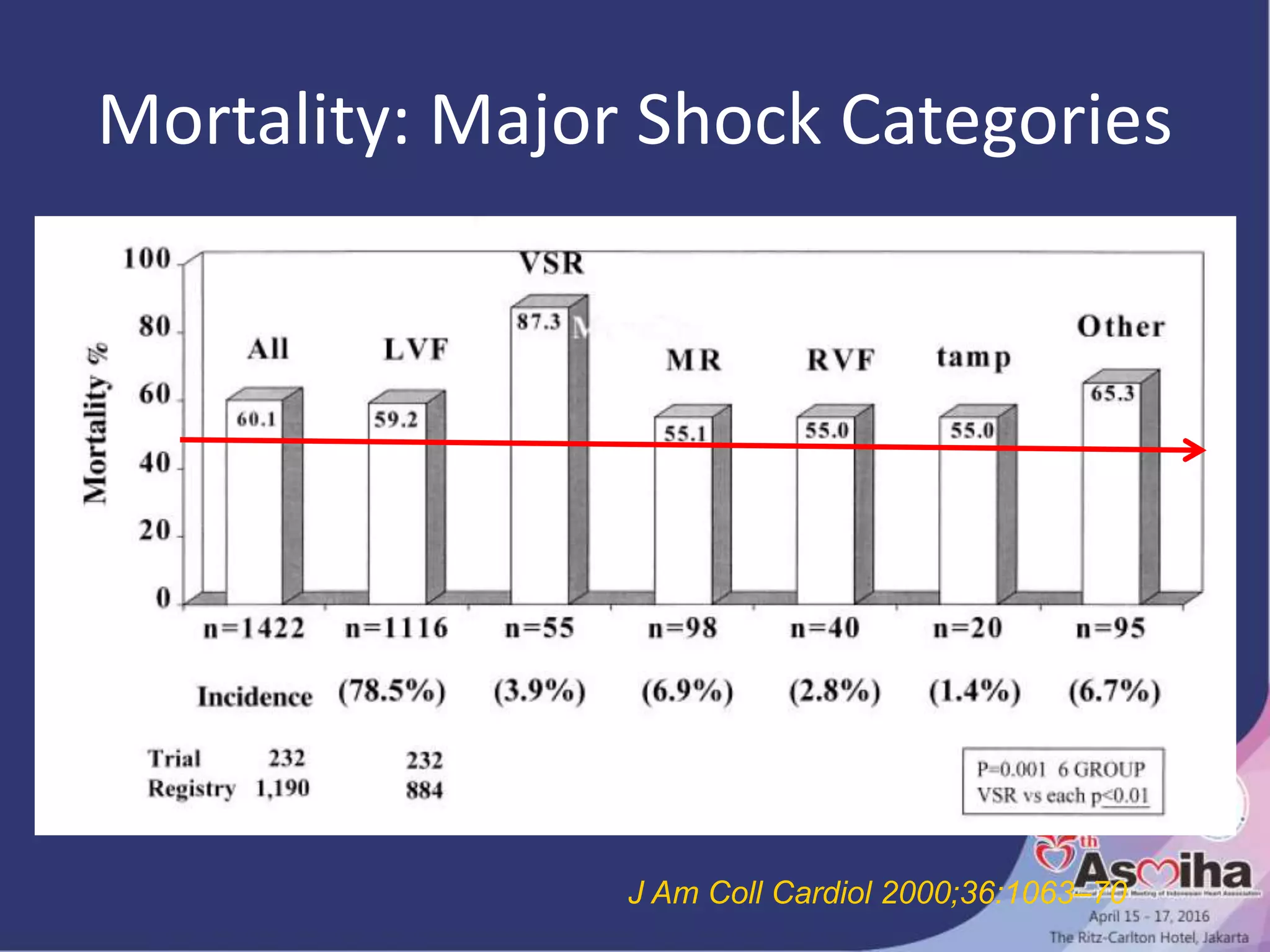
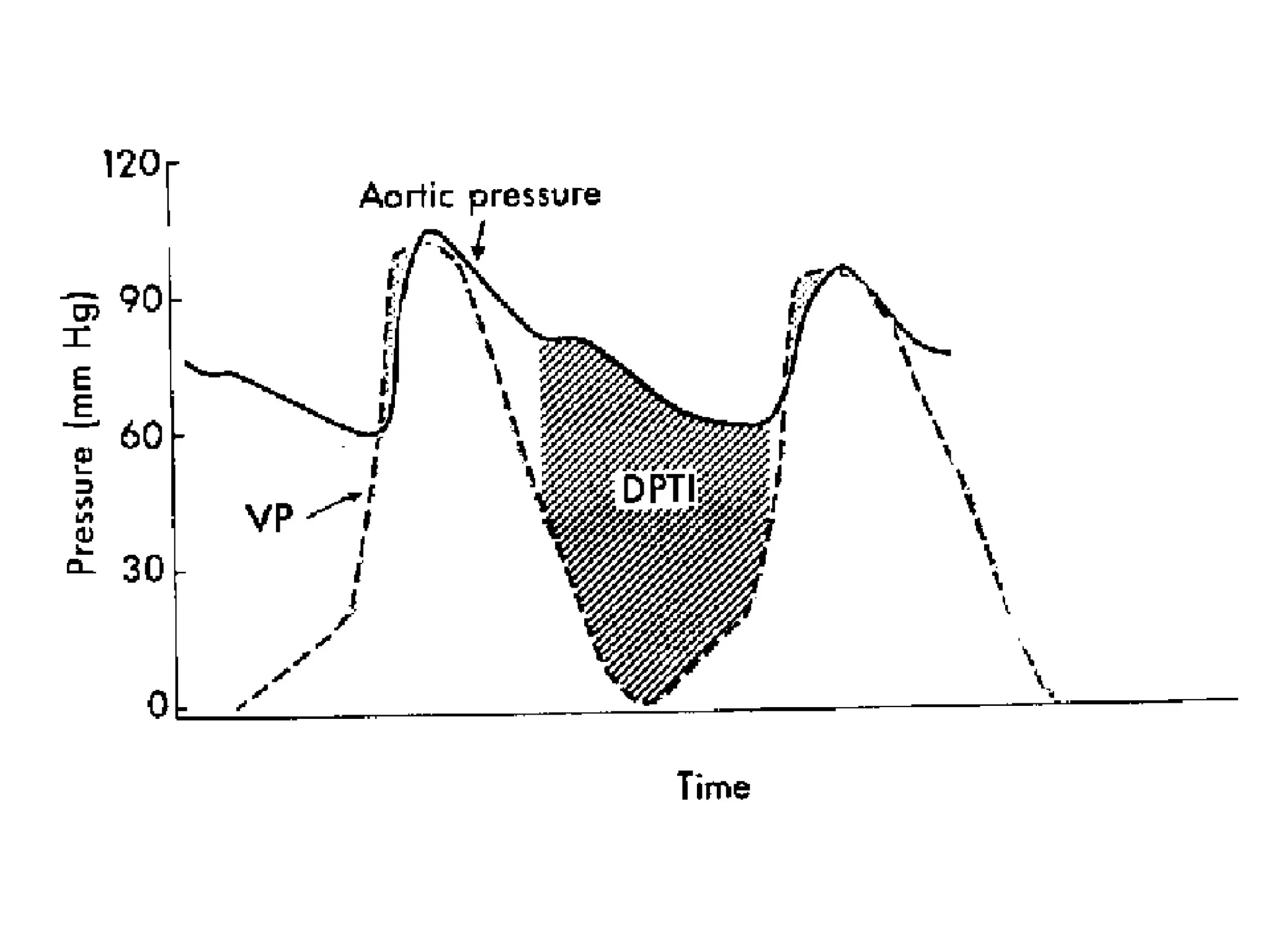
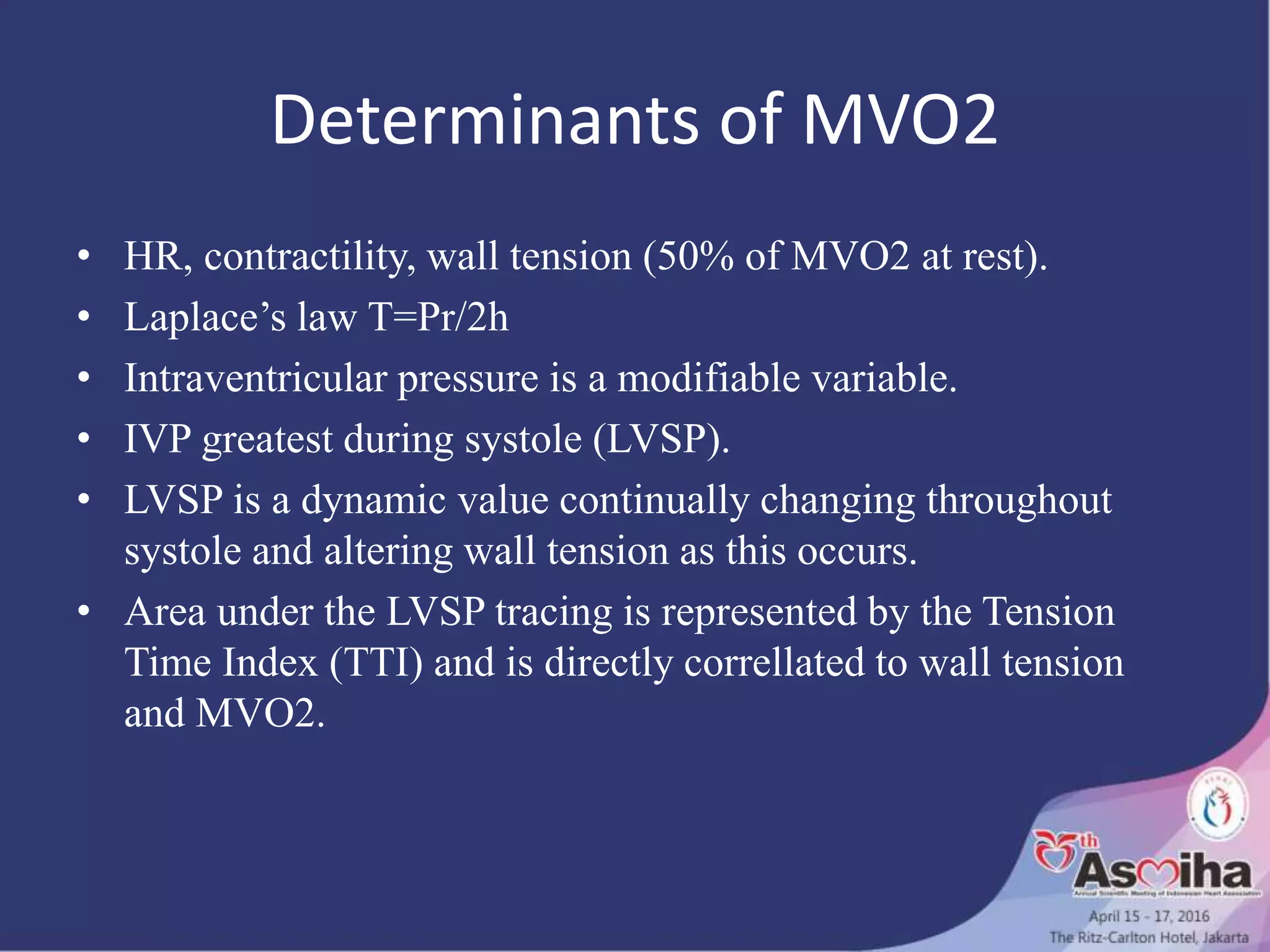
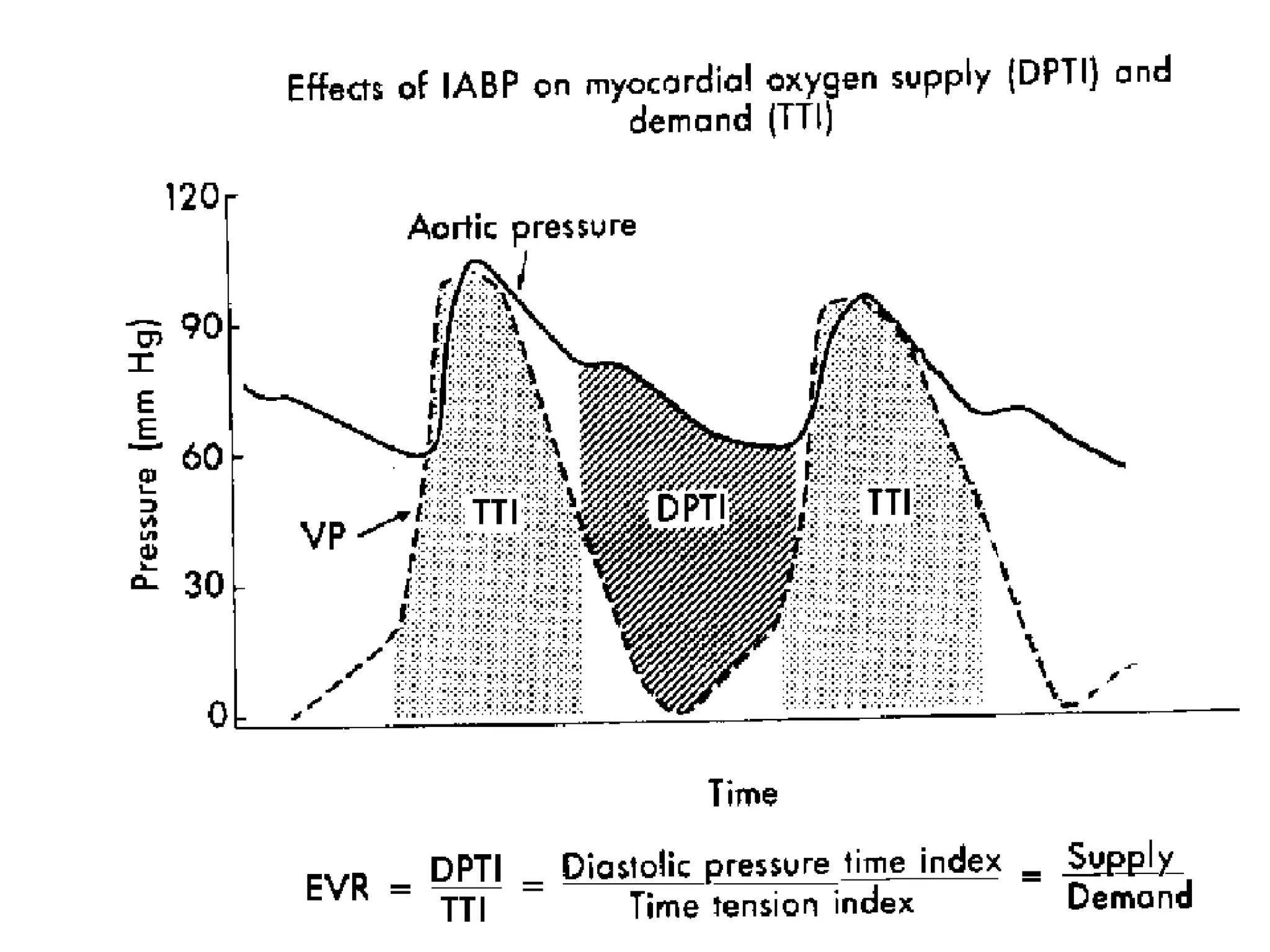
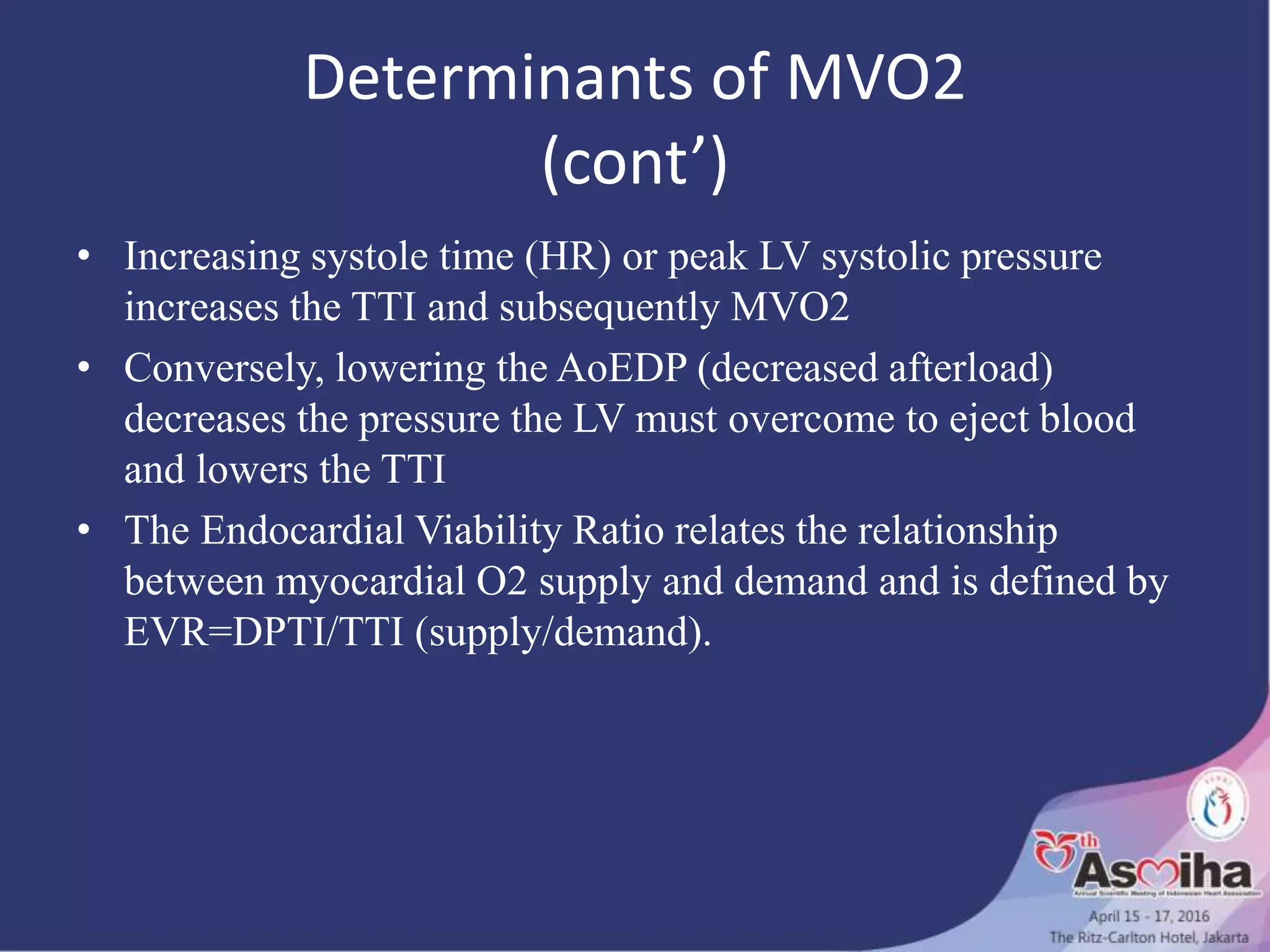
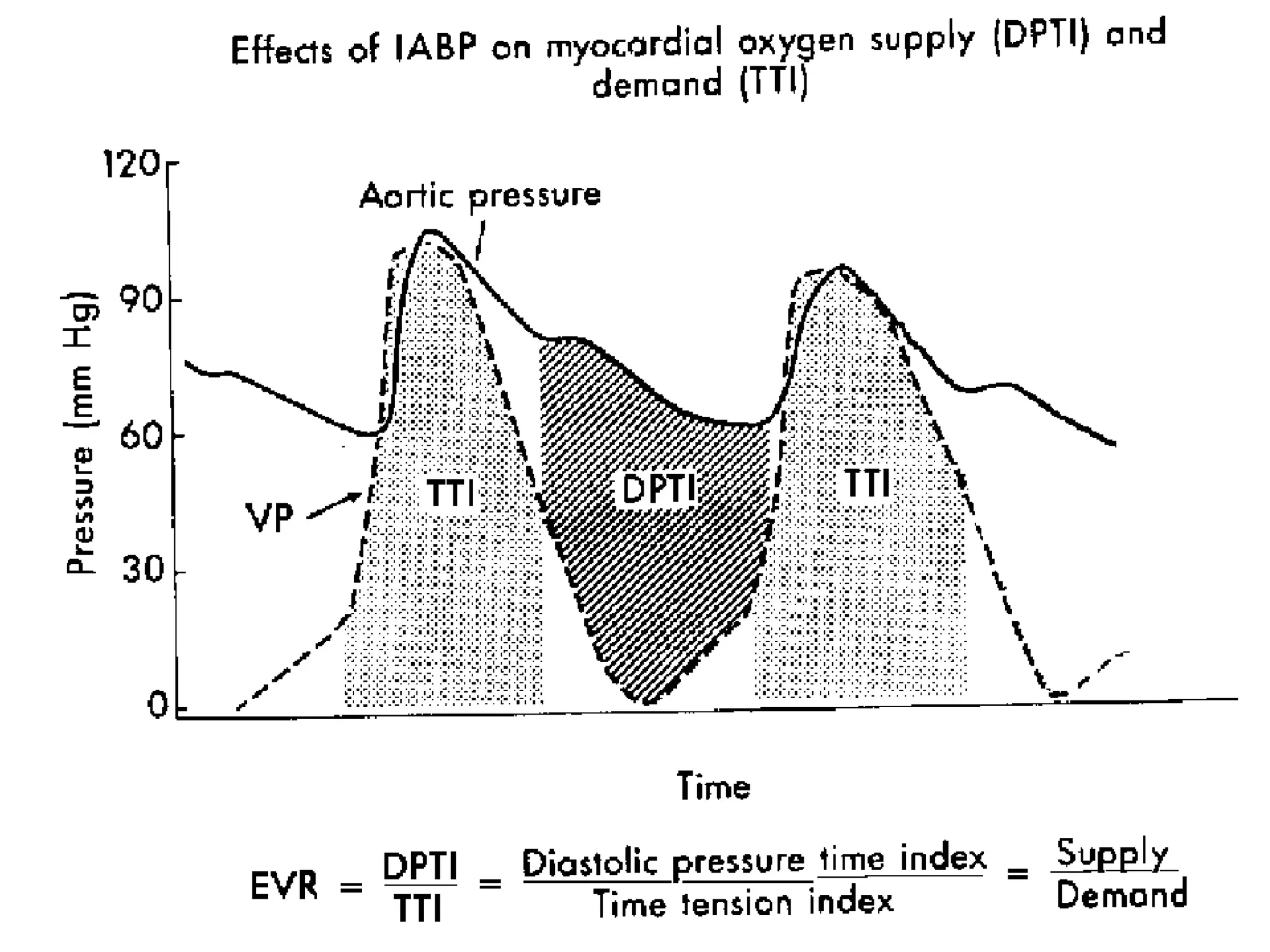
