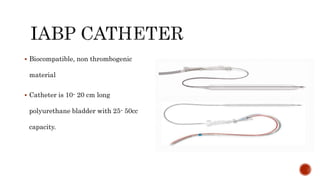
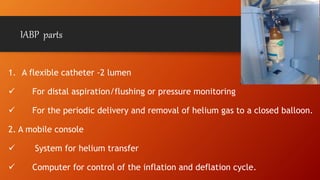
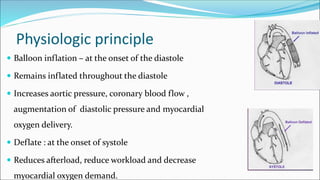
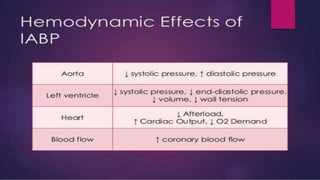
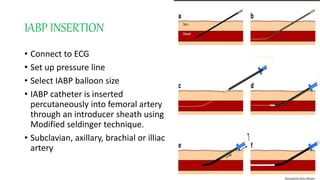
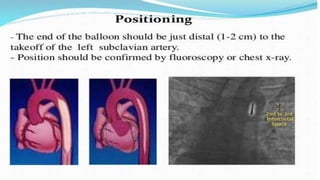
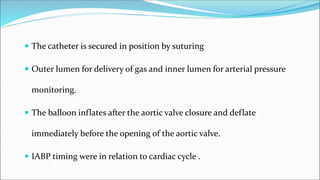
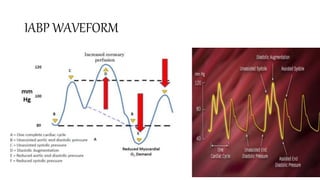
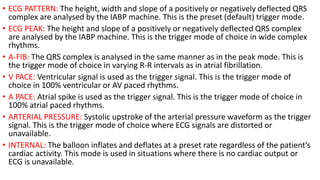
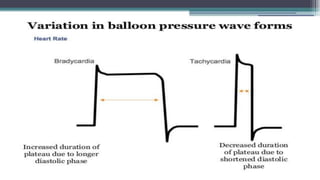
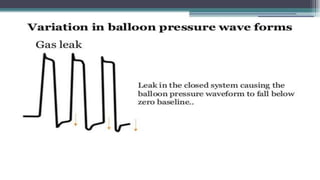
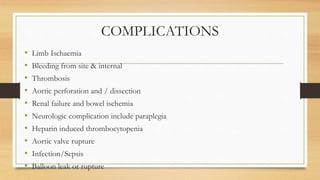
The intra-aortic balloon pump (IABP) is a mechanical device that increases coronary blood flow and reduces cardiac workload by inflating and deflating in sync with the cardiac cycle. It has a flexible catheter inserted into the femoral artery connected to a console that controls helium delivery. The balloon inflates in diastole to boost diastolic pressure and deflates in systole to reduce afterload. This improves cardiac output and oxygen delivery while decreasing oxygen demand. IABP is used in heart failure, unstable angina, cardiogenic shock, and high-risk cardiac procedures as a bridge to recovery or surgery. Nursing care involves monitoring for complications like bleeding, infection and limb ischemia.