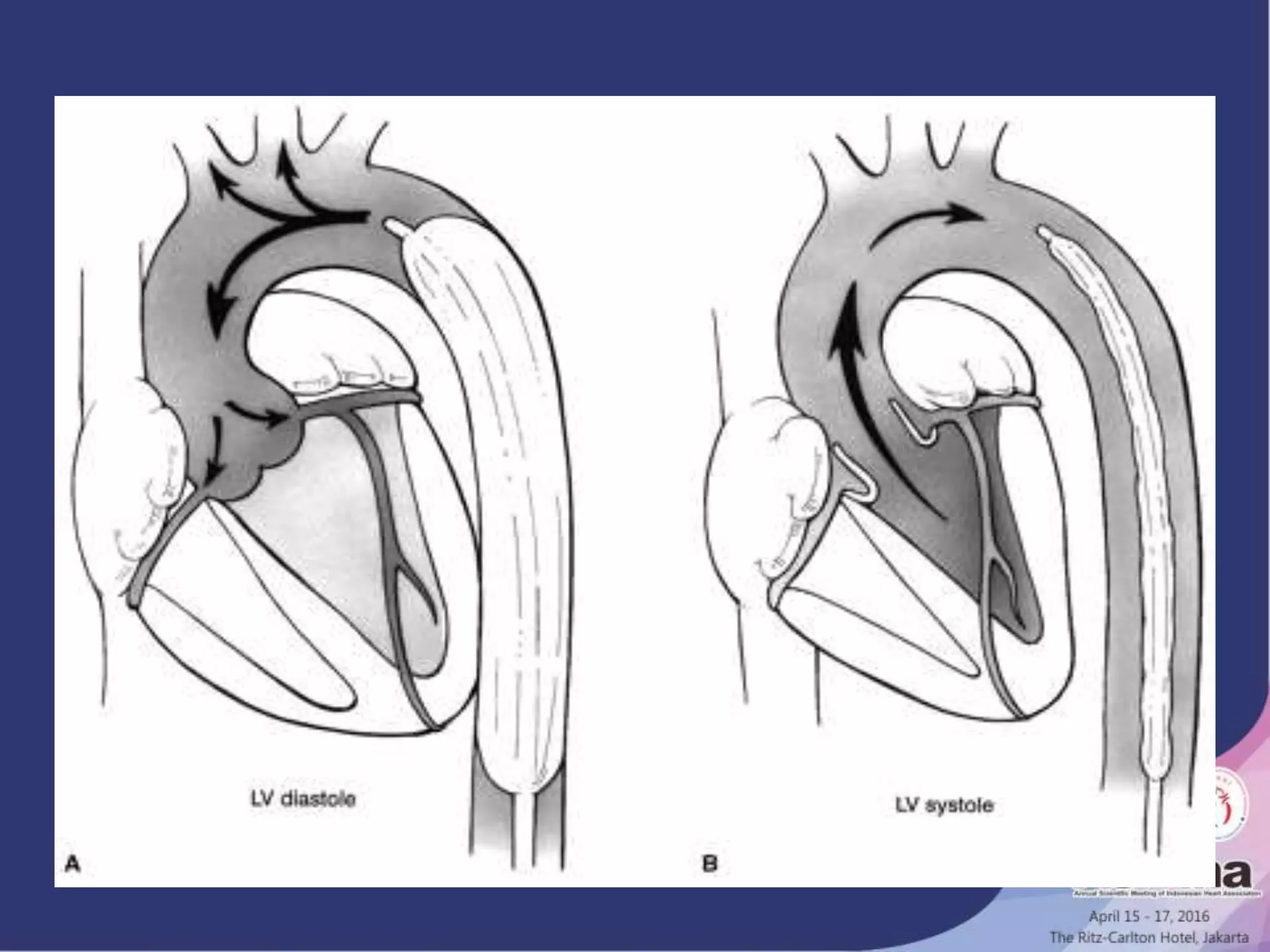
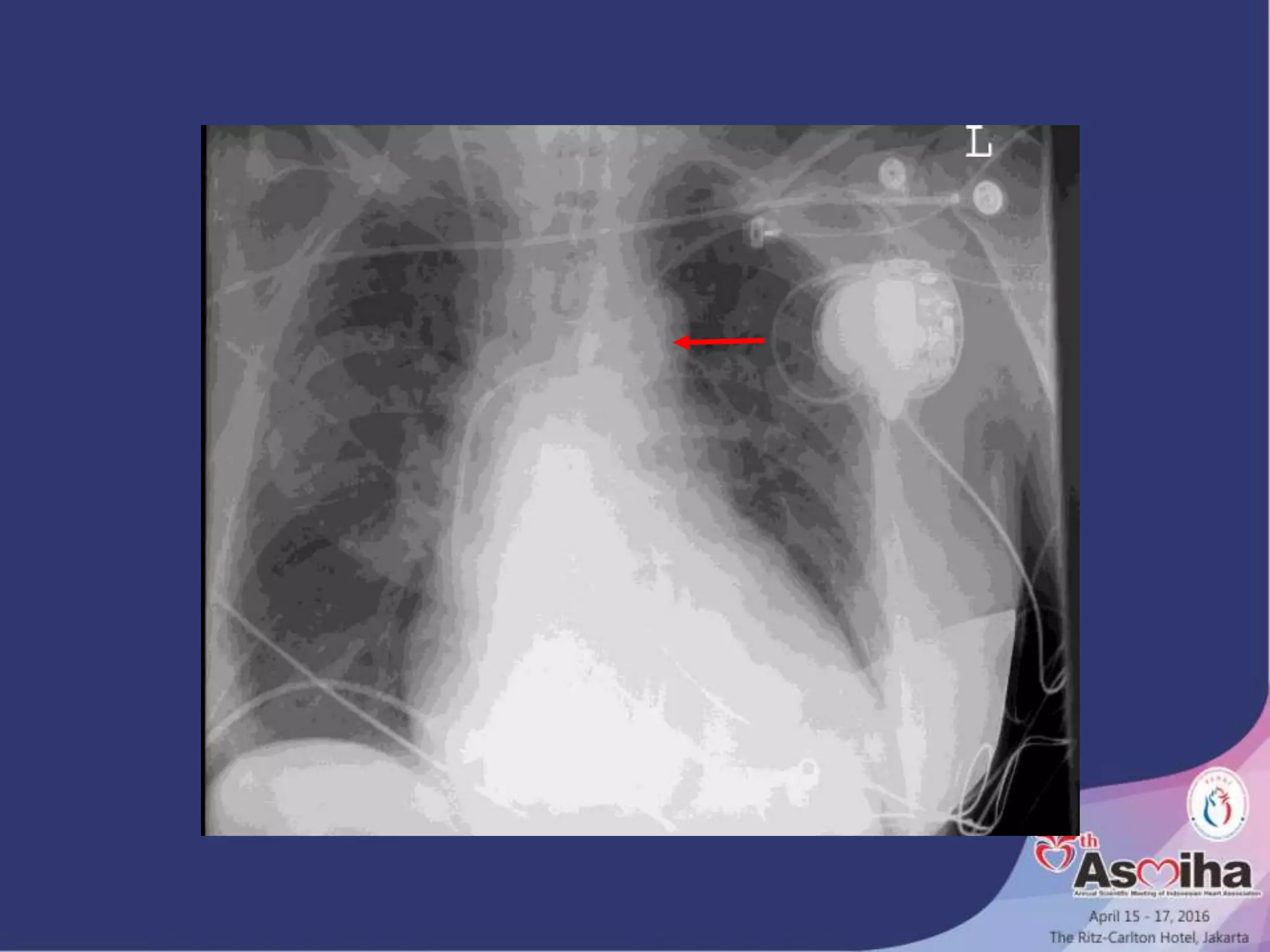
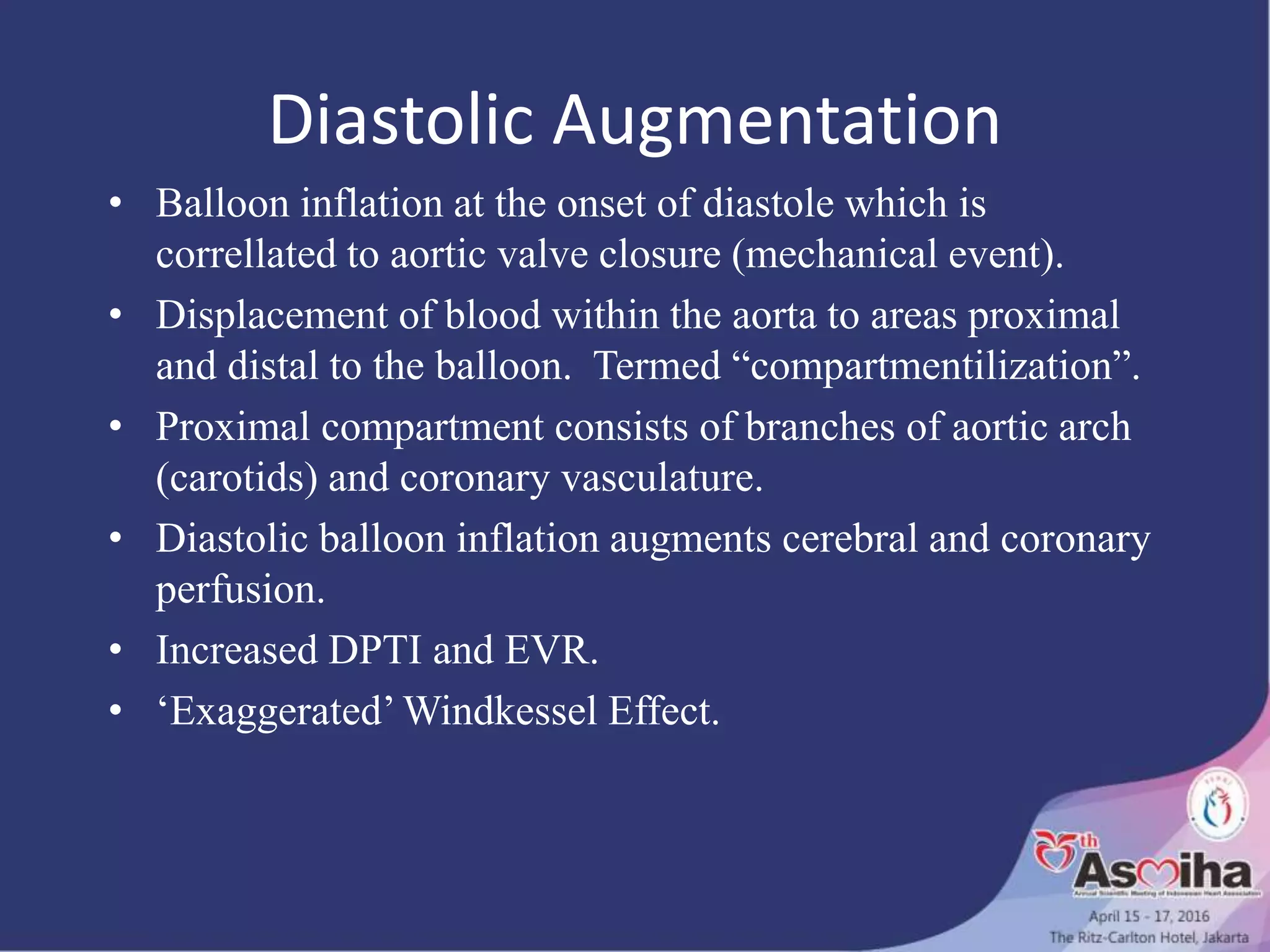
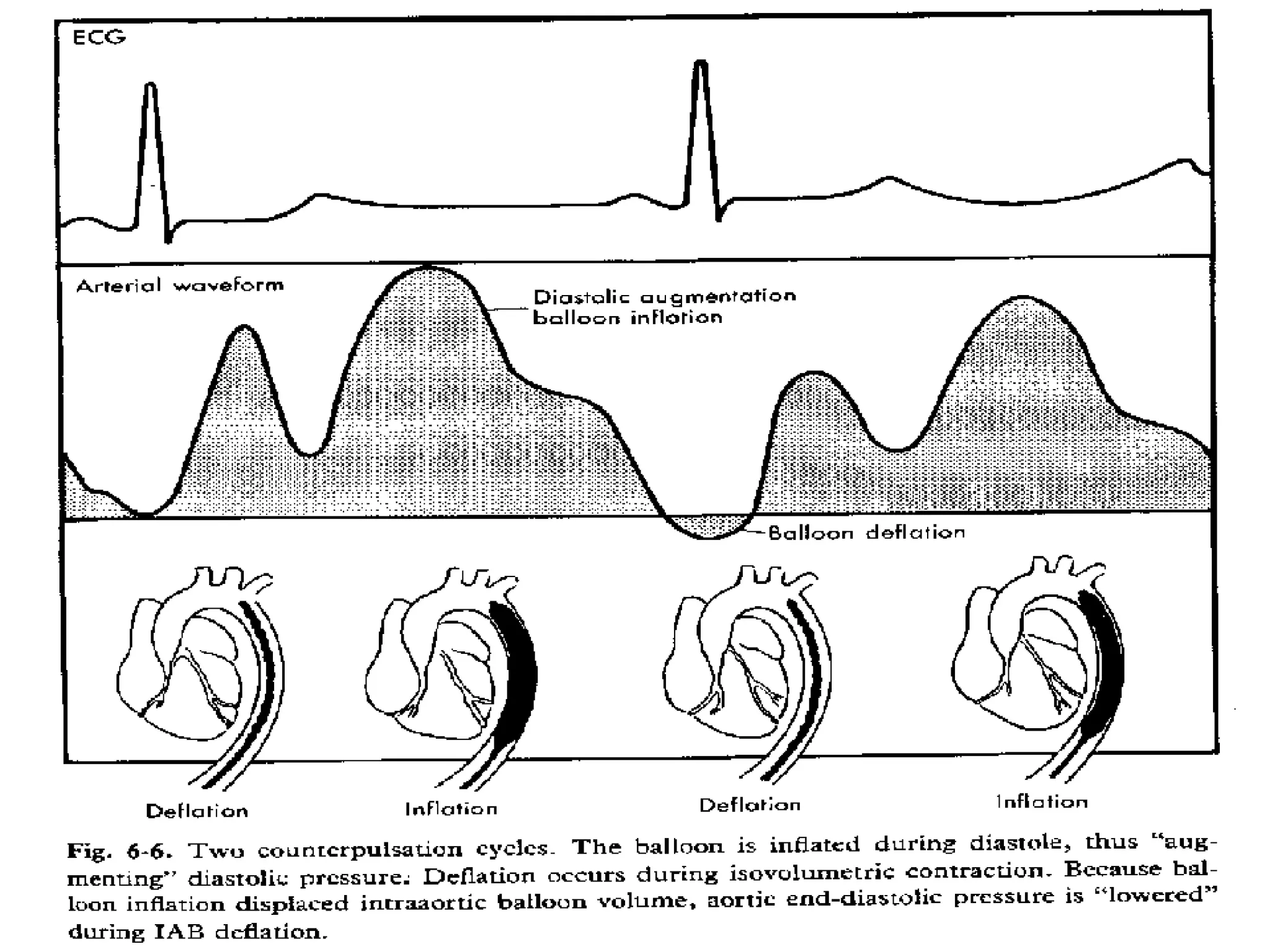
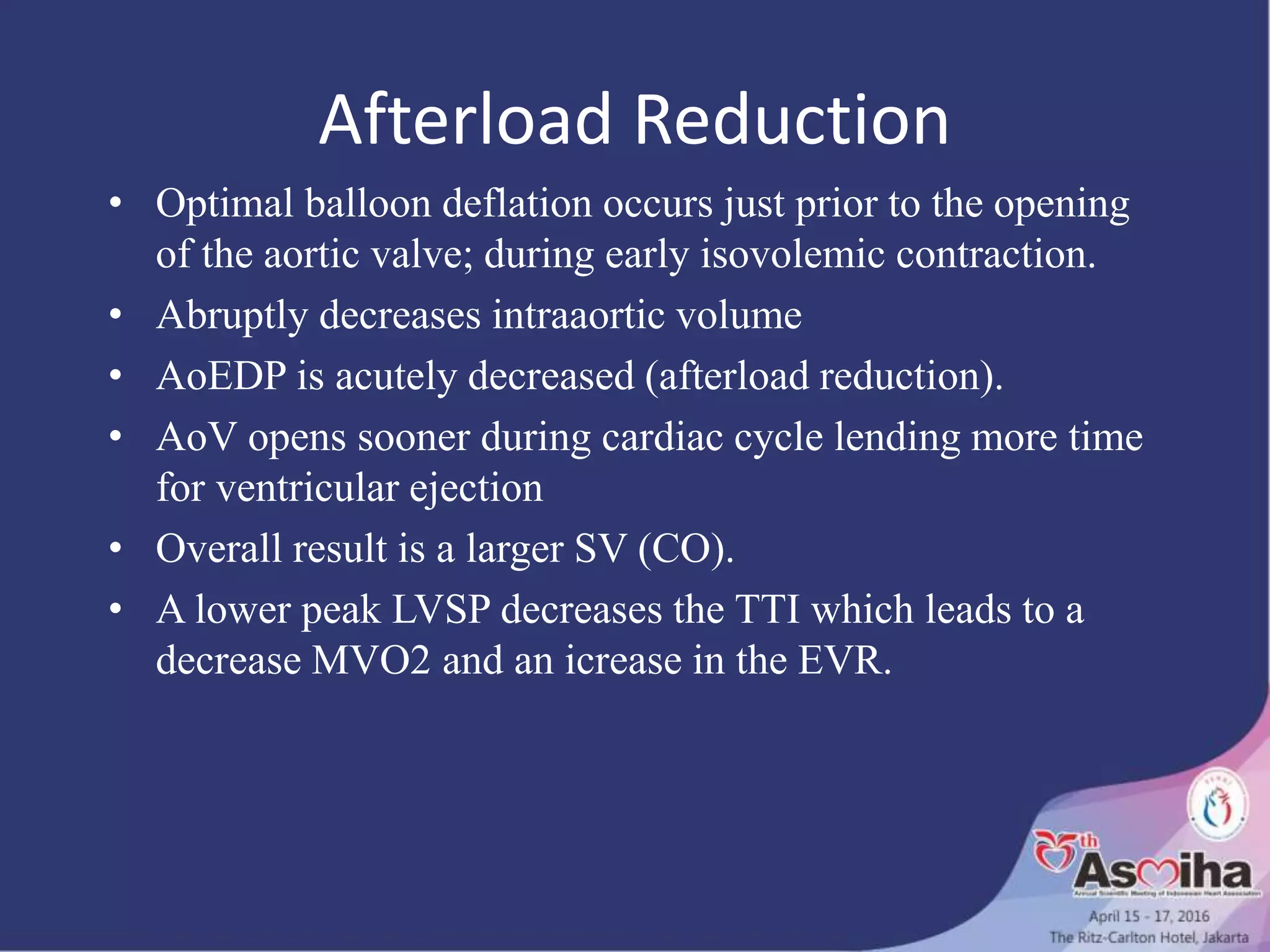
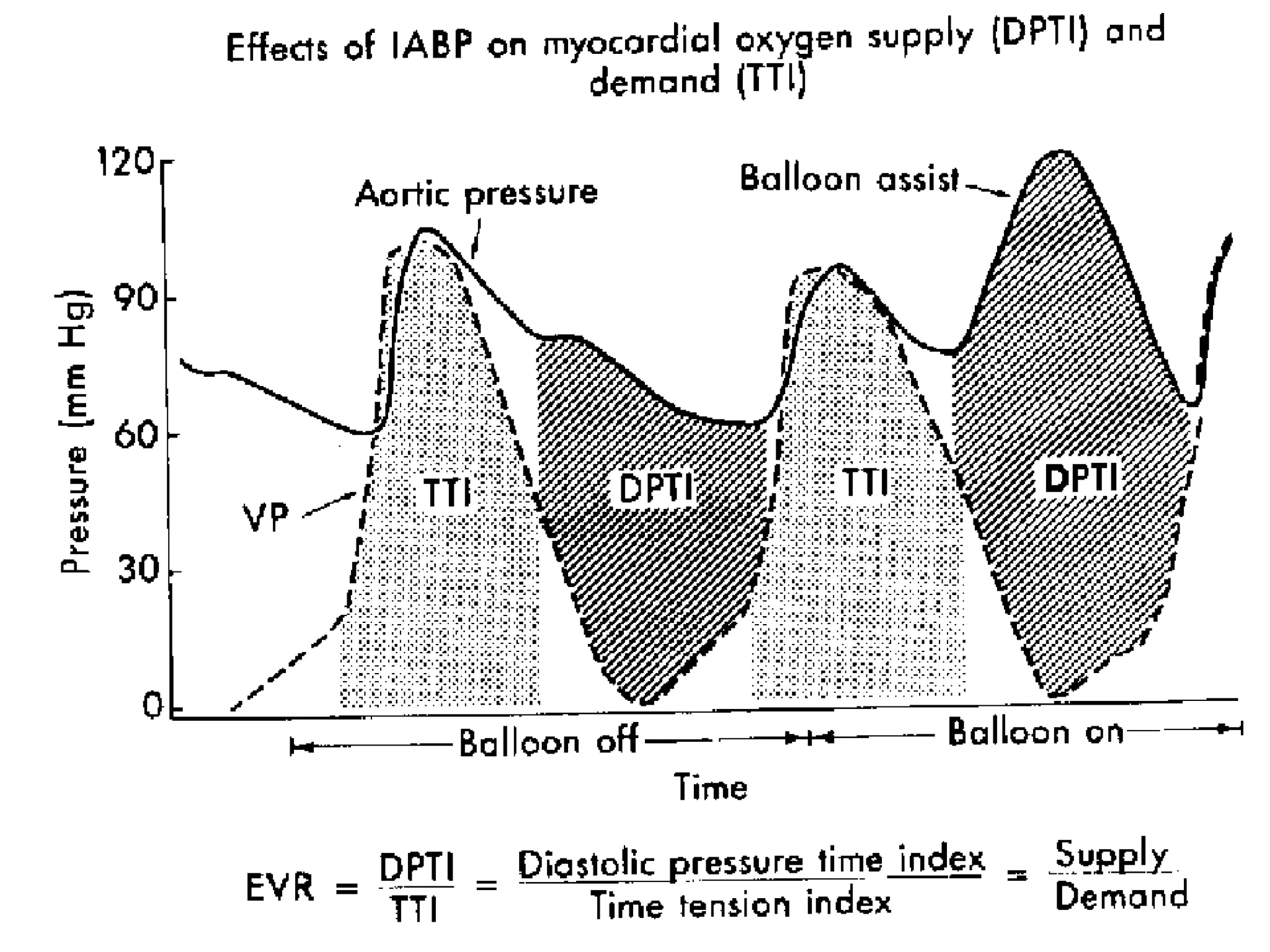
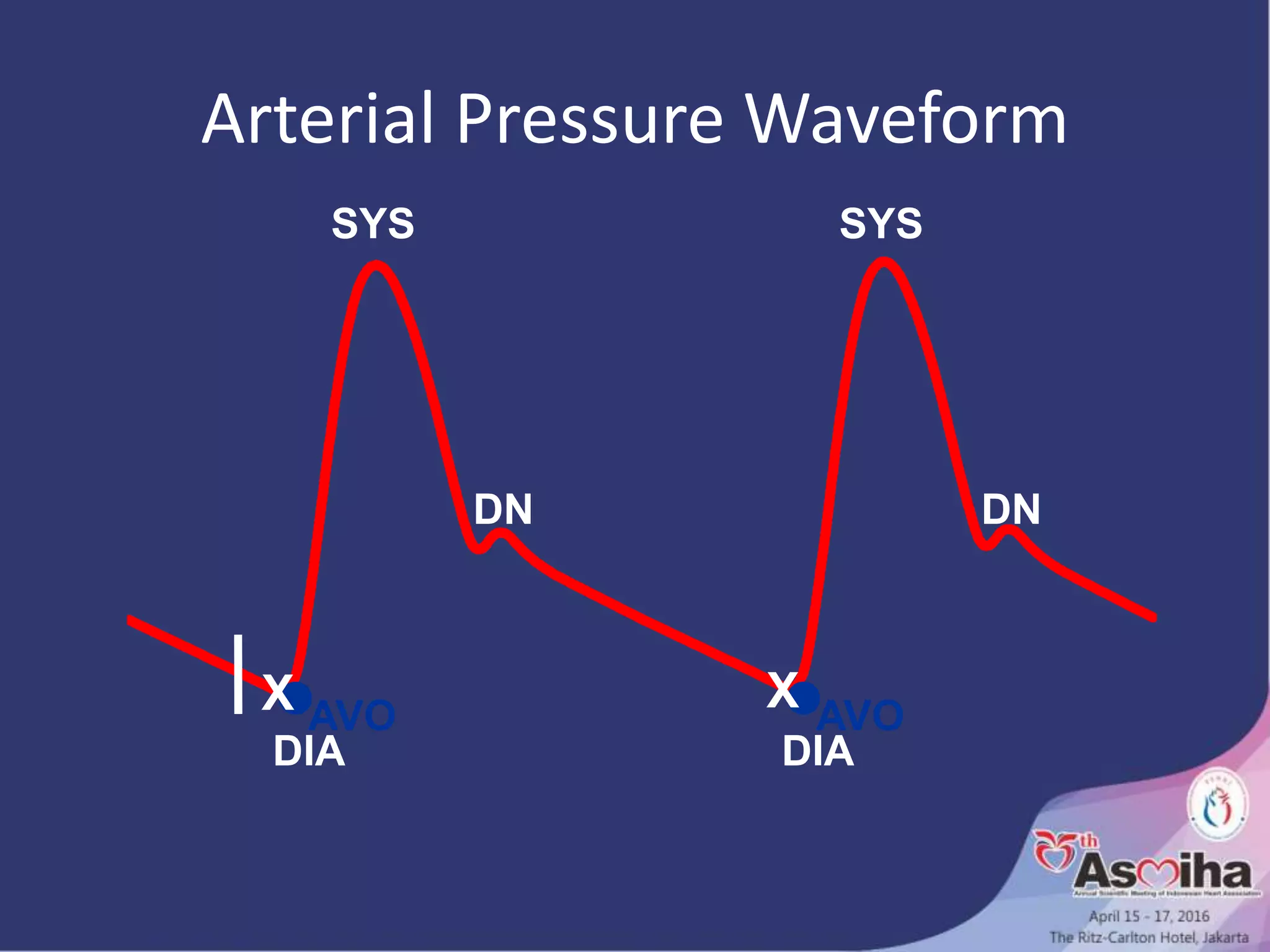
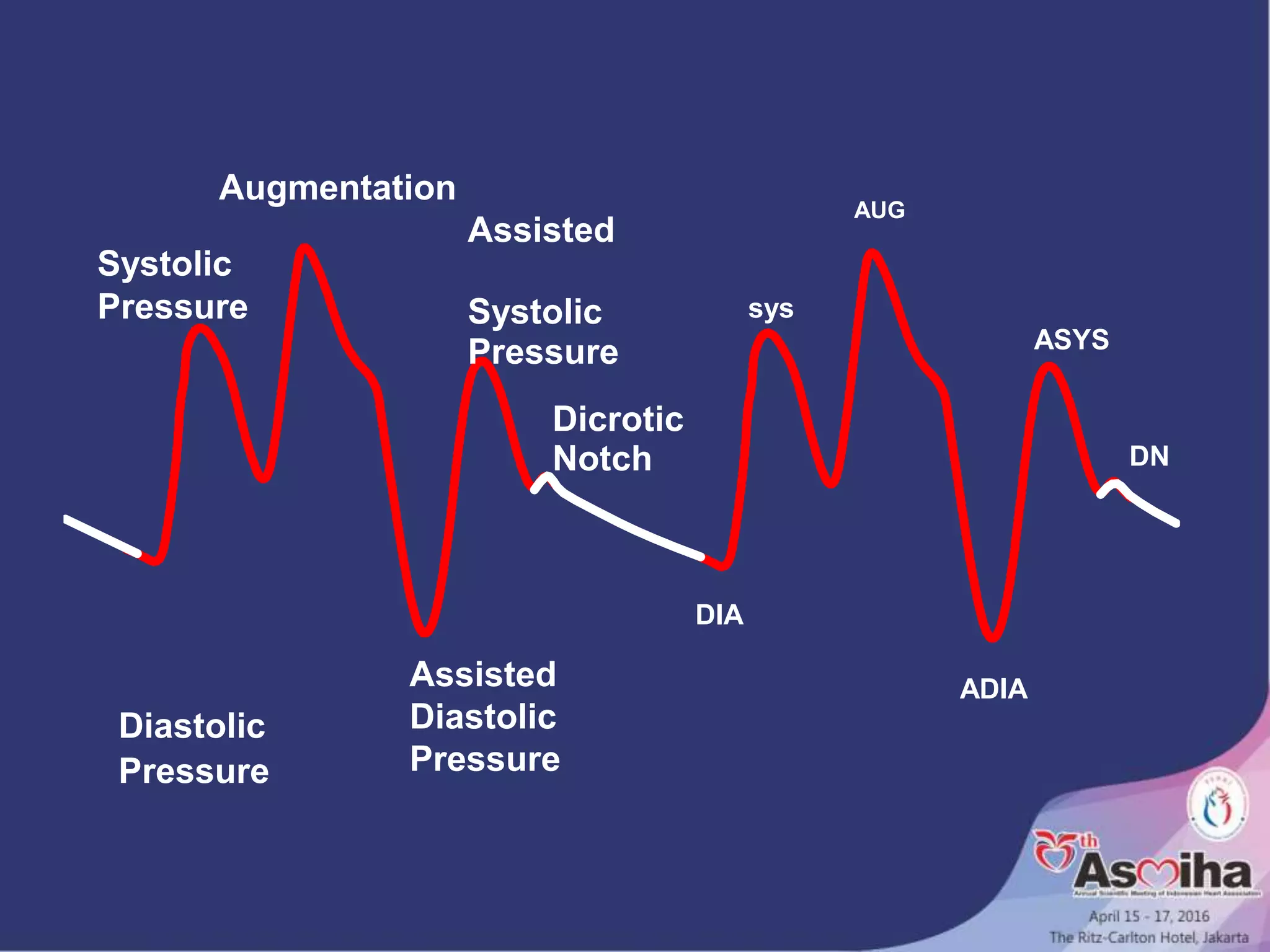
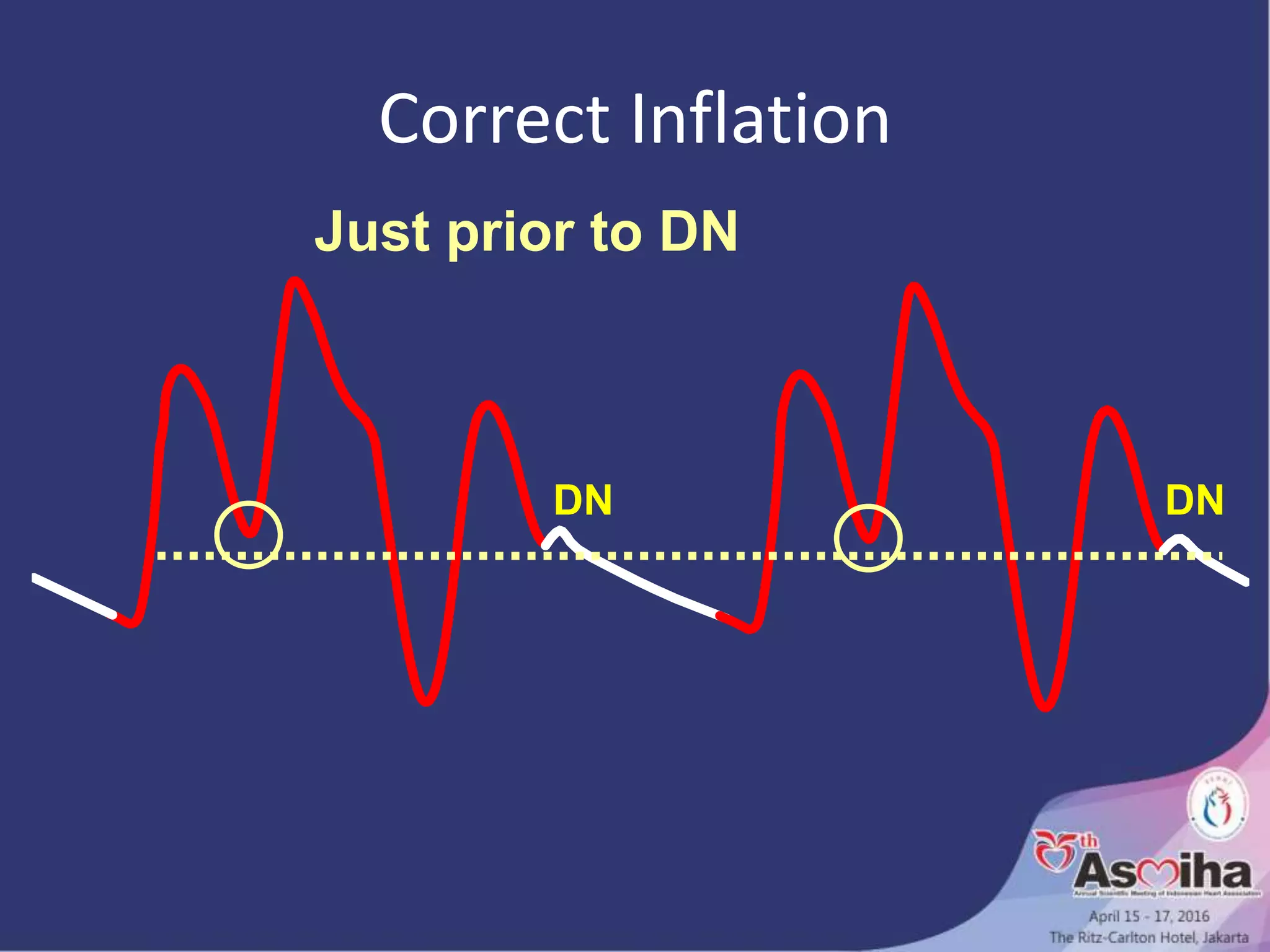
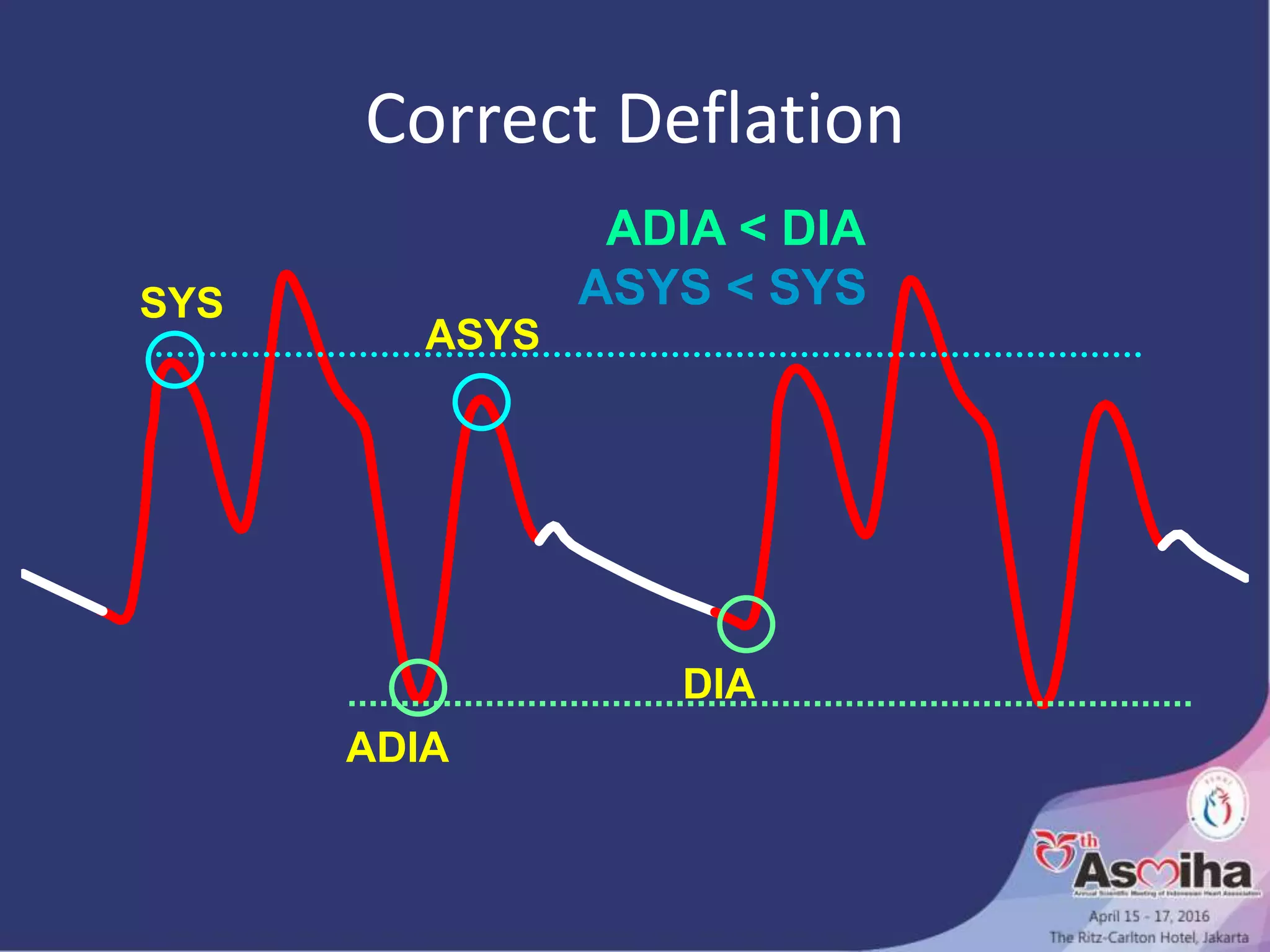
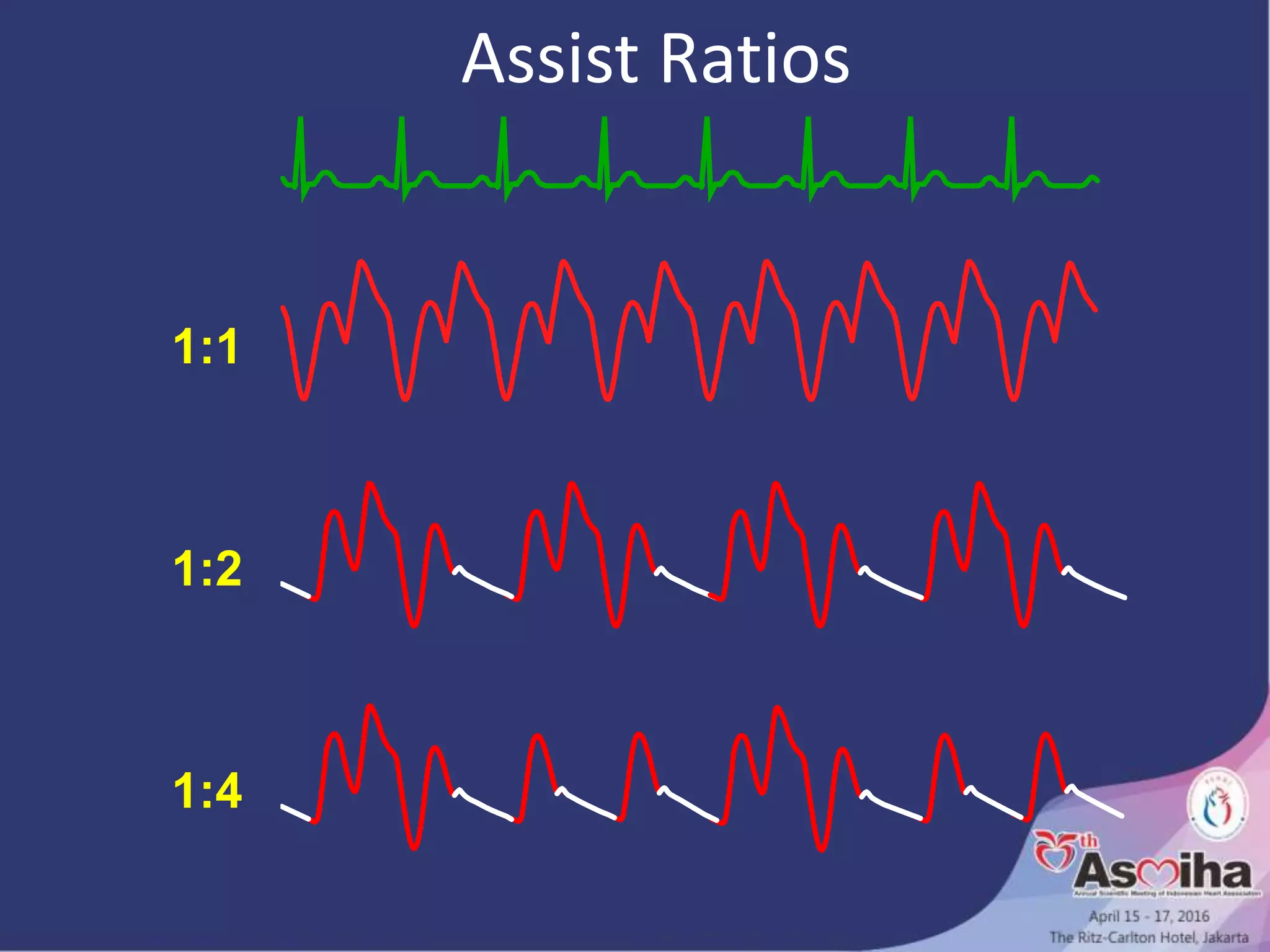
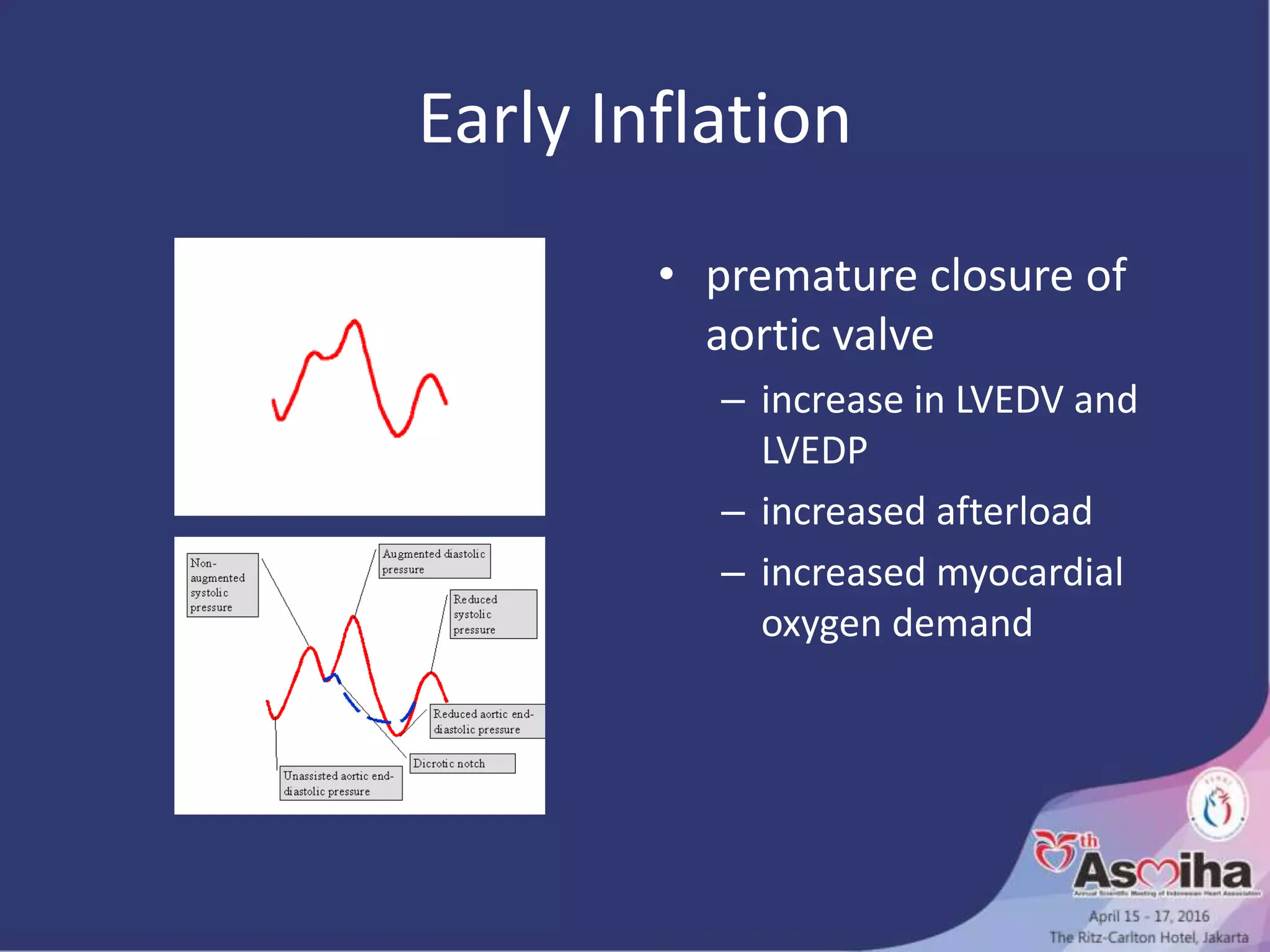
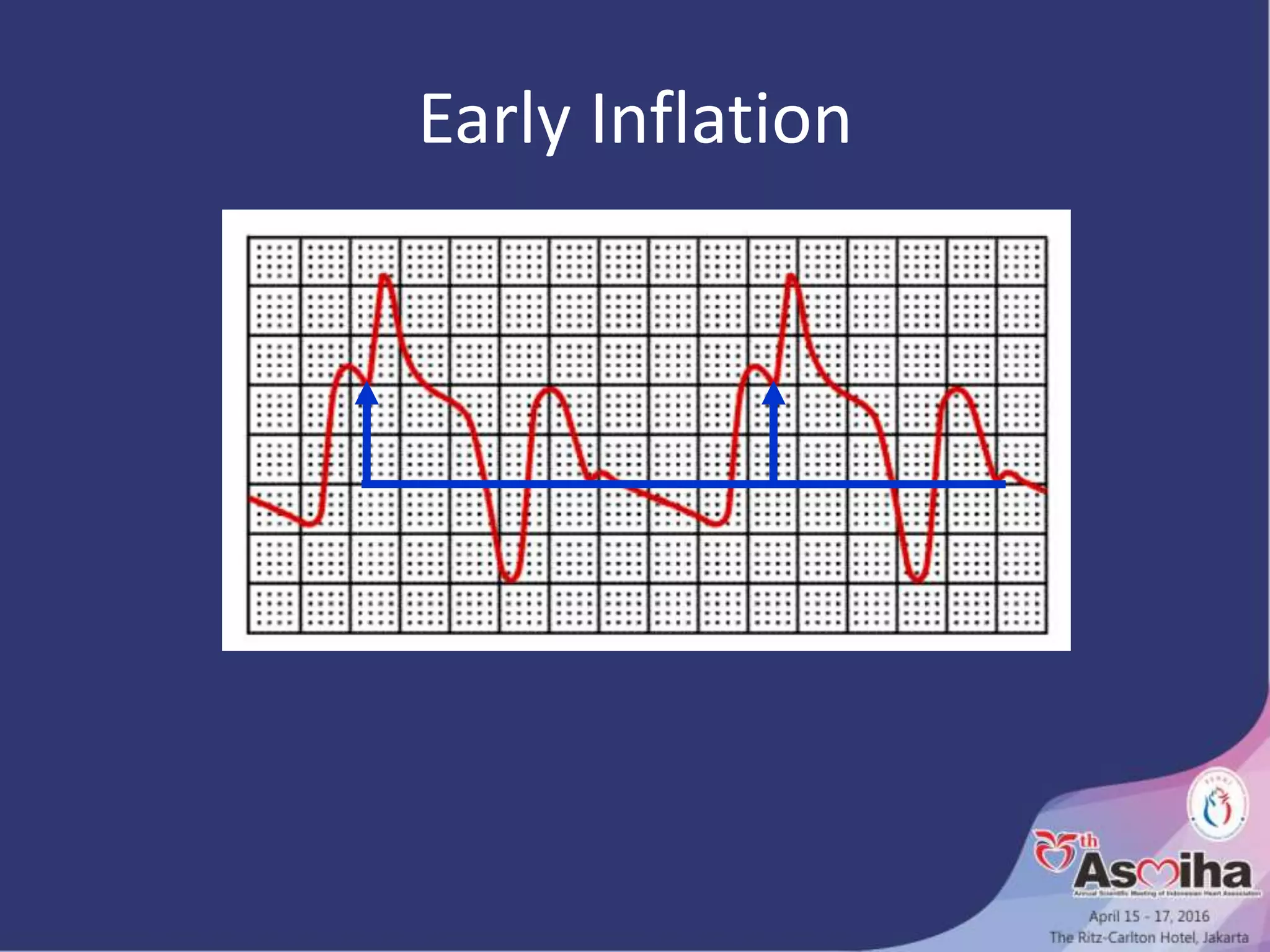
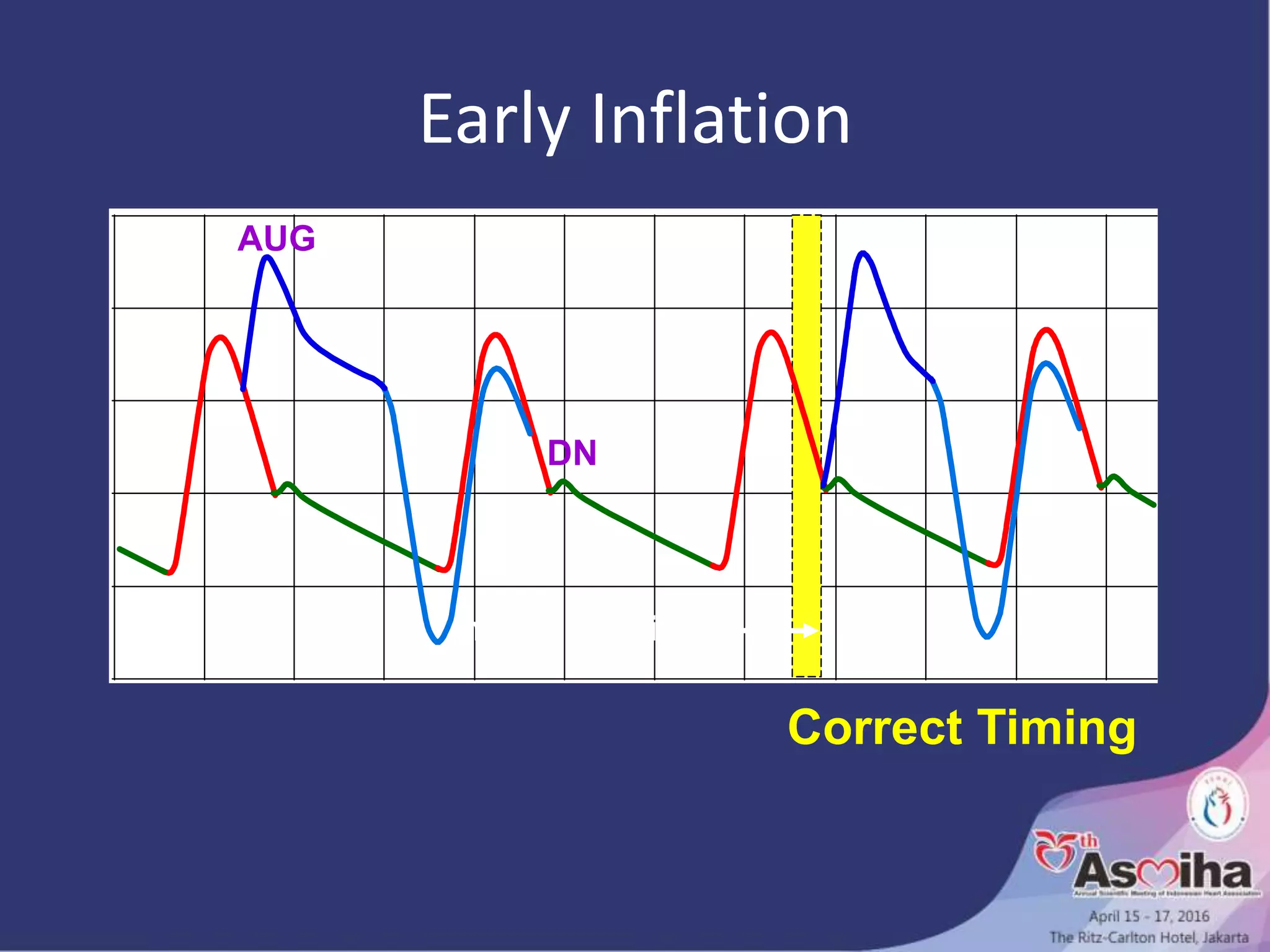
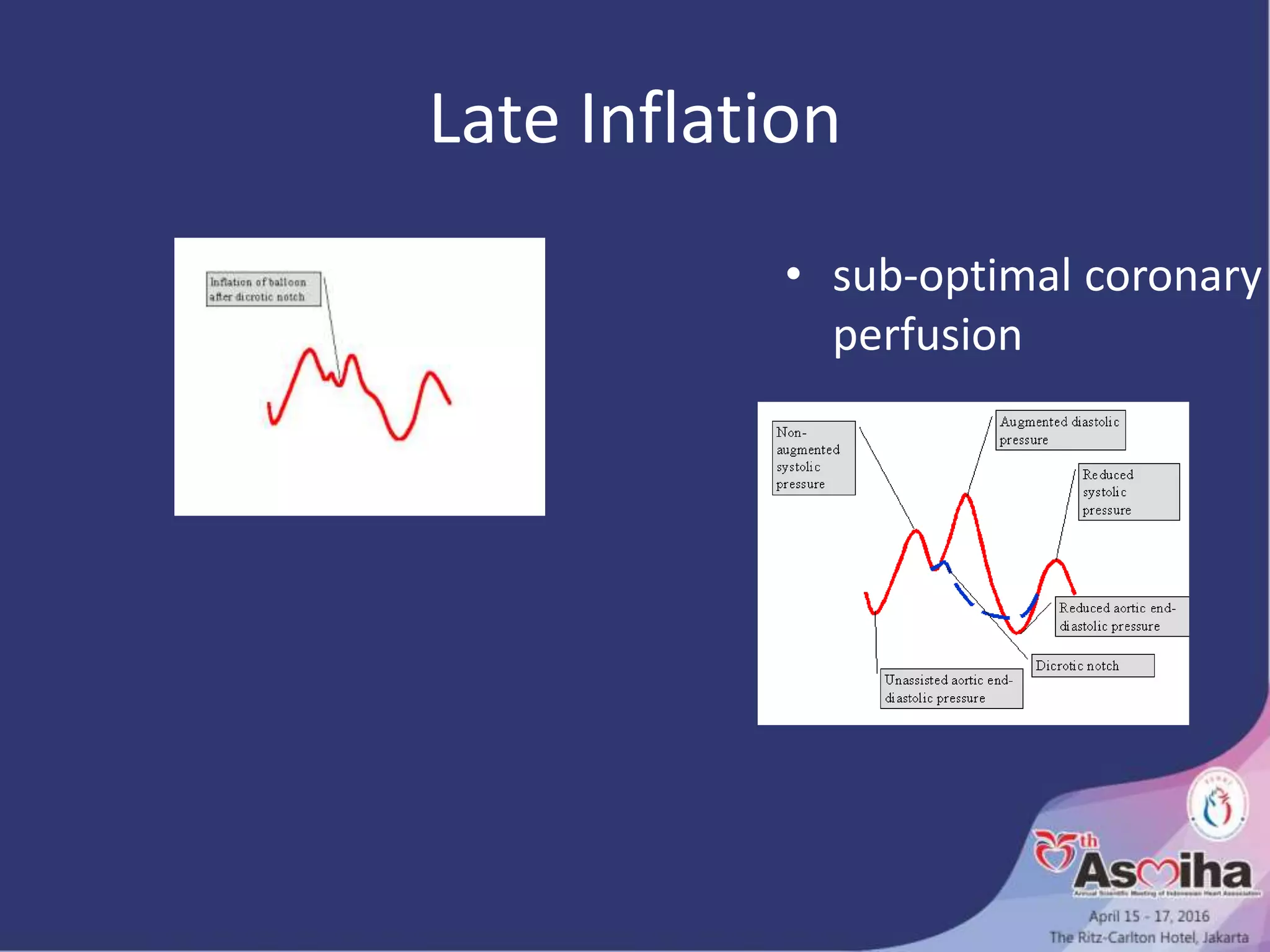
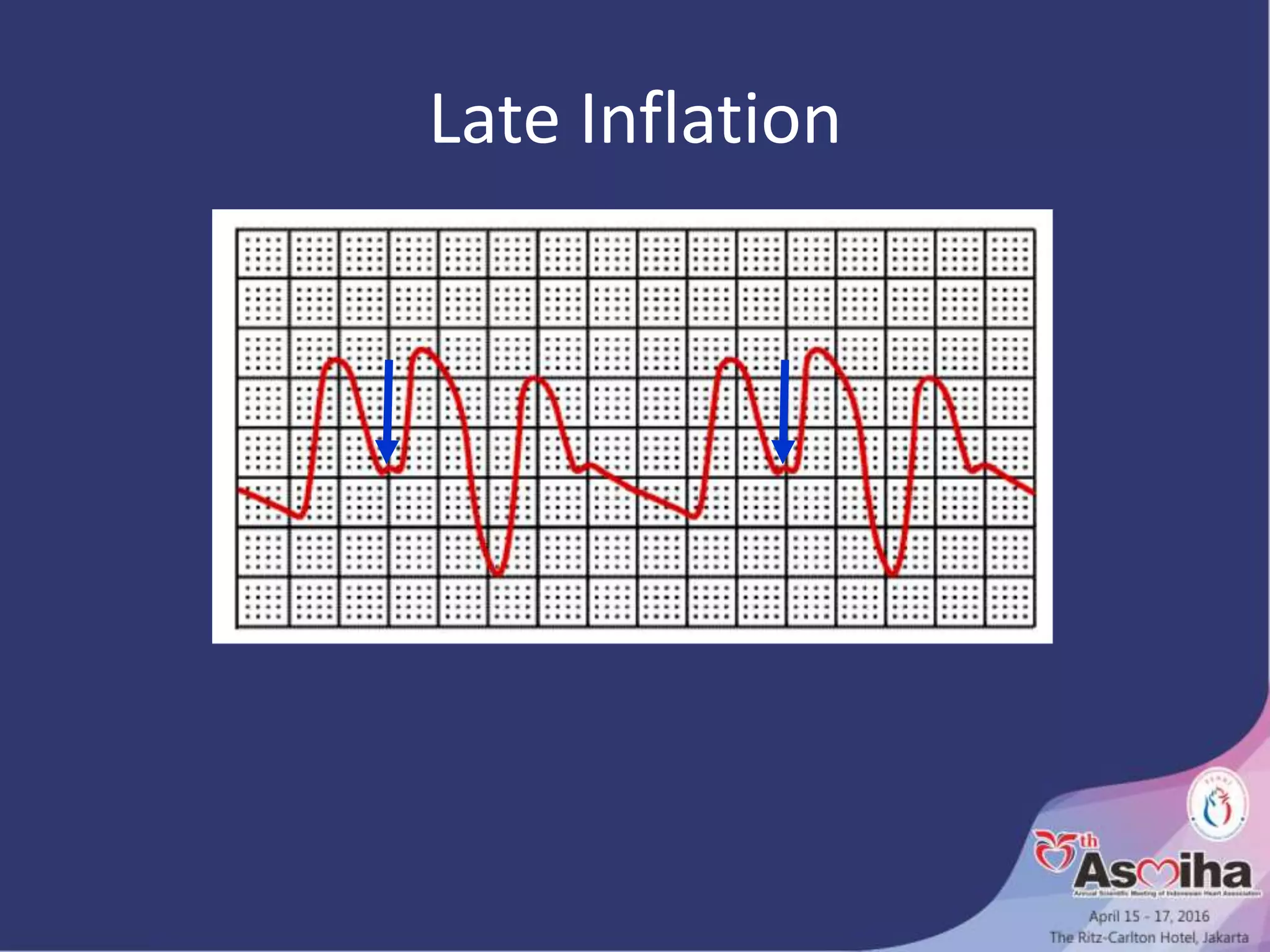
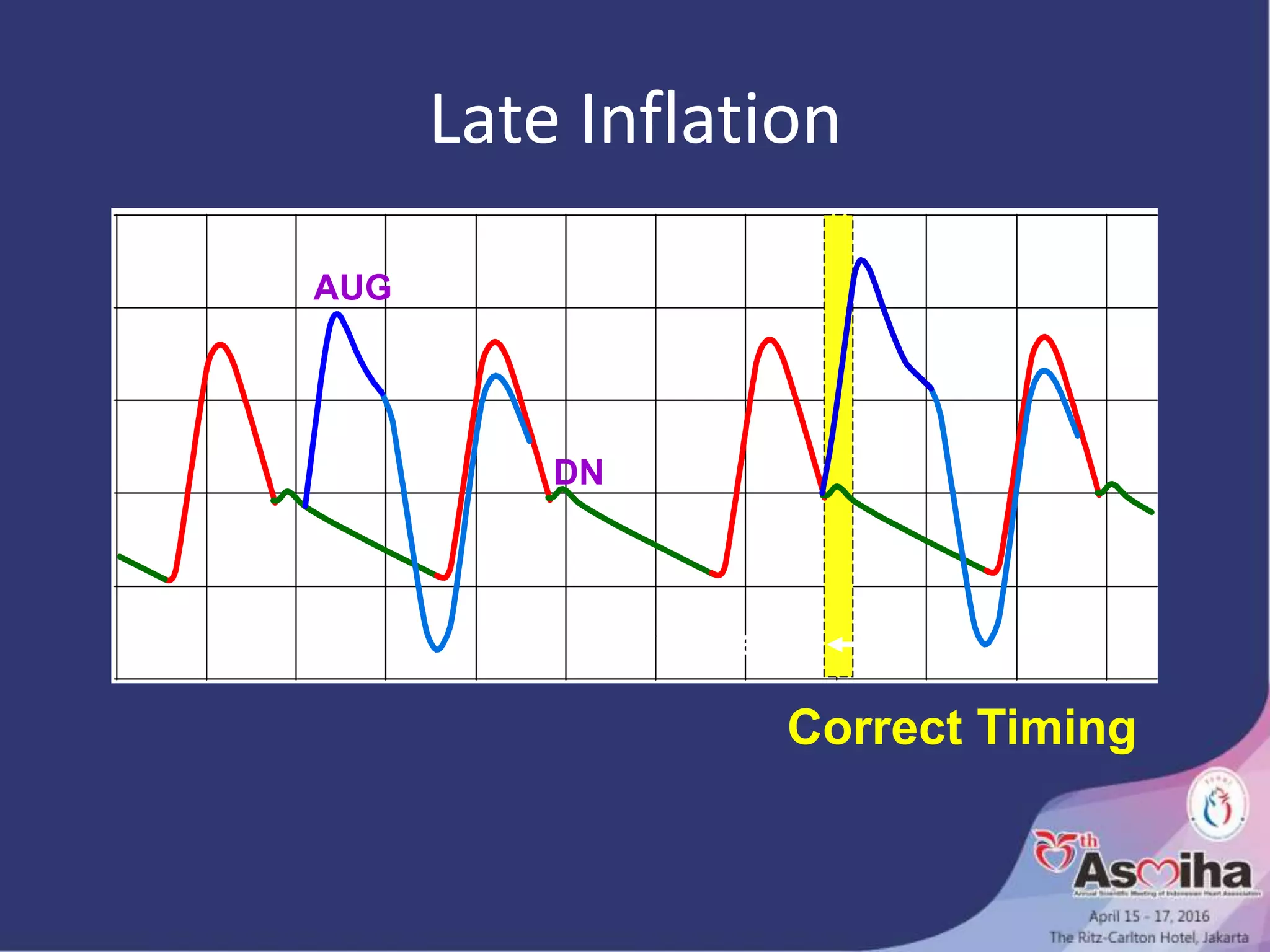
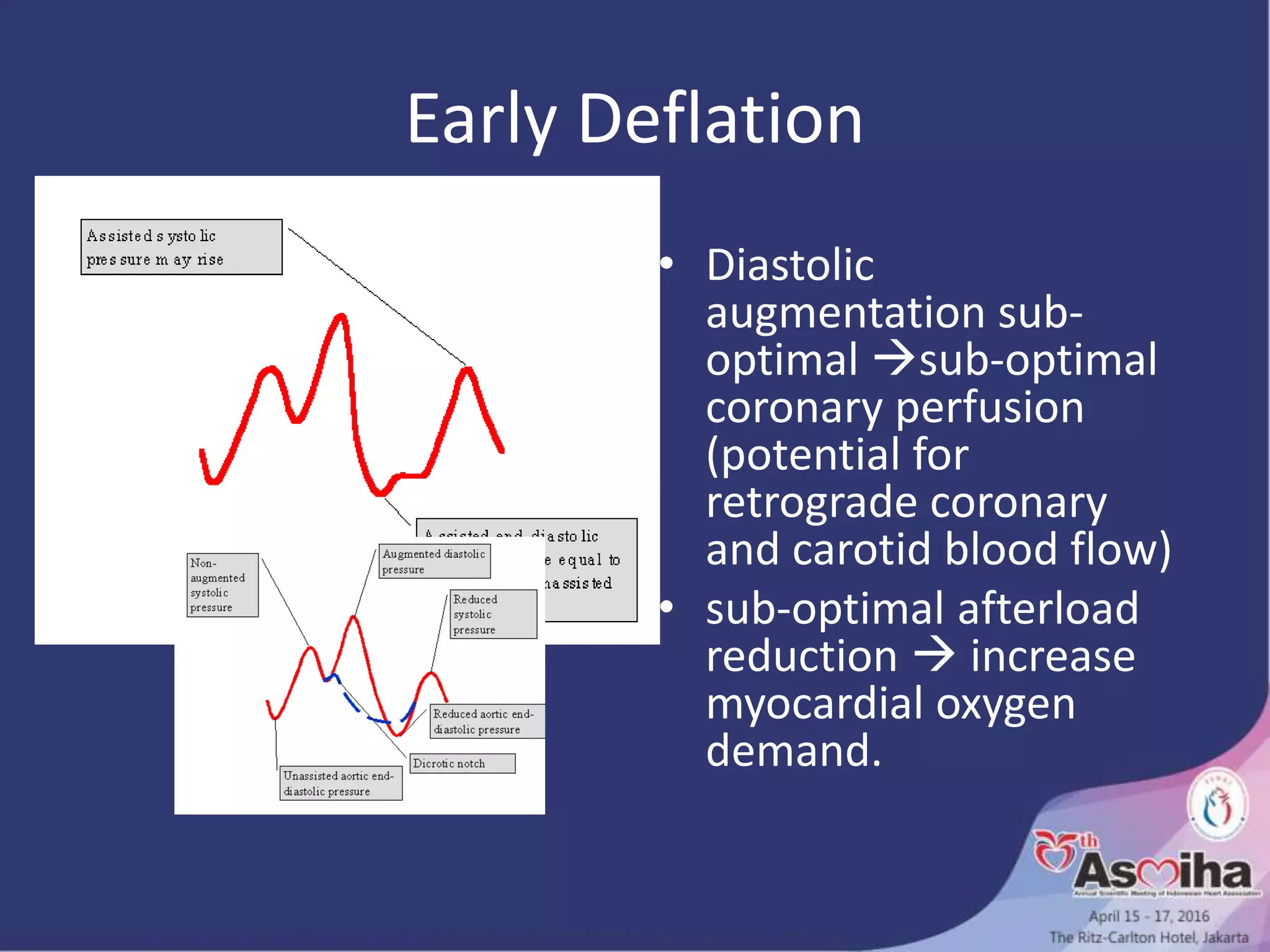
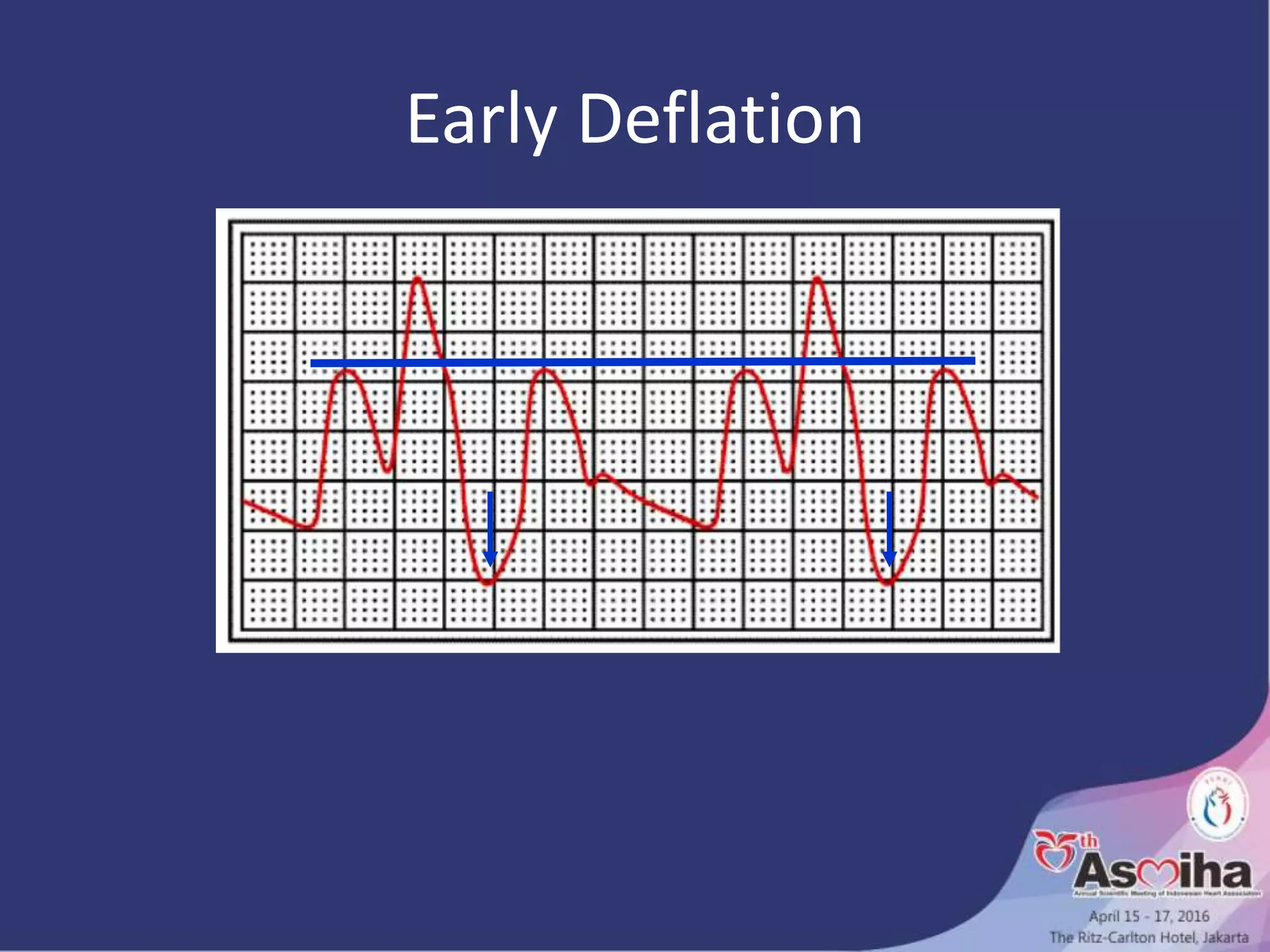
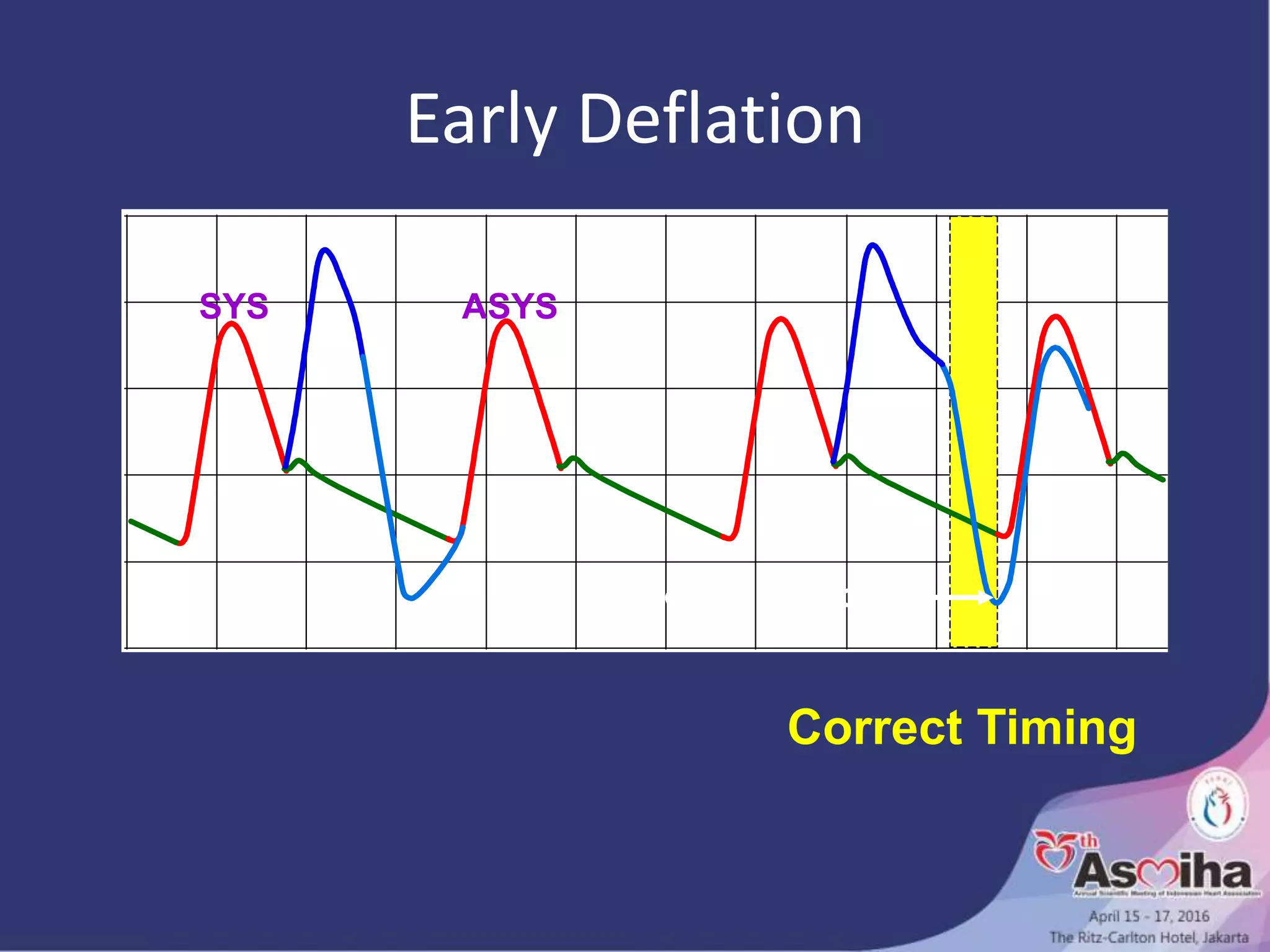
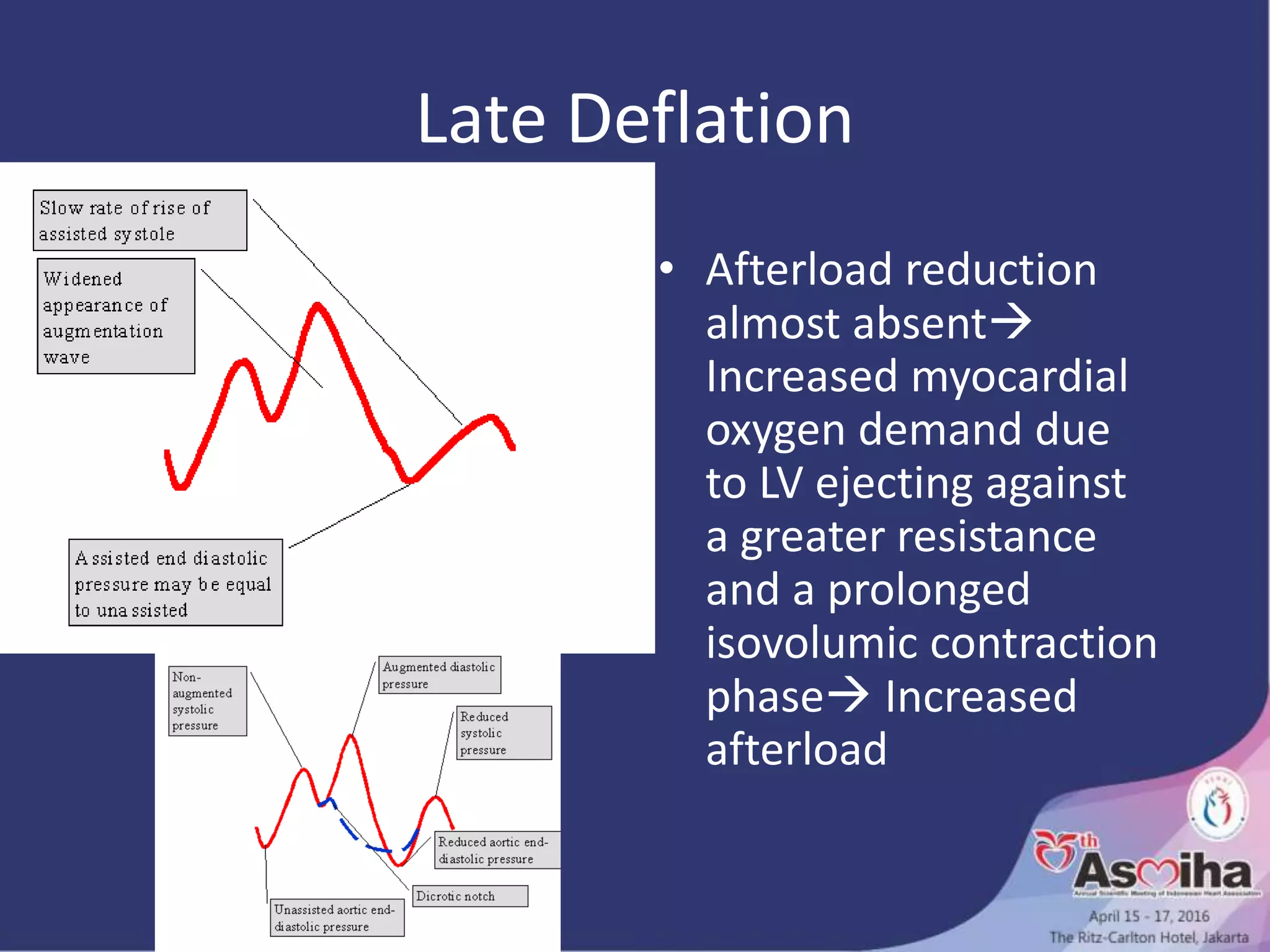
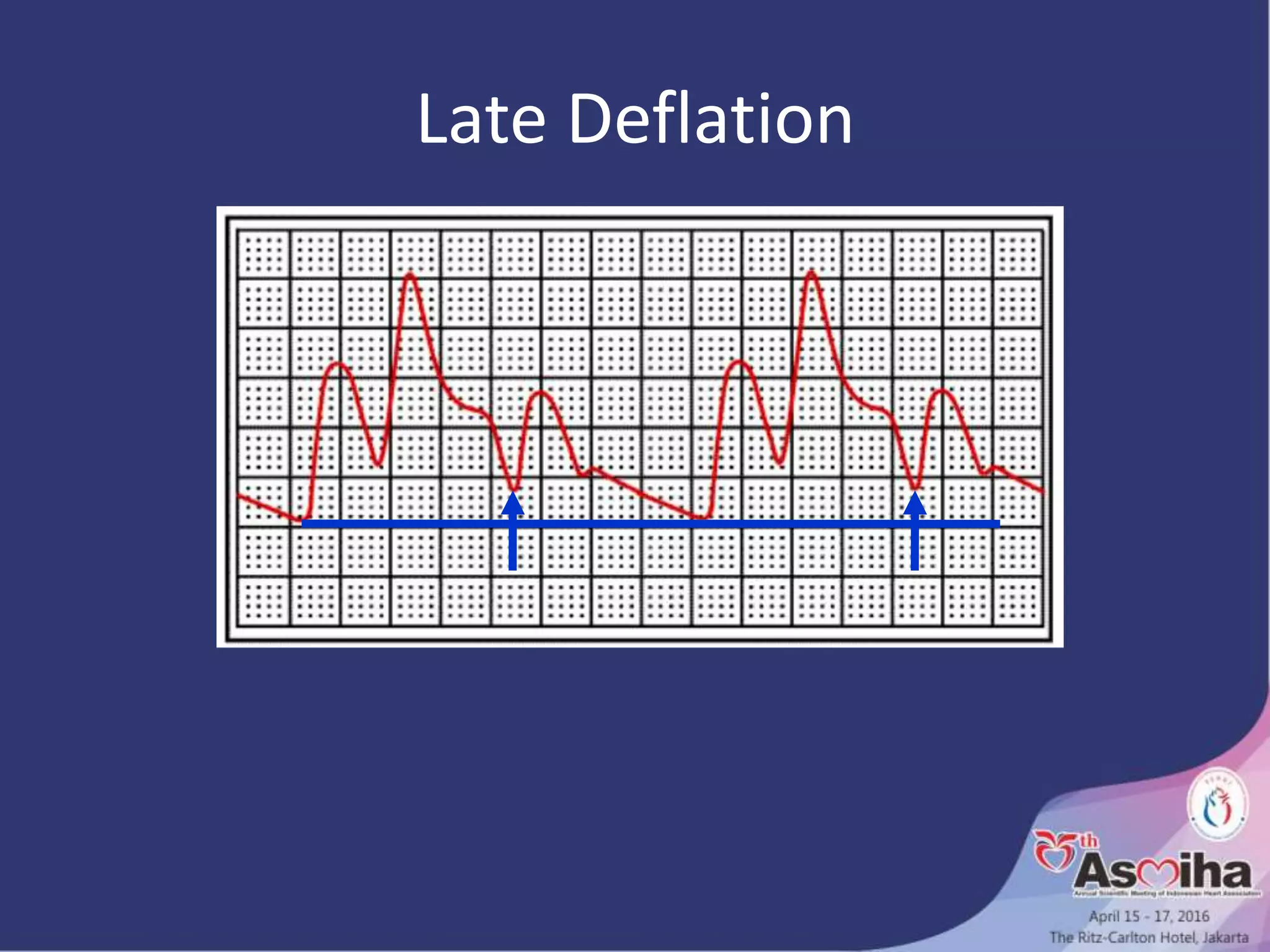
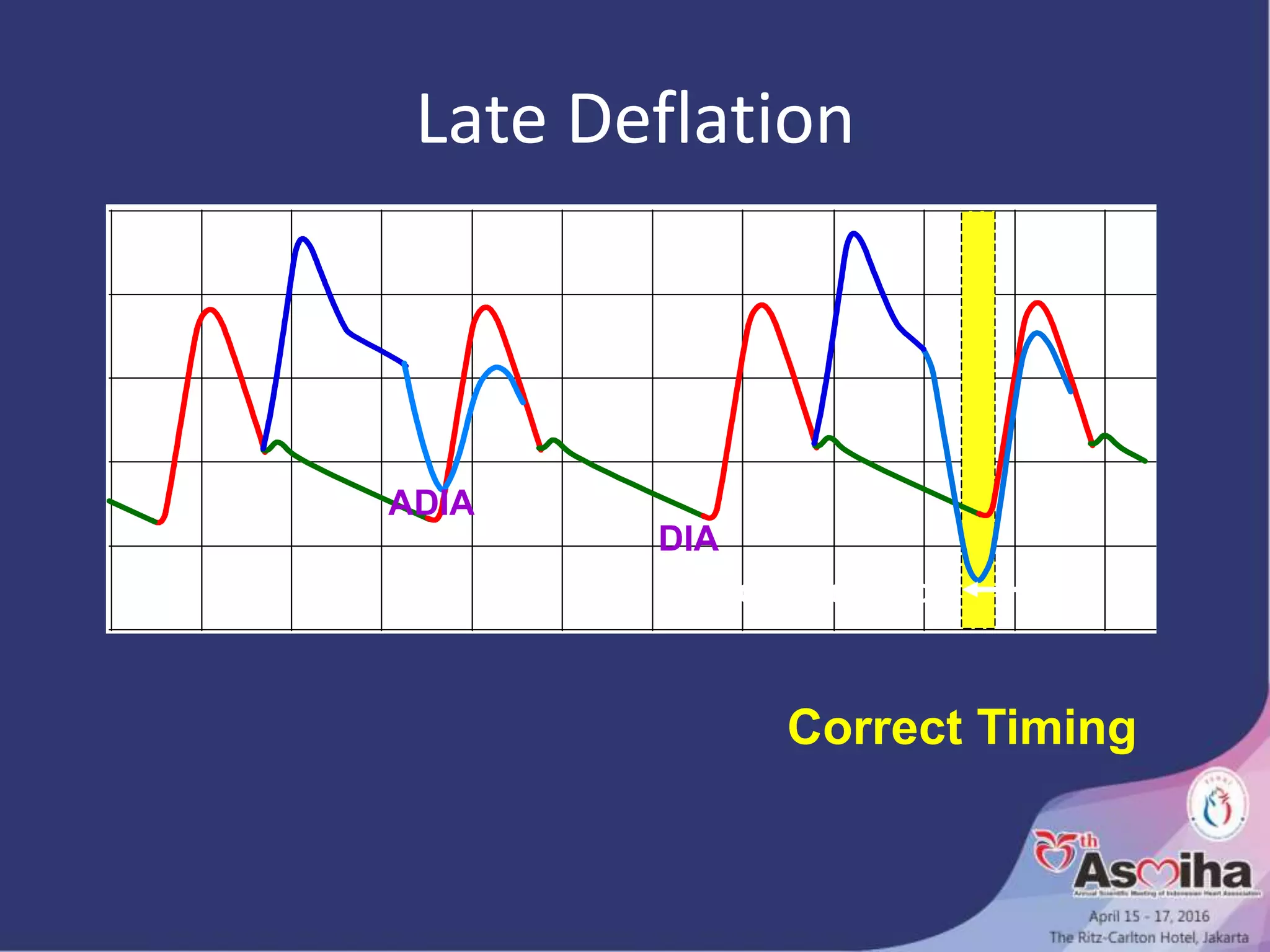
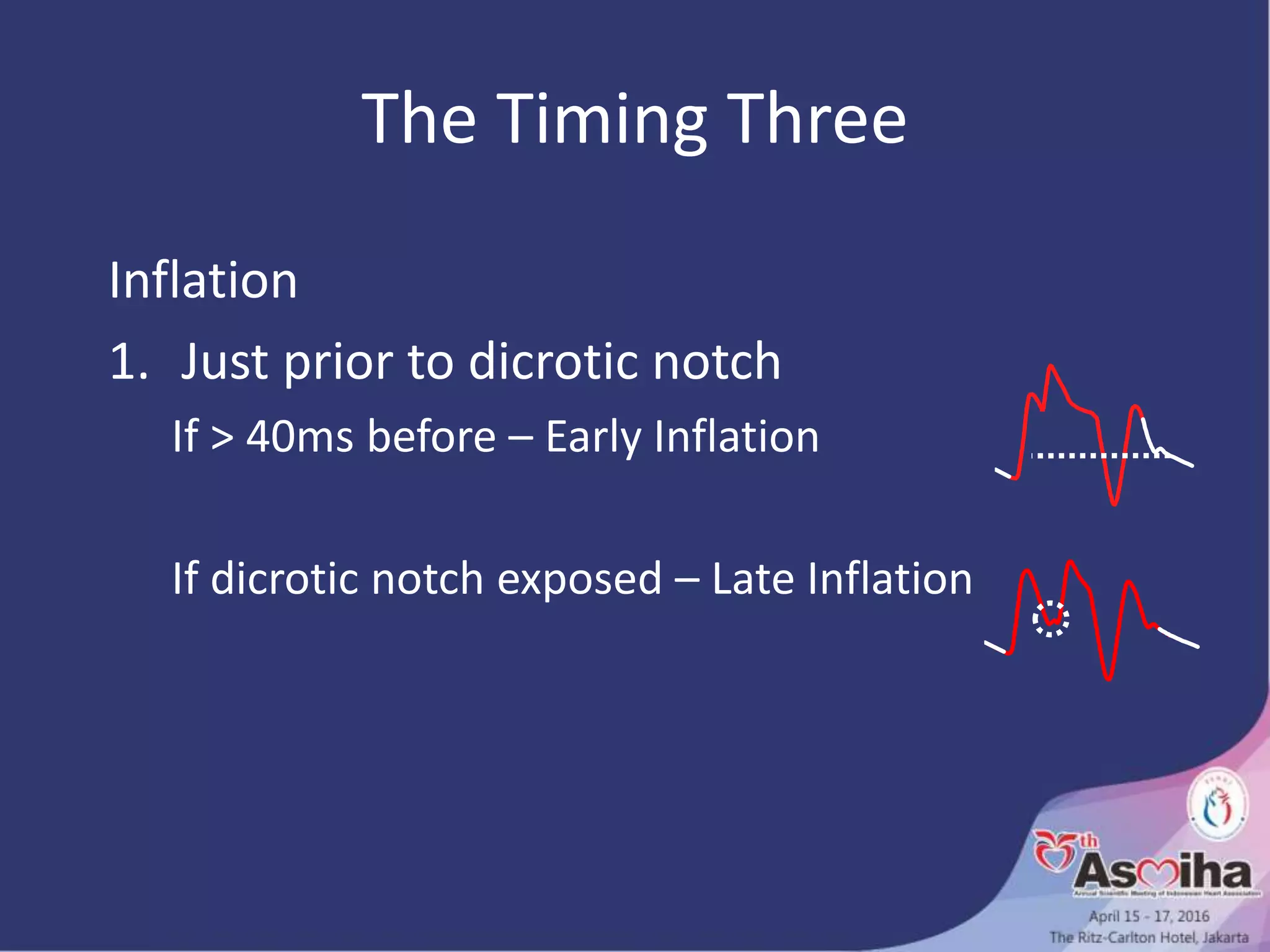
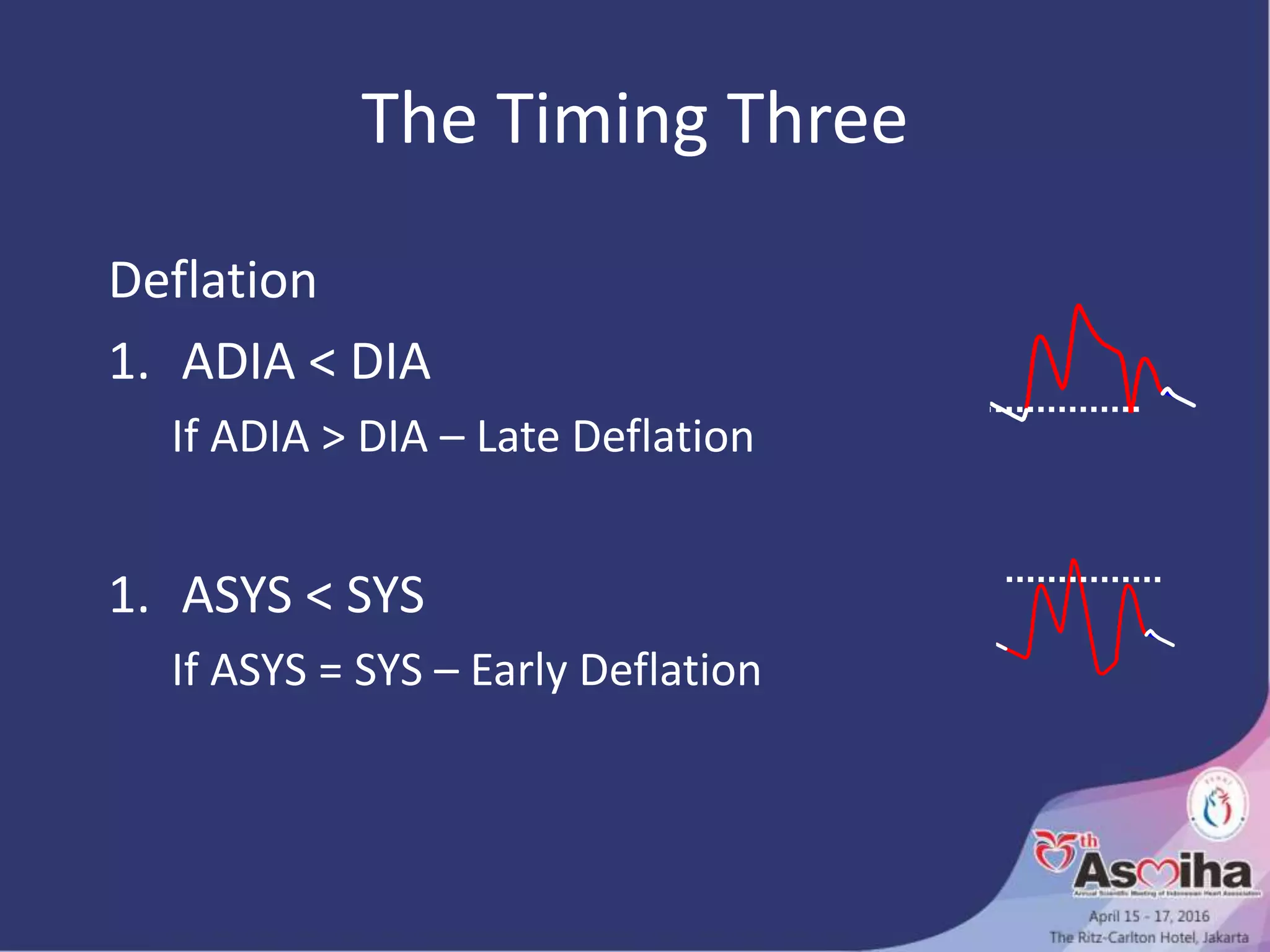
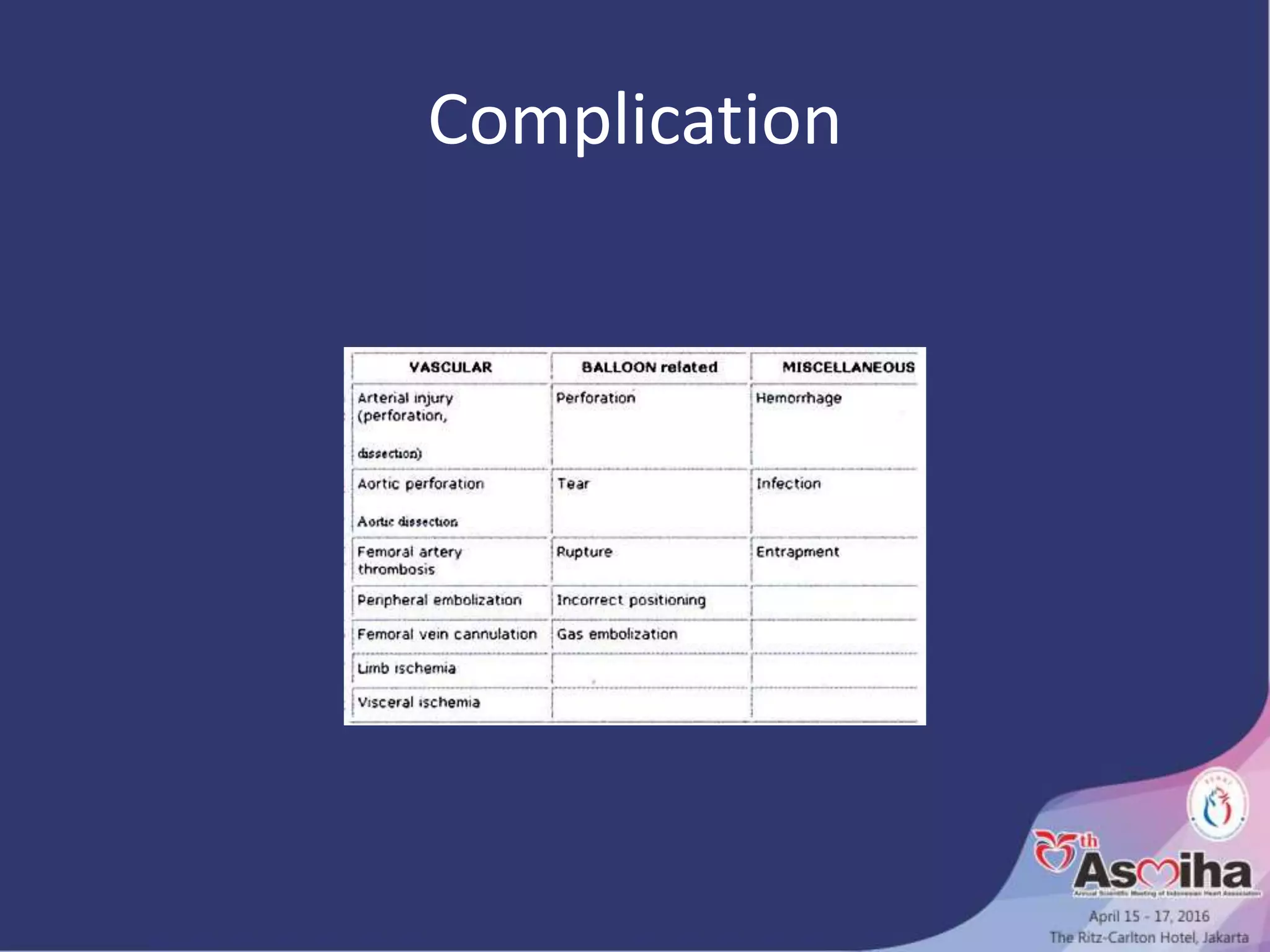
Dr. Isman Firdaus is a critical care and interventional cardiologist affiliated with the National Cardiovascular Center, with multiple prestigious memberships and recognitions in cardiology. The document details the intra-aortic balloon pump (IABP) as a crucial tool for managing hemodynamically unstable patients, covering its workings, determinants of myocardial oxygen delivery, and importance of timing in its application. Additionally, potential complications and guidelines for its use in high-risk procedures are discussed, emphasizing IABP's role in cardiac care.